
 English
English
 French
French
Distribution and antibiotic resistance of bacterial induced ventilator - associated pneumonia at the intensive care unit
Distribution et résistance aux antibiotiques des bactéries responsables de la pneumonie associée au ventilateur à l'unité de soins intensifs
L. Pham, V. Nguyen Nhu, S. Nguyen Van
Department of Intensive Care Unit. Pham Ngoc Thach Hospital. Hochiminh City. Vietnam
Corresponding author
Dr. PHAM Luc
Department of ICU. PNT Hospital. Hochiminh City. Vietnam
Email: phamlucpnt@gmail.com
DOI: 10.12699/jfvpulm.8.25.2017.29
ABSTRACT
Introduction and Objective. Ventilator - associated pneumonia (VAP) is a severe disease with high mortality. The bacteria causing VAP have been varied between countries, hospitals, and change over time. The empiric choice of antibiotics as the first-line should be based on microbiological data and on-site antibiotic resistance. This retrospective study aimed to evaluate: 1) the change in distribution of bacterial induced pneumonia; 2) the modification of bacterial antibiotic resistance; 3) the first-line therapy of antibiotics for VAP in intensive care unit.
Results. During 7 years, 748 samples were collected. Three types of bacteria accounting for the highest rates over the years were A. baumannii, Klebsiella spp, and Pseudomonas spp. Other bacteria accounting for a small proportion were Enterobacter spp, E. coli, S. aureus, etc. A. baumannii was always accounted for the highest proportion over the years: in 2016, it was 38%. The percentage of Klebsiella spp, Pseudomonas spp was varied over years without significant difference: in 2016, it was accounted for 30% and 17%, respectively. A. baumannii resistance was >80% with cefepime, ceftazidime, imipenem, meropenem, piperacillin/tazobactam (PTZ), quinolone, and aminoglycoside; the resistance to cefoperazone/sulbactam, and doxycycline was varied over the years: in 2016, it was 7.1% and 26.7%, respectively. There was no record for the resistance to polymyxin B from 2012- 2016. Klebsiella spp resistance was high: >80% to ceftazidime, cefoperazone, cefepim, and quinolone; >70% to PTZ, ampicillin/sulbactam (2016); the resistance to cefoperazone/sulbactam, amikacin was varied over the years: in 2016, it was accounted for 42.1% and 14.8%, respectively. The resistance to meropenem and imipenem was varied over the years: in 2016, it was 71.4% and 72.4%, respectively. There was no record of resistance to polymyxin B over the years. Pseudomonas spp was highly resistant to ceftazidime, cefepim, and PTZ in 2010, 2011; the resistant rate was decreased in the last two years: in 2016, it was reported for 41.2%, 41.2%, and 14.3%, respectively. The resistance to cefoperazone/sulbactam was 75.9% in 2010 and 30.8% in 2016. The resistance to levofloxacin and ciprofloxacin was high over the years: in 2016, it was about 64.7% and 58.8%, respectively. The resistance to amikacin was varied over the years; it was 43.8% in 2016. The resistance to imipenem and meropenem was high, but gradually reduced in the last two years: in 2016, it was 47.1%. Polymyxin B had not been recorded for the resistance from 2012-2015. However, in 2016, it was reported 5.9% for polymyxin B resistance.
Conclusion. Bacteria causing VAP was mainly negative Gram bacteria. The three most commonly presented bacteria included A. baumannii, Klebsiella spp, Pseudomonas spp. A. baumannii was highly resistant to many groups of antibiotics.
KEYWORDS: Pneumonia; mechanical ventilation; bacteria; antibiotic resistance
RÉSUMÉ
Introduction et Objectifs. La pneumonie associée au ventilateur (PAV) est une maladie grave avec une haute mortalité. Les bactéries responsables du PAV ont varié entre les pays, les hôpitaux et les changements au cours du temps. Le choix empirique des antibiotiques en première intention devrait être basé sur des données microbiologiques et sur la résistance aux antibiotiques sur place. Cette étude rétrospective visait à évaluer: 1) le changement dans la distribution de la pneumonie induite par des bactéries; 2) la modification de la résistance bactérienne aux antibiotiques; 3) la thérapie de première ligne des antibiotiques pour PAV en unité de soins intensifs.
