
 English
English
 French
French
Allergic rhinitis, upper airway and quality of sleep
Rhinite allergique, voie aerienne supérieure et qualité du sommeil
TD. Ho Viet1, S. Duong-Quy1,2,3, TJ. Craig2
1: Lam Dong Medical College, 16 Ngo Quyen. Da Lat, Viet Nam
2: Penn State University. 500 University Drive, Hershey, PA, USA
3: Paris Descartes University, France
Corresponding author
Dr. Thuy Duong HO VIET
Lam Dong Medical College. Dalat, Vietnam
Email: drthuyviet@gmail.com
DOI: 10.12699/jfvp.8.24.2017.3
ABSTRACT
The symptoms of allergic rhinitis (AR) include rhinorrhea, nasal pruritus and sneezing, and nasal congestion. AR is usually associated with the allergic symptoms of another organs such as the eyes and throat. Nasal congestion stands as one of the most prominent and bothersome symptoms of the disorder, especially since it is linked to sleep-related problems associated with allergic rhinitis, such as sleep-disordered breathing, including snoring and sleep apnea. Patients with allergic rhinitis, one of several inflammatory disorders of the upper respiratory tract, often suffer from impaired sleep. A recent survey of allergic rhinitis patients revealed that 68% of respondents with perennial allergic rhinitis (PAR) and 48% with seasonal allergic rhinitis (SAR) reported that their condition caused significant sleep disturbances. One of the major symptoms of the disorder, nasal congestion, and also mediators of the underlying inflammatory reaction and other allergic symptoms such as ocular pruritus, can cause the sleep impairment associated with allergic rhinitis and the daytime somnolence and fatigue. The quality of life in patients with allergic rhinitis is detrimentally impacted by the sleep impairment associated with the disorder. One of the key causes leading to sleep disruptions and sleep-disordered breathing is nasal congestion, one of the most common and bothersome symptoms of allergic rhinitis.
KEYWORDS: Rhinitis, nasal congestion, sleep, sleep disordered, airway resistance.
RÉSUMÉ
Les symptômes de la rhinite allergique (RA) comprennent la rhinorrhée, le prurit nasal et les éternuements, ainsi que la congestion nasale. L'RA est généralement associée aux symptômes allergiques d'autres organes tels que les yeux et la gorge. La congestion nasale est l'un des symptômes les plus importants et gênants du trouble, d'autant plus qu'il est lié à des problèmes de sommeil associés à la rhinite allergique, tels que la respiration désordonnée du sommeil, y compris le ronflement et l'apnée du sommeil. Les patients souffrant de rhinite allergique, l'un des troubles inflammatoires des voies respiratoires supérieures, souffrent souvent de troubles du sommeil. Une enquête récente auprès de patients atteints de rhinite allergique a révélé que 68% des répondants souffrant de rhinite allergique perannuelle (RAP) et 48% de rhinite allergique saisonnière (RAS) ont signalé que leur état causait d'importantes perturbations du sommeil. L'un des principaux symptômes de la maladie, la congestion nasale, ainsi que les médiateurs de la réaction inflammatoire sous-jacente et d'autres symptômes allergiques tels que le prurit oculaire, peuvent causer l'insomnie associée à la rhinite allergique et la somnolence et la fatigue. La qualité de vie des patients atteints de rhinite allergique est affectée de manière préjudiciable par les troubles du sommeil associés à cette pathologie. La congestion nasale, l'un des symptômes le plus commun et le plus gênant de la rhinite allergique, est l'une des principales causes des troubles respiratoires au sommeil et de la qualité du sommeil.
MOTS CLÉS: Rhinite, congestion nasale, sommeil, trouble du sommeil, résistance de voie aérienne.
INTRODUCTION
The symptoms of allergic rhinitis (AR) include rhinorrhea, nasal pruritus and sneezing, and nasal congestion. AR is usually associated with the allergic symptoms of another organs such as the eyes and throat. Nasal congestion stands as one of the most prominent and bothersome symptoms of the disorder, especially since it is linked to sleep-related problems associated with allergic rhinitis, such as sleepdisordered breathing, including snoring and sleep apnea [1,2].
