
 English
English
 French
French
Study of changes in the clinics, lung function and skin prick-test in asthmatic patients allergic to D.pteronyssinus under the effect of sublingual immunotherapy
Étude des changements de la clinique, la ventilation pulmonaire et le test cutané des patients asthmatiques allergiques au D.pteronyssinus
H. Dinh Thi Dieu1, T. Pham Van2, T. Phung Chi2
1: Hai Duong University of Medical Technology. Hai Duong, Viet Nam
2: Hai Phong University of Medicine and Pharmacy. Hai Phong, Viet Nam
Corresponding author
Pr. PHAM VAN Thuc
Hai Phong University of Medicine and Pharmacy. Hai Phong, Viet Nam
Email : pvthuc@yahoo.com
ABSTRACT
Introduction. First step in evaluation of the efficacy of allergic asthma to Dermatophagoides pteronyssinus (Dp) by using sublingual immunotherapy (SLIT) through the change of clinics, prick test, and lung ventilation is very necessary to confirm its validity.
Objective. To study the change of clinics, lung ventilation, prick test and the efficacy of SLIT in asthma to Dp treatment.
Method. Auto controlled follow-up study included 30 patients with allergic asthma to Dp at Haiphong Medical University Hospital. This is descriptive study method and all patients were selected by convenient sampling.
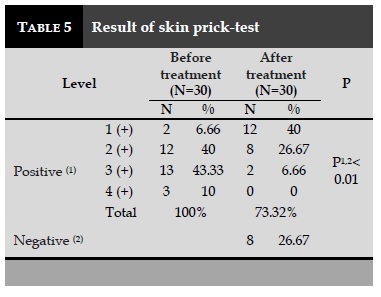
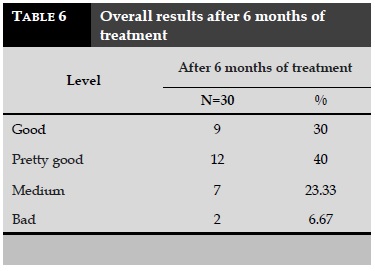
Results. After treatment, cough reduced from 80% to 26.67%; the number of outbreak ≥ 3 times/month from 60% to 6.67%; wheezing and sonorous rales from 86.67% to 23.34%. FEV1: before treatment 78,12±11.2 and after 92.04±16.02; PEF: before treatment 84.1±11.6 and after 91.08±14.9. Prick test: before treatments 100% were positive and after 26.67% negative. Common efficacy of therapy: Excellent, good were 70%, average 23.33%, and bad 6.67%.
Conclusion. SLIT is good in allergic asthma to Dp treatment.
KEYWORDS: Asthma, sublingual immunotherapy, Dermatophagoides pteronyssinus.
RÉSUMÉ
Introduction. La première étape de l’évaluation de l’efficacité de l’asthme allergique à Dermatophagoides pteronyssinus (Dp) en utilisant l’immunothérapie sublinguale (SLIT) par le changement de l’état clinique, le test cutané et la ventilation pulmonaire sont très nécessaire pour confirmer sa validité.
Objectif. Pour étudier le changement de la clinique, la ventilation pulmonaire, le prick-test et l'efficacité de l'SLIT dans le traitement de l'asthme à la Dp.
Méthode. Une étude de suivi auto-contrôlée a inclus 30 patients souffrant d'asthme allergique à Dp à l’Hôpital Universitaire de Médecine de Haiphong. C'est une méthode d'étude descriptive et tous les patients ont été sélectionnés par échantillonnage pratique.
Résultats. Après le traitement, la toux a été réduite de 80% à 26,67%; le nombre d’exacerbation ≥3 fois/mois de 60% à 6,67%; respiration sifflante et bronchiques de 86,67% à 23,34%. VEMS: avant le traitement 78,12±11,2 et après 92,04±16,02; DEP: avant traitement 84,1±11,6 et après 91,08±14,9. Prick test: avant les traitements, 100% étaient positifs et après 26,67% négatifs. Efficacité commune du traitement: excellente, bonne: 70%, moyenne de 23,33% et mauvaise de 6,67%.
Conclusions. L’SLIT était efficace dans l'asthme allergique au traitement Dp.
MOTS CLÉS: Asthme, immunothérapie sublinguale, Dermatophagoides pteronyssinus.
INTRODUCTION
Bronchial asthma is a common respiratory disease in many countries around the world and has a great impact on academic health and social activities. The cause of respiratory allergy is mainly Dermatophagoides pteronyssinus [1,2]. Currently, the treatment of allergic asthma basing on its pathogenesis is strongly studied and developed. The treatment of asthma causes by specific desensitization, or immune therapy (IT), is the best and only method to completely eliminate asthma.
In Vietnam, IT injection has been applied and achieved good results [1]. But injectable IT has a number of limitations, such as pain, swelling of the injection site, which must be carried out at the medical facility and carried out by experienced medical staff who are not favorable to patients living away from the hospital, medical facilities or on business trips. Recently, IT via sublingual drop (under the tongue) was introduced, the sublingual way overcome the disadvantages of IT by injection. However, the study evaluating the treatment outcome of these two methods is also being studied by some authors. As a result, initial clinical efficacy and a number of laboratory criteria for evaluating the IT are essential and useful. Therefore, we conducted this study for the following purposes: Assessment of clinical changes, lung function, and skin prick-test in patients with allergic asthma induced by D.pteronyssinus who was treated with sublingual immunotherapy (SLIT); Evaluation of the primary result of SLIT in asthmatic patients who were allergic with D.pteronyssinus.