Résultats. Pendant 7 ans, 748 échantillons ont été collectés. A. baumannii, Klebsiella spp et Pseudomonas spp. étaient les trois types de bactéries qui étaient enregistré avec les fréquences les plus hautes au cours des années. Les autres bactéries représentant une faible proportion étaient Enterobacter spp, E. coli et S. aureus, etc. A. baumannii représentait toujours le pourcentage le plus élevé au cours des années: en 2016, il était de 38%. Le pourcentage de Klebsiella spp, Pseudomonas spp a été varié au cours des années sans différence significative: en 2016, il a été estimé respectivement de 30%, 17%. La résistance à A. baumannii était >80% pour le céfépime, la ceftazidime, l'imipénème, le méropénème, la pipéracilline/tazobactam (PTZ), la quinolone et l'aminoglycoside; la résistance à la céfopérazone/sulbactam et à la doxycycline a été varié au cours des années: en 2016, il était respectivement de 7,1% et 26,7%. Il n'y avait aucun record pour la résistance à la polymyxine B de 2012-2016. La résistance de Klebsiella spp était élevée: >80% pour la ceftazidime, la céfopérazone, la céfépine et la quinolone; > 70% pour PTZ, ampicilline/sulbactam (2016); la résistance à la céfopérazone/sulbactam, l'amikacine a été variée au fil des années: en 2016, il représentait respectivement de 42,1% et 14,8%. La résistance au méropénème et à l'imipénème a été varié au cours des années: en 2016, il était de 71,4% et 72,4% respectivement. Il n'y avait aucune rapport de résistance à la polymyxine B au cours des années. Pseudomonas spp était hautement résistant à la ceftazidime, au cefepim et au PTZ en 2010, 2011; le taux de résistance a été diminué au cours des deux dernières années: en 2016, il a été rapporté de 41,2%, 41,2% et 14,3%, respectivement. La résistance au céfopérazone/sulbactam était de 75,9% en 2010 et de 30,8% en 2016. La résistance des bactéries à la lévofloxacine et à la ciprofloxacine était élevée au cours des années. En 2016, il était respectivement d'environ 64,7% et 58,8%. La résistance à l'amikacine a été varié au cours des années. Il était de 43,8% en 2016. La résistance à l'imipénème et à la méropénème était élevée, mais progressivement réduite au cours des deux dernières années, donc en 2016, il était de 47,1%. La polymyxine B n'était pas enregistrée pour la résistance de 2012 à 2015. Cependant, en 2016, il a été signalé que la résistance à la polymyxine B était de 5,9%.
Conclusion. Les bactéries causant la PAV étaient principalement des bactéries à Gram négatif. Les trois bactéries les plus fréquents étaient A. baumannii, Klebsiella spp, Pseudomonas spp. A. baumannii était très résistant à de nombreux groupes d'antibiotiques.
MOTS CLÉS: Pneumonie; ventilation mécanique; bactéries; résistance antibiotique
INTRODUCTION
Ventilator - associated pneumonia (VAP) is a severe disease with high mortality. In intensive care units, hospital-acquired infection is always a matter of concern, particularly in patients with VAP. In developed countries, the average frequency of VAP is 1% for each day of mechanical ventilation [1].
In intubated patients, the risk of pneumonia increases by 3 to 10 times compared to patients who are not intubated. Mortality rates in the VAP group ranging from 24 to 50% and may reach at 76% if bacterial infections are caused by highly virulent bacteria. As a result, VAP is one of the leading causes of increased burden for health care system, increased treatment costs, and increased mortality among patients with VAP at intensive care units.
On the other hand, that is also one of the causes for the difficulties of withdraw mechanical ventilation, which prolongs then mechanical ventilation duration [1].
Hospital-acquired pneumonia is a pneumonia that occurs after 48 hours of hospitalization, with no incubation at the time of admission. VAP is defined as pneumonia that occurs after 48 to 72 hours of mechanical ventilation, with no incubation at the time of intubation [2]. According to the Infectious Diseases Society of American and American Thoracic Society (IDSA/ATS), hospital-acquired pneumonia and VAP are the cases of pneumonia that occur in hospital setting with or without mechanical ventilation[2].