The prevalence of inflammatory disorders of the upper respiratory tract make the sleep impairment associated with many of these disorders a common problem. Allergic rhinitis alone reportedly affects approximately 25% of the world’s population, and its prevalence has continued to climb [3]. It has been estimated that the disorder affects 20 to 40 million people in the United States, which includes approximately 40% of the nation’s children. In Europe, the prevalence of allergic rhinitis is estimated as 23% of the population [4,5].
MECHANISMS OF DISORDERED SLEEP IN RHINITIS
Rhinitis no doubt effects sleep, but the exact mechanism or mechanisms that attribute to the decrement of sleep is still under debate and research. Nasal congestion alone can result in an increase in apneahyponea index (AHI) and early studies using nasal occlusion resulted in disordered sleep and daytime somnolence symptoms have been under investigation [6-8]. In addition, tonal changes to the upper airway muscles and upper airway collapse secondary to hypotonic muscles has gathered much attention [9,10].
Anatomic upper airway, pharyngeal collapse and the role of the nose. The upper airway at the oral and nasal openings, and has a complex geometry. The major respiratory function of the upper airway is to allow air exchange, humidification of the air and removal of pathogens, particles, allergens and irritants. Airflow through the nose, pharynx and larynx to the extrathoracic trachea is responsible for the majority of airway resistance during breathing. The upper airway is responsible for 40-70% the total pulmonary resistance during breathing [2,9,10]. In the patient with OSAS, upper airway resistance can increase negative pressure causing further collapse of the pharynx leading to worsening of he inspiration airflow obstruction [11].
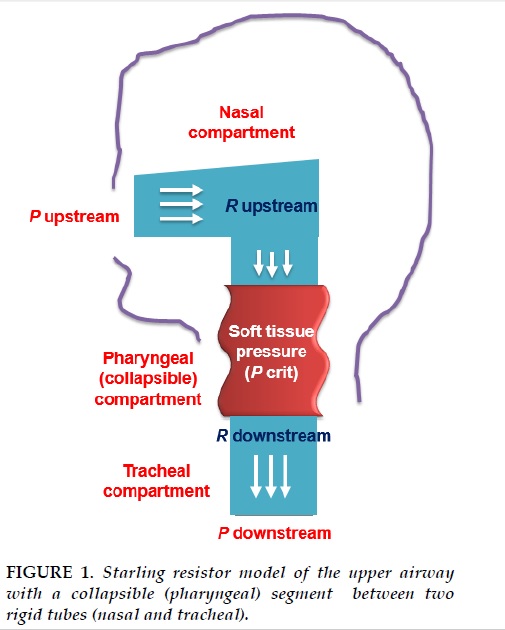
The mechanism of nasal airway resistance can be explained by the Starling resistance model. The Starling model emphasizes that the upper airway is a hollow tube and that partial obstruction at the inlet, corresponding to the nose, results in a collapsible segment downstream corresponding to the oropharynx. The critical closing pressure can be affected by many factors, such as gender, body mass index (BMI), congenital and hereditary defects of the upper airway and the others factors are known to contribute to airway dysfunction in OSAS [7,11,12]. As expected, with increasing nasal congestion oral breathing becomes predominant, but unlike expected this can lead to increasing disordered breathing since oral breathing fails to activate upper airway dilator muscles by activation of the negative pressure reflex, leading to an increased tendency for the upper airway to collapse [12]. During sleep in a healthy person, nasal ventilation reflexes respond to respiratory rate and minute ventilation. When nasal airflow is restricted or absent, as seen in the upper airway obstruction, ventilation during sleep will be decreased and arousals during sleep will be increased. When flow limitation is present, maximal inspiratory flow is defined by (Pupstream-Pcrit)/Rupstream, where Pcrit is the critical closing pressure (tissue pressure); Pupstream= upstream pressure; Pdownstream= downstream pressure; Rupstream=upstream resistance, and Rdownstream=downstream resistance.
Nasal congestion, which results when the cavernous tissues of the nasal turbinates swell following dilation of the capacitance vessels, is a common and bothersome symptom that affects numerous allergic rhinitis patients. Its mechanism involves the reduction in the internal nasal diameter and the increase in airway resistance to nasal airflow, and the symptom can also cause nasal obstruction. Subjective, symptoms of nasal congestion exist, as well as objective measures of decrease nasal airflow, such as peak nasal inspiratory flow (PNIF), assessments of airway resistance and conductance (rhinomanometry), and acoustic rhinometry, which assesses the volume and area of the nasal cavity by assessing reflected sound waves [4,9,11,12]. The symptom of nasal congestion worsens at night and first thing in the morning, peaking at 6 AM, presumptively due to the posture change when an individual lays down and to the normal decrease in serum cortisol levels overnight. The lower cortisol levels lead to greater nocturnal airway obstruction and may partially explain the large-amplitude, circadian variation (Figure 1). These changes may serve to explain why patients with inflammatory nasal conditions and nasal congestion often suffer from sleep impairment and daytime fatigue. Results from an internet survey of 2,355 individuals with allergic rhinitis or the parents of children with allergic rhinitis further reinforced the complaints of those suffering from the disorder. 85% of the respondents or their children reported experiencing nasal congestion, and 40% of all respondents, the greatest proportion of participants who rated the severity of various symptoms, considered their nasal congestion severe. Approximately 50% of the respondents reported that nasal congestion was their most bothersome symptom and that it woke them during the night and made it difficult to fall asleep. 20% of adult respondents claimed that their partner’s or spouse’s sleep was adversely affected by their nasal congestion, and the degree of sleep impairment correlated with the severity of their congestion. Moreover, the survey revealed that nasal congestion negatively impacted the individuals’ or their children’s emotions and ability to perform daily activities, all of which may result from the detrimental effects of nasal congestion on sleep. Studies on treatments for the nasal congestion associated with allergic rhinitis, such as one by Craig et al. on treatment with topical nasal corticosteroids, propose that the poor sleep and daytime somnolence characteristic of the disorder is predominantly attributed to the symptom of nasal congestion. Increased sleep apnea and transient arousals even occur when subjecting healthy individuals to nasal occlusion with a nose clip. Previous studies that objectively assessed the sleep patterns of allergic rhinitis patients demonstrated that their symptoms of nasal congestion led to increased microarousals and episodes of apnea at night. Subjective instruments, such as Juniper’s Nocturnal Rhinoconjunctivitis Quality of Life Questionnaire (NRQLQ), correlate with the objective findings noted on polysomnography. Allergic rhinoconjunctivitis patients who complained of impaired sleep due to night time symptoms found nasal and sinus congestion to be among their most bothersome and troublesome symptoms.
The activation of the mediators of inflammation such as histamine and cytokines are examples of inflammatory mediators released in the process of an allergic reaction, and such mediators may directly influence the central nervous system and result in the disturbed sleep and daytime somnolence characteristic of allergic rhinitis. Histamine helps regulate the sleep-wake cycle and arousal, while the higher levels of the cytokines interleukin (IL)-1β, IL-4, and IL-10 seen in patients with allergies, compared with healthy individuals, correlate with increased latency to rapid eye movement (REM) sleep, decreased time in REM sleep, and increased latency to sleep onset. It is postulated that any such disruptions in REM sleep may cause daytime fatigue, difficulty concentrating, and poor performance in allergic rhinitis patients. Inflammatory cells and mediators exhibit evident circadian variation, with its highest levels in the early morning hours, thus possibly explaining why the peak of allergic rhinitis symptoms frequently occurs upon waking and why night time sleep is detrimentally affected in the disorder.
During sleep, the obstruction of the upper airway leads to a reduced (hyponoea) or interrupted (apnoea) airflow, which can daytime sleepiness. Several studies support the fact that some inflammatory mediators, such as cytokines and NO may contribute to the fatigue and quality of life; however structural changes in the airway also is a variable for sleep quality. Many structural factors affect to the sleep quality, upper airway dilator muscle dysfunction, neck size, posture, abnormal facial anatomy and physical nasal obstruction. Obviously, in allergic rhinitis swelling of the upper airway mucosa leads to obstruction of the airway and decrease in airflow. Sleep is further degraded by cytokine inflammatory mediators that are over produced in allergic rhinitis such as IL-4, IL-5 and IL-13.