The International Nosocomial Infection Control Consortium (INICC) was conducted between 2003 and 2008 in many countries in Latin America, Asia (including Vietnam), Africa and Europe which included 173 of intensive care units (ICUs) and 155,358 participated patients. The results showed that the overall rate of VAP was 13.6/1,000 days of mechanical ventilation, of which the highest prevalence was in the ICUs of Trauma (51.7%) and Neuropathy Surgery (25.3%) [3].
The main cause of pneumonia is bacteria. Bacteria distribution varies between countries, regions, and changes over time. In Vietnam, previous studies have shown that hospital-acquired pneumonia was caused by Gram negative multidrug resistant bacteria, such as Klebsiella spp, E. coli, P. aeruginosa, A. baumannii, and Enterobacter spp. Gram (-) bacteria secrete ESBL (extended-spectrum β-lactamases), which are resistant to many antibiotics, tend to increase recently (local data). VAP in the ICUs most commonly seen are A. baumannii and multidrug resistant P. aeruginosa.
Methicillin-resistant Staphylococcus aureus (MRSA) accounts for 50-60% of isolated S. aureus that cause hospital-acquired pneumonia and VAP.
According to IDSA/ATS 2016, the first choice of antibiotics according to experience (empiric) should be based on data of on-site antibiotic resistance [2].
Therefore, this study was realized with the following objectives: 1) to evaluate the change of bacterial distribution causing VAP at the Intensive Care Unit (ICU) of Pham Ngoc Thach Hospital (Hochiminh city of Vietnam) from 2010 -2016; 2) to evaluate the change of antibiotic resistance of those bacteria; 3) to orientate the selection of first-choice antibiotics for VAP at the ICU of Pham Ngoc Thach Hospital.
METHODS
Study subjects
Patients were diagnosed with VAP at the ICU of Pham Ngoc Thach Hospital from January 2010 to December 2016.
Study method
Study design: retrospective, descriptive, and case series analysis study.
Inclusion criteria of study subjects
Patients with invasive mechanical ventilation ≥48 hours.
Eligible for VAP diagnosis: posterior-anterior chest X-ray with new lesions or in progress and associated with at least two of the following criteria:
+ Purulent sputum.
+ Fever ≥ 38.50C or hypothermia ≤ 350C.
+ White blood count >10,000/mm3 or <4,000/mm3.
+ PaO2 reduction.
There were the results of bacteria cultures from aspiration fluids through the intubation and antibiograms.
Statistical analyses
The data was processed with STATA 8.0 software. Quantitative variables were presented as means ± standard deviation (SD). The comparison of two means was performed by T-test. Qualitative variables were presented as %; the comparison was verified by χ2 or Fisher's exact test. The results were statistically significant when P <0.05.
RESULTS
From January 1st, 2010 to December 31th, 2016, the number of eligible subjects was 748. The results have been recorded as following:
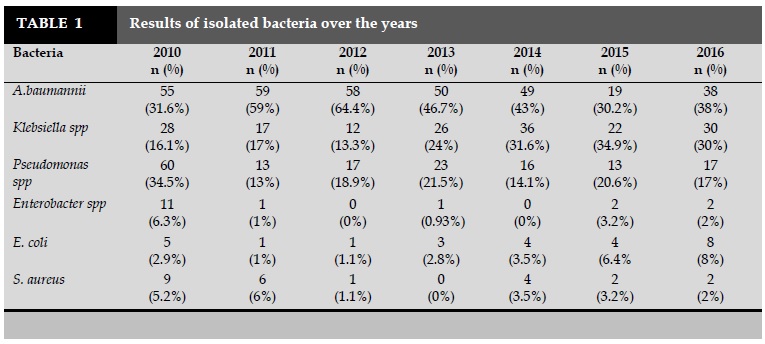
Bacteria distribution over the years (Table 1)
The most commonly seen bacteria included A. baumannii, Klebsiella spp, and Pseudomonas spp.
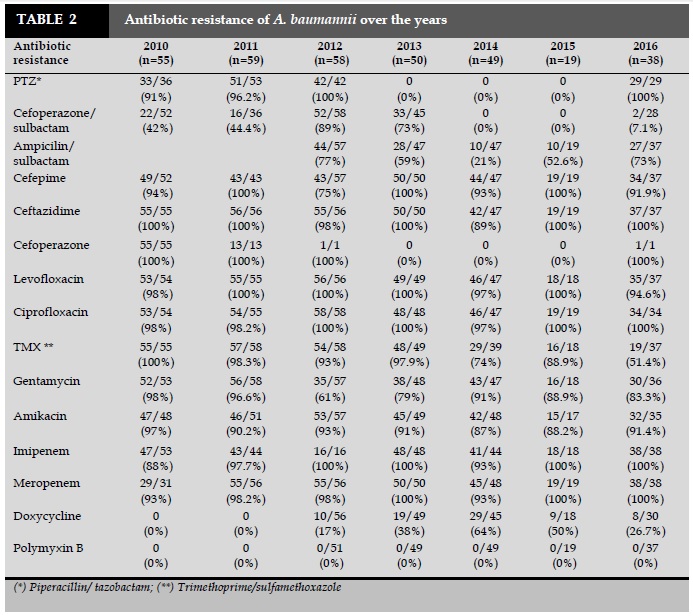
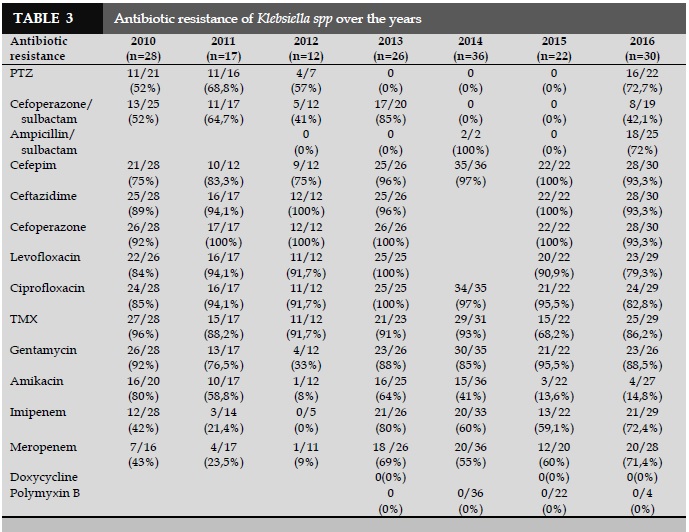
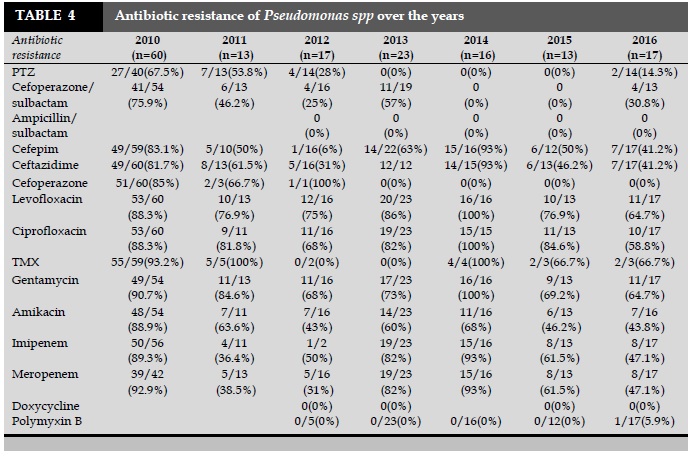
The antibiotic resistance of 3 most commonly seen bacteria A. baumannii (Table 2), Klebsiella spp (Table 3), and Pseudomonas spp (Table 4).
DISCUSSION
Bacteria distribution of pneumonia
The results of yearly bacteria isolation for 7 years are presented in Table 1. The isolated bacteria included A. baumannii, Klebsiella spp, Pseudomonas spp, Enterobacter spp, E. coli, S. aureus. The other bacteria wereaccounted for negligible percentages. The 3 most commonly seen bacteria were A. baumannii, Klebsiella spp, and Pseudomonas spp.