The study by Lavigne et al, demonstrated that the inflammation in the upper airway in obstructive sleep apnea syndrome (OSAS) patients when treated with topical intranasal corticosteroids lead to greater reduction in disease severity in OSAS patients with AR, than those without AR, by reducing the level of inflammation in upper airwayThe baseline values for apnea hyponea index (AHI), the arousals, oxygen saturation, sleep architecture were collected in this study with and without allergic rhinitis. They hypothesized that CS treatment can lead to the reduction in the patients with OSAS and allergic rhinitis and they were successful demonstrating a positive outcome. Standard sleep indices improved after CS treatment, demonstrated significantly improved oxygen saturation, AHI score in the group with AR and improvement were not seen in the non-AR group. During treatment, fewer eosinophils and CD4 lymphocytes were noted in AR group, but with minimal changes in the non-AR group [13,14].
The same study found that subjects in the CS treatment reported a reduction in sneezing, post nasal drip, nasal obstruction, and the immune responses in the upper airway. There were changes in the number of CD4 lymphocytes in the inferior turbinate, nasopharynx and uvula in AR and also in non-AR. The greatest change was for CD4 lymphocytes, in that there were more CD4+ cells in the nasopharynx in allergic subjects than in non-allergic subjects before therapy (P<0.001), however, after treatment, there were no longer any significant differences in CD4 cell counts at any of the sites sampled between the allergic and non allergic subjects (P>0.05). This means treatment significantly reduced CD4 lymphocytes mainly in the allergic patients.
On the assessment of sleep parameters, after treatment, the allergic group improved in several indices of sleep-disordered breathing. The level of oxygen saturation was lower (P=0.016) in the non-allergic group compared with the allergic patients. Furthermore, CS reduced the AHI score in the supine position in allergic subjects significantly more than in non-allergic subjects (P=0.05) and this improvement persisted even after adjusting for age, BMI, and gender.
THE IMPACT OF SLEEP ON QUALITY OF LIFE (QOL)
As noted above, allergic rhinitis (AR) is a common disorder, affecting between 20 and 30% of patients in the EU and USA. AR is classified by ARIA guidelines (Allergic Rhinitis and its impact on Asthma) and recently, Valero et al suggested three instead of two categories to classify rhinitis severity: mild (no ARIA items affected), moderate (one of three items affected) and severe (all four items effected ). Daytime symptoms, including sleepiness, irritability, depressed mood and various aspects of cognitive dysfunction can expect to impact patient’s QOL secondary to AR. In short, QOL is a concept encompassing the physical, mental and social components associated with an illness or its treatment as perceived by the patient. Many studies have reported impairment of QOL in AR patients. Subjects with more severe impairment and persistent rhinitis symptoms score significantly worse on these QOL instruments. Sleep disturbances with AR can lead to decreased cognitive and psychomotor abilities, impaired work performance, decreased productivity, impaired learning, difficulty concentrating and memory deficits. QOL as reflected by somnolence, daytime fatigue, sleepiness, impaired memory, mood and sexuality. Other symptoms can also result that can further lead to a decrement of QOL and include headaches upon awakening, anxiety, depression and daytime somnolence.
THE EVOLUTION OF MANAGEMENT AND THERAPY IN THE PATIENT WITH AR AND ASSOCIATED WITH SLEEP DISORDER BREATHING
Treatments aimed at reducing nasal congestion may alleviate sleep disturbances and daytime somnolence and consequently improve the quality of life in those who suffer from allergic rhinitis. However, the treatments for the disorder vary in their efficacies. Sedating antihistamines are no longer recommended in allergic rhinitis and are especially contraindicated in patients who complain of sleep disordered breathing, daytime sedation, fatigue, and functional impairment. Common treatment for allergic rhinitis includes non-sedating oral antihistamines, which alleviate nasal symptoms, such as rhinorrhea, sneezing, and pruritus, but may be less effective in reducing nasal congestion. Studies by Murray et al, Golden et al and others suggest that treatment using oral ono-sedating antihistamines or topical antihistamines result in improved sleep and quality of life, but less so than topical nasal corticosteroids.