A. baumannii always had a higher rate than other bacteria. The distribution of this bacteria was increased statistically significant in 2011, 2012 in comparison with 2010 (P<0.05). However, this rate was declined and significantly different in 2014 compared to 2012 (43% vs 64.4%; P<0.05). Then, it was varied non significantly until 2016, which was still accounted for the highest percentage (38%). The interesting point is that the distribution of A. baumannii has been varied significantly after 1 to 2 years.
The percentage of Klebsiella spp, Pseudomonas spp was varied over years with non significant difference (P>0,05). In 2016, it was accounted for 30% and 17%, respectively.
Enterobacter spp, E. coli, and S. aureus were low in frequency, varying in years. However, the difference was not statistically significant (P>0.05).
A follow-up study of microbiological process lasting for 11 years (2000-2010) at the ICU of Tropical Diseases Hospital realized by Khanh Nhu et al. in 2014, showed the change of the major pathogenic role from P. aeruginosa to A. baumannii in patients with VAP [4].
In Asia, according to Chung et al. (2011) [5], bacteria causing VAP included A. baumannii (35.7%), S. aureus (28.1%), P. aeruginosa (24.3%), and K. pneumoniae (11.9%). This result showed that in Asia, the main cause of VAP was still mainly Gram negative bacteria, similar to the results of the present study. However, the pathogenic role of S. aureus has been more concerned, especially in the developed countries.
The studies realized by An VD et al. (2017) and Binh NT et al. (2015) (national publication), were conducted at the ICUs in Ho Chi Minh City also had the same results with the three common bacteria types: A. baumannii, P. aeruginosa, and K. pneumoniae.
The similar results of these studies suggest that A. baumannii always occupied the highest percentage in comparison with other bacteria; the rate of other bacteria may be varied among different hospitals, ICUs (medical or surgical department), and time of study.
The high prevalence of A. baumannii causing the disease is a very disturbing feature in ICUs. Most of A. baumannii causing VAP are multidrug-resistant bacteria (MDR) or extensively drug resistance (XDR), which greatly affect the effectiveness of treatment. Further study on the cause of this high incidence of this bacteria is really necessary in the future.
Bacteria antibiotic resistance
A. baumannii
A. baumannii was highly resistant to many antibiotics such as more than 90% to ceftazidime, cefepim, and PTZ. The resistance to ampicillin/sulbactam was 75% in 2012, significantly decreased year after year, to 21% in 2014; then the resistance was increased in the last two years, with the resistance rate of 73% in 2016.
For cefoperazone/sulbactam: the resistance was increased in 2012 and 2013, compared to 2010 and 2011. However, the observation of antibiogram was discontinued during 2 years; the resistance of these antibiotics in 2016 was accounted only for 7.1%. There were the resistance to imipenem and meropenem more than 87% and >80% to ciprofloxacin, levofloxacin, amikacin, and gentamicin. Doxycycline resistance was increased gradually from 2012 to 2014, then decreased significantly in the last two years with the resistance rate in 2016 was 26.7%. Polymyxin B has not been recorded for the resistance from 2012 to 2016.
At the national level, the data of antibiotic resistance are both similar to and different from other studies.
According to Phuong DM et al. (2017; national data), A. baumannii was resistant to ampicillin/sulbactam in the different regions in Vietnam such as 70% in the North, 51.9% in the Central area, and 73.5% in the South. There was a high resistance rate to piperacillin and ceftazidime in all three regions (≥75.9%). The bacterial resistance to amikacinin in the North, the Central area, and the South were 28.6%, 39.6%, and 60.2%, respectively. The resistance to ciprofloxacin was 79.3% in the North, 76.5% in the Central, and 95.2% in the South. The resistance to imipenem in the Central area was lowest accounted for 47.8% vs 76.2% in the North and up to 90.2% in the South.
A. baumannii antibiotic resistance cause difficulty for treatment. Studies show that resistance may change after 1-2 years. Consequently, monitoring of bacteria's antibiotic receptors every year is required.