Oral decongestants are successful in improving nasal congestion but may detrimentally impact sleep due to their stimulatory effects and, additionally, may result in systemic side effects, such as tachycardia, urinary retention and decrease sexuality. For these reasons the benefits of oral decongestants are often outweighed the adverse effects. Topical decongestants improve sleep in patients with nasal obstruction, but should not be used for more than a few days, due to the risk of rhinitis medicamentosa, or “rebound” congestion. Minimal data are available suggesting that use of nasal corticosteroids and topical decongestants can be used together safely for prolonged periods; but more data are needed before suggesting this treatment. Data, though very limited, shows that the anticholingeric agent, ipratropium bromide, may improve sleep and used as first-line therapy when congestion or sleep disordered breathing are the predominant symptoms in patients with AR.
The role of intranasal corticosteroids have been shown to effectively relieve all the nasal symptoms of allergic rhinitis including congestion. The effectiveness of intranasal corticosteroids in relieving nasal congestion may have a positive impact on sleep, daytime somnolence, and quality of life in patients who suffer from allergic rhinitis. Studies on adults and children with PAR support the hypothesis that intranasal corticosteroids decrease nasal congestion and subjective daytime sleepiness and fatigue, and improve sleep and quality of life. Further studies displayed efficacy in the improvement of nasal symptoms and quality of life, as well as verbal memory. Treatment was also proven to alleviate allergic rhinitis associated with OSAS and to consequently lead to both significantly lower frequencies of apnea/hypopnea episodes and subjective improvements in nasal congestion and daytime alertness, though snoring noise was unchanged. Studies in allergic rhinitis patients using the RQLQ, NRQLQ and the Pittsburgh Sleep Quality Index revealed that intranasal corticosteroid improves both nasal congestion and health-related quality of life, including sleep. These studies therefore support the notion that treatments focusing on the nasal symptoms of allergic rhinitis may reduce sleep impairment and improve patients’ quality of life. As noted, intranasal corticosteroids reduce congestion, improve sleep and sleep problem, reduce daytime sleepiness, fatigue and inflammation. This benefit includes budesonide, flunisolide, triamcinolone acetonide, fluticasone propionate and fluticasone furoate. There is actually a correlation between the reduction in nasal congestion and improvement in sleep and daytime somnolence [13,15,16]. In one study, 20 patients with AR and symptoms of daytime sleepiness with therapy with flunisolide, which signicantly improved sleep quality and congestion. In another study, fluticasone propionate improved nasal congestion and also quality of sleep, which demonstrates this is an attribute of the class and not of just certain topical corticosteroids. These symptoms were evaluated as an average of 3 individual symptom scores-difficultly falling asleep nasal congestion on awakening, nighttime awakening. There is an increased prevalence of AR in the patients with OSAS. Intranasal fluticasone is of benefit to some patients with OSAS and Rhinitis [11,17,18].
Role of antihistamines for therapy in patients with AR and SDB In turn, sedating antihistamines are associated with central nervous system effects such as sedation, however, the patient does not always perceive these effects, but they are evident with objective performance testing, and position emission tomography scanning has directly demonstrated central H1 receptor occupancy. First generation H1 antihistamines have been known to cause subjective somnolence and objective performance impairment [16,19,20] and are a concern among patients with safety-critical occupations [3]. Second generation H1 antihistamines reduce or eliminate sedative effects, therefore the CNS effects are avoidable, and for this reason first-generation H1 antihistamines should no longer be used in the management of allergic rhinitis when non sedative drugs are available [21]. The second generation H1 antihistamines desloratadine and fexofenadine have proven to be almost free of adverse effects in terms of subjective sleepiness, daytime sleep latency and psychomotor performance. These findings support the use of antihistamines in patients involved in activities requiring increased attention.
Role of decongestants in AR and SDB decongestants decrease nasal congestion but their effect on sleep has not been extensively studied. Oral decongestants when dosed to late in the day may disturb sleep by inducing insomnia and as noted above may interfere with sexuality. Antihistamine decongestant combinations are used routinely for the treatment of seasonal allergic rhinitis; however, can induce the same adverse effect profile as solo oral decongestants can. Topical decongestants may provide some benefit in SDB as noted above, but prolonged use is discouraged due to receptor down regulation. Some have advocated that combining topical nasal decongestants with topical nasal corticosteroids may have greater benefit on SDB and avoid the rebound effect of decongestants, but minimal data support this symbiosis. Intranasal corticosteroids reduce congestion, improve sleep and sleep problem, reduce daytime sleepiness, fatigue and inflammation. These include nudesonide, flunisolide, triamcinolone acetonide, fluticasone propionate and fluticasone furoate. There is the correlation between the reduction in nasal congestion and improvement sleep and daytime somnolence [22,23]. In one study, 20 patients with AR and symptoms of daytime sleepiness with therapy with flunisolide, which signicantly improved sleep quality and congestion. In another study, fluticasone propionate improved nasal congestion and also quality of sleep [24,25]. These symptoms were evaluated as an average of 3 individual symptom scoresdifficultly falling asleep nasal congestion on awakening and nighttime awakening. In addition, there is an increased prevalence of AR in the patients with OSAS. Intranasal fluticasone is of benefit to some patients with OSAS and Rhinitis.
CONCLUSION
The quality of life in patients with allergic rhinitis is detrimentally impacted by the sleep impairment associated with the disorder. One of the key causes leading to sleep disruptions and sleep-disordered breathing is nasal congestion, one of the most common and bothersome symptoms of allergic rhinitis. Recent research has led to the use of therapeutic agents that specifically target the nasal congestion associated with sleep impairment. Intranasal corticol-steroids stand as effective treatment that significantly reduces nasal congestion in allergic rhinitis. Clinical trials using this treatment suggest that this reduction in nasal congestion correlates with decreased sleep impairment, reduced daytime somnolence, and improved quality of life. Further research is necessary to definitively conclude with objective instruments that intranasal corticosteroids hold the ability to improve sleep and quality of life in patients with allergic rhinitis. In addition, studies with immunotherapy are needed since few have addressed sleep or daytime somnolence. These studies should utilize sleep-related measures as primary endpoints and assess sleep parameters both subjectively and objectively, thus serving to identify the most effective therapies for alleviating the detrimental effects of sleep impairment associated with allergic rhinitis.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
REFERENCES
1. Léger D, Annesi-Maesano I, Carat F, Rugina M, Chanal I, Pribil C, El Hasnaoui A, Bousquet J. Allergic rhinitis and its consequences on quality of sleep: an unexplored area. Arch Intern Med. 2006;166:1744-8.
2. Ng DK, Chan CH, Kwok KL, Cheung JM. Allergic rhinitis as a risk factor for habitual snoring in children. Chest. 2005;127:2285-2286.
3. Carah B. Santos, Ellen L. Pratt, Chris Hanks, Jeffery McCann, Timothy J. Craig. Allergic rhinitis and its effect on sleep, fatigue, and daytime somnolence. Ann Allergy Asthma Immunol. November 2006Volume 97, Issue 5, Pages 579–587.
4. Bhattacharyya N. Incremental healthcare utilization and expenditures for allergic rhinitis in the United States. Laryngoscope. 2011;121:1830-1833) .
5. Canonica GW, Bousquet J, Mullol J, Scadding GK, Virchow JC. A survey of the burden of allergic rhinitis in Europe. Allergy. 2007;62(Suppl 85):17-25.
6. Suratt PM, Turner BL, Wilhoit SC (1986) Effect of intranasalobstruction on breathing during sleep. Chest 90 (3):324–329.
7. Lavie P, Fischel N, Zomer J, Eliaschar I (1983) The effects of partial and complete mechanical occlusion of the nasal passages on sleep structure and breathing in sleep. Acta Otolaryngol 95(1–2):161–166).
8. Nadeem R, Molnar J, Madbouly EM, et al. Serum Inflammatory Markers in Obstructive Sleep Apnea: A Meta-Analysis. J Clin Sleep Med. 2013;9(10):1003-1012.
9. Krouse HJ, Davis JE, Krouse JH (2002) Immune mediators in allergic rhinitis and sleep. Otolaryngol Head Neck Surg 126(6): 607–613).
10.Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP. Pathophysiology of Sleep Apnea. Physiol Rev. 2010;90 (1):47-112.)
11.Jason P.Kirkness , Vidya K., Susheel P.Patil, Hartmut S. Upper Airway Obstruction in Snoring and upper Airway Resistance Syndrome.Prog Respir Res.2006.vol 35:7989.