Klebsiella spp
Klebsiella spp was highly resistant with more than 80% to ceftazidime, cefoperazone, and cefepim. The rate of resistant to PTZ was from 52% to 68.8% in 2010, 2011, and 2012 vs 72.7% in 2016. The resistance rate to ampicillin/sulbactam was 72.7% in 2016.
The rate of resistance to cefoperazone/sulbactam was ranged from 41% to 64.7% in 2010, 2011, and 2012. The resistance rate was increased significantly at 85% in 2013, and decreased to 42.1% in 2016. There was the resistance rate of 90% to levofloxacin and ciprofloxacin. Amikacin resistance had very low frequency in 2012 (8%), but increased significantly in 2013 (64%), then decreased gradually and in 2016 to 14.8%. The low resistance rate to carbapenem (≤ 42%) in 2010, 2011, and 2012; after that, it was highly increased in 2013. In 2016, there were 71.4% and 72.4% of the resistance rate to meropenem and imipenem, respectively. The resistance to polymyxin B was not recognized in 2014, 2015, 2016.
In the study of Binh NT (2015) (local data), realized at the ICU of Trung Vuong Hospital, K. pneumoniae was resistant to ceftazidime at 61,5%, cefepim at 53,9%, and PTZ at 63,2%. However, the resistance to cefoperazone/sulbactam was only 7.7%. The result of this study suggests that cefoperazone/sulbactam should be concerned in the treatment of bacterial infections caused by this type of bacteria. In comparison with the result of the present study that showed K. pneumoniae resistance to these antibiotics was higher (42.1%). However, this rate is still the lowest in comparison with the remaining antibiotics in the groups of β-lactam and β-lactam/β-lactamase inhibitors. In clinical practice, this result may be interested in applying in antibiotic choice and combination.
Pseudomonas spp
Pseudomonas spp was highly resistant to ceftazidime (> 80%) in 2010, 2013, and 2014; then gradually reduced, in 2016 to 41.2%. The resistance to cefepime was varied, the highest rate was in 2010 (83.1%) and 2014 (93%); then it was gradually reduced in the last two years: in 2016, it was reported for 41.2%. PTZ also had the high rate of resistance in 2010 (67.5%), reduced after two years to 28% in 2012; the follow-up with antibiogram was then discontinued. However, in 2016, the resistance rate was 14.3%.
Pseudomonas spp was highly resistant to cefoperazone/sulbactam in 2010 (75.9%), lower in 2013 (57%); the antibiogram was discontinued for follow-up; in 2016, the resistance rate was 30.8%. Levofloxacin, ciprofloxacin were with high resistance by bacteria with ≥68% from 2010 to 2014. In 2016, the resistance rates were 64.7% and 58.8%, respectively. The resistance to amikacin was high in 2010 (88.9%) and in 2014 (68%); it was lower in other years and reached 43.8% in 2016. The resistance rate of imipenem and meropenem was ≥82% in 2010, 2013, and 2014; it was gradually decreased to 47.1% in 2016. Polymyxin B has not been recognized as antibiotic resistance from 2012 to 2015. However, in 2016, it was recorded 5.9% of resistance.
In the study realized by Binh NT (2015; national publication), Pseudomonas spp was resistant to ceftazidime at 43.3%, cefepime in 43.3%, cefoperazone/sulbactam in 36.7%, and PTZ for 19%. This result was nearly similar to the result of the present studies. At Nguyen Tri Phuong Hospital (Hochiminh city, Vietnam), in 2013 to 2015, the changes in antibiotic resistance for β-lactam, β-lactam/β-lactamase inhibitors were negligible. In 3 years, bacteria was sensitive to many types of antibiotics, maintly cefoperazone/sulbactam, ceftazidime, PTZ, and ticarcilline/clavulanate, with the resistance rate was <10% [6].
According to Phuong DM et al. (2017; national publication), P. aeruginosa was resistant to piperacillin in the North for 19.3%, in the Central area for 11.1%, and in the South at 51.5%. Ceftazidime resistance in the North was 38.7%, in the Central was 22.8%, and in the South was 58.8%. Cefepim resistance in the North was 36%, 17.8% in the Central, and 63.2% in the South. The results in the South were totally similar to that in the present study.