12.Chelle P.Wilhelm , Richard D.deShazo, Sadeka Tamanna, M.Iftekhar Ullah, Leigh Baldwin Skipworth.The nose, upper airway, and obstructive sleep apnea.Ann Allergy Asthma Immunol 115.96-102.2015/12//
13. McLean HA, Urton AM, Driver HS, et al. Effect of treating severe nasal obstruction on the severity of obstructive sleep apnea. Eur Respir J 25:521, 2005.
14. F. Lavigne, B.J.Petrof, J.R.Johnson, P. Lavigne , N. Binothman, G-O.Kassissia, M.Al Samri , C.Giordano, N.Dube, D.Hercz, A.Benedetti , Q. Hamid. Effect of topical corticosteroids on allergic airway inflammation and disease severity in obstructive sleep apnoea.Clinical and Experimental Allergy, Volume 43,issue 10, 1124-1133
15. Juniper EF, Rohrbaugh T, Meltzer EO. A questionnaire to measure quality of life in adults with nocturnal allergic rhinoconjunctivitis. J Allergy Clin Immunol 111:484, 2003
16. Kessler RC, Almeida DM, Berglund P, Stang P. Pollen and mold exposure impairs the work performance of employees with allergic rhinitis. Ann Allergy Asthma Immunol 87:289, 2001.
17. Kiely JL, Nolan P, McNicholas WT. Intranasal corticosteroid therapy for obstructive sleep apnoea in patients with co-existing rhinitis. Thorax 59:50, 2004.
18. Kremer B, den Hartog HM, Jolles J. Relationship between allergic rhinitis, disturbed cognitive functions and psychological well-being. Clin Exp Allergy 32:1310, 2002.
19. Camhi SL, Morgan WJ, Pernisco N, Quan SF. Factors affecting sleep disturbances in children and adolescents. Sleep Med 1:117,2000.
20.Canova CR, Downs SH, Knoblauch A, Andersson M, Tamm M, Leuppi JD. Increased prevalence of perennial allergic rhinitis in patients with obstructive sleep apnea. Respiration 71 : 138, 2004.
21. Hughes K, Glass C, Ripchinski M, et al. Efficacy of the topical nasal steroid budesonide on improving sleep and daytime somnolence in patients with perennial allergic rhinitis. Allergy 58:380,2003.
22. Juniper EF, Rohrbaugh T, Meltzer EO. A questionnaire to measure quality of life in adults with nocturnal allergic rhinoconjunctivitis. J Allergy Clin Immunol 111:484, 2003.
23.Kessler RC, Almeida DM, Berglund P, Stang P. Pollen and mold exposure impairs the work performance of employees with allergic rhinitis. Ann Allergy Asthma Immunol 87:289, 2001./23//
24. Kiely JL, Nolan P, McNicholas WT. Intranasal corticosteroid therapy for obstructive sleep apnoea in patients with co-existing rhinitis. Thorax 59:50, 2004.
25. Kremer B, den Hartog HM, Jolles J. Relationship between allergic rhinitis, disturbed cognitive functions and psychological well-being. Clin Exp Allergy 32:1310, 2002.
FIGURES
REFERENCES
1. Léger D, Annesi-Maesano I, Carat F, Rugina M, Chanal I, Pribil C, El Hasnaoui A, Bousquet J. Allergic rhinitis and its consequences on quality of sleep: an unexplored area. Arch Intern Med. 2006;166:1744-8.
2. Ng DK, Chan CH, Kwok KL, Cheung JM. Allergic rhinitis as a risk factor for habitual snoring in children. Chest. 2005;127:2285-2286.
3. Carah B. Santos, Ellen L. Pratt, Chris Hanks, Jeffery McCann, Timothy J. Craig. Allergic rhinitis and its effect on sleep, fatigue, and daytime somnolence. Ann Allergy Asthma Immunol. November 2006Volume 97, Issue 5, Pages 579–587.
4. Bhattacharyya N. Incremental healthcare utilization and expenditures for allergic rhinitis in the United States. Laryngoscope. 2011;121:1830-1833) .
5. Canonica GW, Bousquet J, Mullol J, Scadding GK, Virchow JC. A survey of the burden of allergic rhinitis in Europe. Allergy. 2007;62(Suppl 85):17-25.
6. Suratt PM, Turner BL, Wilhoit SC (1986) Effect of intranasalobstruction on breathing during sleep. Chest 90 (3):324–329.
7. Lavie P, Fischel N, Zomer J, Eliaschar I (1983) The effects of partial and complete mechanical occlusion of the nasal passages on sleep structure and breathing in sleep. Acta Otolaryngol 95(1–2):161–166).
8. Nadeem R, Molnar J, Madbouly EM, et al. Serum Inflammatory Markers in Obstructive Sleep Apnea: A Meta-Analysis. J Clin Sleep Med. 2013;9(10):1003-1012.
9. Krouse HJ, Davis JE, Krouse JH (2002) Immune mediators in allergic rhinitis and sleep. Otolaryngol Head Neck Surg 126(6): 607–613).
10.Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP. Pathophysiology of Sleep Apnea. Physiol Rev. 2010;90 (1):47-112.)
11.Jason P.Kirkness , Vidya K., Susheel P.Patil, Hartmut S. Upper Airway Obstruction in Snoring and upper Airway Resistance Syndrome.Prog Respir Res.2006.vol 35:7989.
12.Chelle P.Wilhelm , Richard D.deShazo, Sadeka Tamanna, M.Iftekhar Ullah, Leigh Baldwin Skipworth.The nose, upper airway, and obstructive sleep apnea.Ann Allergy Asthma Immunol 115.96-102.2015/12//
13. McLean HA, Urton AM, Driver HS, et al. Effect of treating severe nasal obstruction on the severity of obstructive sleep apnea. Eur Respir J 25:521, 2005.
14. F. Lavigne, B.J.Petrof, J.R.Johnson, P. Lavigne , N. Binothman, G-O.Kassissia, M.Al Samri , C.Giordano, N.Dube, D.Hercz, A.Benedetti , Q. Hamid. Effect of topical corticosteroids on allergic airway inflammation and disease severity in obstructive sleep apnoea.Clinical and Experimental Allergy, Volume 43,issue 10, 1124-1133
15. Juniper EF, Rohrbaugh T, Meltzer EO. A questionnaire to measure quality of life in adults with nocturnal allergic rhinoconjunctivitis. J Allergy Clin Immunol 111:484, 2003
16. Kessler RC, Almeida DM, Berglund P, Stang P. Pollen and mold exposure impairs the work performance of employees with allergic rhinitis. Ann Allergy Asthma Immunol 87:289, 2001.
17. Kiely JL, Nolan P, McNicholas WT. Intranasal corticosteroid therapy for obstructive sleep apnoea in patients with co-existing rhinitis. Thorax 59:50, 2004.
18. Kremer B, den Hartog HM, Jolles J. Relationship between allergic rhinitis, disturbed cognitive functions and psychological well-being. Clin Exp Allergy 32:1310, 2002.
19. Camhi SL, Morgan WJ, Pernisco N, Quan SF. Factors affecting sleep disturbances in children and adolescents. Sleep Med 1:117,2000.
20.Canova CR, Downs SH, Knoblauch A, Andersson M, Tamm M, Leuppi JD. Increased prevalence of perennial allergic rhinitis in patients with obstructive sleep apnea. Respiration 71 : 138, 2004.
21. Hughes K, Glass C, Ripchinski M, et al. Efficacy of the topical nasal steroid budesonide on improving sleep and daytime somnolence in patients with perennial allergic rhinitis. Allergy 58:380,2003.
22. Juniper EF, Rohrbaugh T, Meltzer EO. A questionnaire to measure quality of life in adults with nocturnal allergic rhinoconjunctivitis. J Allergy Clin Immunol 111:484, 2003.
23.Kessler RC, Almeida DM, Berglund P, Stang P. Pollen and mold exposure impairs the work performance of employees with allergic rhinitis. Ann Allergy Asthma Immunol 87:289, 2001./23//
24. Kiely JL, Nolan P, McNicholas WT. Intranasal corticosteroid therapy for obstructive sleep apnoea in patients with co-existing rhinitis. Thorax 59:50, 2004.
25. Kremer B, den Hartog HM, Jolles J. Relationship between allergic rhinitis, disturbed cognitive functions and psychological well-being. Clin Exp Allergy 32:1310, 2002.