Antibiotic resistance of P. aeruginosa was varied over the years, with statistical significance after 1 year such as for ceftazidime and cefepime, they were with high rate of resistance in 2014, but this rate significantly was reduced one year after that (2015) (P<0.05). The monitor of antibiotic resistance every year once again proved necessary. The recent changes in the last two years have shown a more favourable trend in the selection of antibiotics for the treatment of pneumonia caused by this agent.
The tendency of selecting antibiotics for common bacteria
According to the antibiograms in 2016, the antibiotics were sensitive remarkably to 3 common bacteria types:
A. baumannii was sensitive to cefoperazone/sulbactam (92.9 %), polymyxin B (100%), and doxycycline (73.3 %).
Klebsiella spp was sensitive to cefoperazone/sulbactam (57.9%), amikacin (85,2%), and polymyxin B (100%).
Pseudomonas spp was sensitive to PTZ (85.7%), cefoperazone/sulbactam (69.2%), cefepim (58.8%), ceftazidime (58.8%), carbapenem: imipenem, meropenem (52.9%), amikacin (56.2%), and polymyxin B (94,1%).
The antibiotics such as cefoperazone/sulbactam and polymyxin B were highly sensitive to mentioned bacteria. Amikacin might be considered to combine for covering both Klebsiella spp and Pseudomonas spp.
The choice of first-line antibiotics to obtain high treatment effectiveness in the current multidrug- resistant periode is very difficult, depending on many factors. However, according to antibiotic sensibility for bacteria, these antibiotics may prefer to be selected if pneumonia might be suspected to be due to the respective bacteria.
CONCLUSIONS
By studying the distribution and antibiotic resistance of bacteria causing VAP at the Intensive Care Unit of Pham Ngoc Thach Hospital during 7 years, from 2010 to 2016, there are some conclusions from the present study:
Distribution of bacteria causing diseases
The three most commonly seen bacteria types over the years included A. baumannii, Klebsiella spp, and Pseudomonas spp. Other types of bacteria were reported with the low percentages.
A. baumannii always occupied a leading rate over all the years. This rate may be changed with statistical significance after 1-2 years.
The distribution of Klebsiella spp, Pseudomonas spp varied over years without the statistical significance.
Antibiotic resistance of bacteria
A. baumannii
Polymyxin B has not been recorded being resistant from 2012 to 2016.
A. baumannii was highly resistant to many antibiotics such as ceftazidime, cefepim, PTZ, ampicillin/sulbactam, imipenem, meropenem, ciprofloxacin, levofloxacin, amikacin, and gentamycin.
Cefoperazone/sulbactam was highly resistant in 2011 and 2012. However, the resistance rate in 2016 only reported at 7.1%.
Doxycycline resistance was increased gradually from 2012 to 2014, and then decreased significantly in the last two years. The resistance rate in 2016 was 26.7%.
Polymyxin B has not been recognized for resistance from 2012 to 2016.
Klebsiella spp
Klebsiella spp was highly resistant to ceftazidime, cefoperazone, cefepime, PTZ, ciprofloxacin, and levofloxacin.
The rate of cefoperazone/sulbactam and amikacin resistance was high, varied over the early years of study. In 2016, it was reduced to 42.1% and 14.8%, respectively.
The rate of imipenem and meropenem resistance was low from 2010 to 2012. However, this rate was increased remarkably from 2013 to 2016 with the resistance rate in 2016 of imipenem was 72.4% and meropenem was 71.4%.
Polymyxin B had not recorded resistant from 2014 to 2016.
Pseudomonas spp
Ceftazidime and cefepime were highly resistant, varied in the early periode of the study, then decreased significantly in the last two years. In 2016, the rate of resistance to this two antibiotics was 41.2%.
PTZ resistance rate was high in 2010 (67.5%), the lowest rate was in 2012 (28%). In 2016 the recorded resistance rate was 14.3%.
The rate of cefoperazone/sulbactam resistance was high in 2010 (75.9%), then varied; in 2016, the resistance rate was 30.8%.
The rate of levofloxacin, ciprofloxacin, and gentamycin resistance was high, varied from 2010 to 2014. This rate was decreased gradually. In 2016, resistance rate was ≥58.8%.
The rate of amikacin resistance was varied, decreased in the last 2 years. The resistance rate of 2016 was 43.8%.
Imipenem and meropenem resistance rate was very high for the first 3 years, then gradually reduced, in 2016, it was 47.1%.
Polymyxin B had not been recorded as antibiotic resistance from 2012 to 2015. However, in 2016, the resistance rate was 5.9%.
Tendency of selecting first-line antibiotics
For pneumonia suspected being due to by A. baumannii, the following antibiotics should be considered for the treatment: cefoperazone/sulbactam, polymyxin B, and doxycyclin.
For pneumonia suspected being due to Klebsiella spp, the following antibiotics should be considered for the treatment: cefoperazone/sulbactam, amikacin, and polymyxin B.
For pneumonia suspected being due to Pseudomonas spp, the following antibiotics should be considered for the treatment: cefepim, ceftazidime, PTZ, cefoperazone/sulbactam, carbapenem, amikacin, and polymyxin B.
Some antibiotics such cefoperazone/sulbactam and polymyxin B are highly sensitive to the 3 most common bacteria. Amikacin may be considered for covering both Klebsiella spp and Pseudomonas spp.
Recommendations
1.The bacterial distribution and antibiotic resistance should be monitored regularly at each intensive care unit.
2.Antibiotic effectiveness based on pharmacokinetics/pharmacodynamics should be optimized.
CONFLICT OF INTEREST
Non.
REFERENCES
1. http://emedicine.medscape.com/article/304836-overview#a2.
2. Infectious Diseases Society of America and the American Thoracic Society (2016), “Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia, Clinical Practice Guidelines”. Clinical Infectious Diseases, vol. 63, pp. 61–111.
3. Rosenthal, Victor D., Maki, Dennis G. and Jamulitrat, Silom (2009). "International Nosocomial Infection Control Consortium report, data summary from 2003 to 2008". American Journal of Infection Control, New York, Vol. 38, pp. 95-106.
4. Chung DR, Song JH et al (2011). “High prevalence of multidrug-resistant nonfermenters in hospital-acquired pneumonia in Asia”. Am J Respir Crit Care Med 2011; 184:1409-17.
5. Nguyen Thi Khanh Nhu et al (2014). “Emergence of carbapenem resistant A. baumannii as a major cause of VAP in intensive care unit patients at infectious desease hospital in southern Vietnam”. J Med Microbiol. 63 (Pt 10), pp. 1386-94.
TABLES
REFERENCES
1. http://emedicine.medscape.com/article/304836-overview#a2.
2. Infectious Diseases Society of America and the American Thoracic Society (2016), “Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia, Clinical Practice Guidelines”. Clinical Infectious Diseases, vol. 63, pp. 61–111.
3. Rosenthal, Victor D., Maki, Dennis G. and Jamulitrat, Silom (2009). "International Nosocomial Infection Control Consortium report, data summary from 2003 to 2008". American Journal of Infection Control, New York, Vol. 38, pp. 95-106.
4. Chung DR, Song JH et al (2011). “High prevalence of multidrug-resistant nonfermenters in hospital-acquired pneumonia in Asia”. Am J Respir Crit Care Med 2011; 184:1409-17.
5. Nguyen Thi Khanh Nhu et al (2014). “Emergence of carbapenem resistant A. baumannii as a major cause of VAP in intensive care unit patients at infectious desease hospital in southern Vietnam”. J Med Microbiol. 63 (Pt 10), pp. 1386-94.
ARTICLE INFO
DOI: 10.12699/jfvpulm.8.25.2017.29
Conflict of Interest
Non
Date of manuscript receiving
12/11/2017
Date of publication after correction
27/12/2017
Article citation
Pham L, Nguyen Nhu V, Nguyen Van S. Distribution and antibiotic resistance of bacterial induced ventilator - associated pneumonia at the intensive care unit . J Func Vent Pulm 2017;25(8):29-36