METHODS
Study subjects
It was including 30 patients identified as asthma patients who were allergic with Dermatophagoides pteronyssinus allergen were selected for the study.
Location of study: Department of Immunology-Clinical Allergy of Hai Phong University Hospital.
Period of study: from September 2013 to May 2017.
Inclusion criteria
• The patients who were selected into the study group including those with diagnosis of asthma allergic with Dermatophagoides pteronyssinus allergens.
• Asthmatic patients who were selected with asthma stage I, II according to GINA 2012 classification.
• Age: 16-55 years (in calendar year).
• Gender: including both men and women, regardless of gender.
• Duration of asthma: 1 year or more.
Exclusion criteria
• Asthmatic patients who were not allergic with D. pteronyssinus.
• Patients who were or expecting in pregnancy during treatment.
• Patients with co-morbidity conditions.
• Patients with combined autoimmune disease.
• Patients suffering from bacterial infections in the mouth such as: tongue inflammation, gingivitis, …
• For patients who were treated within the previous 2 weeks with antihistamines, corticosteroids (topical or systemic), cell membrane stabilizers (eg, cromoglycate), adrenergic stimulants (for example, salbutamol), or general medical allergy medications, these patients were also given a 2-week break and then selected into the study group if they were eligible.
• Patients do not accept IT treatment.
Methods
Study design
It was a prospective, descriptive, and longitudinal study.
Study method
Clinical data: gender, age, occupation, duration of illness.
Asking for a medical history of allergy: based on the health care checking form.
Clinical examination for respiratory system.
Time of clinical study: before IT and each time of IT treatment.
Method of IT treatment
Conducted at the Department of Immunology-Clinical Allergy of Hai Phong University Hospital.
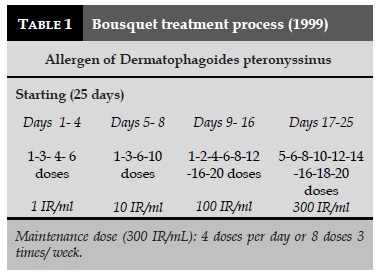
D.pt antigen, produced by the Central Institute of ENT, concentrations of 1 IR/mL, 10 IR/mL, 100 IR/ mL and 300 IR/mL. Technique: according to the procedure of Bousquet [5] (Table 1).
The treatment procedure was applied at Department of Immunology-Clinical Allergy of Hai Phong University Hospital. During the course of treatment, we monitored the patients and documented the status of each patient after 3 months and 6 months.
Spirometry was done by Spirolab II (Germany).
Skin prick-test was followed Sullivan’s technique [7].
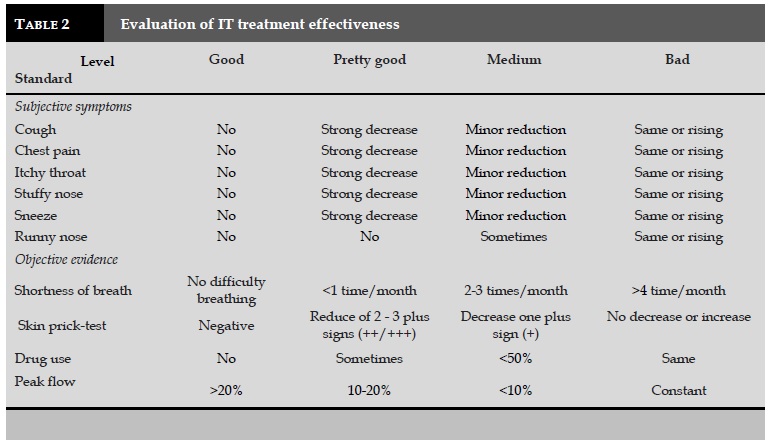
Evaluation after 6 months of treatment of SLIT according to the authors Vu and Trinh [2].
Data processing
Data obtained during the study were processed by EpiInfo 6.04, SPSS 14.0 and other biostatistical methods.
RESULTS
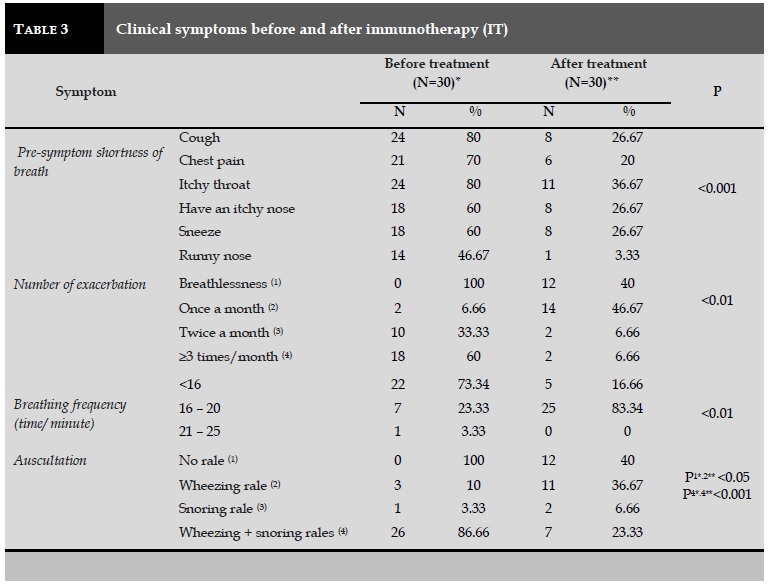
Changes in some clinical symptoms (Table 3)
Symptoms before treatment: cough (80%), itching of the throat (80%), chest pain (21%), nasal itching (60%), sneezing (60%). After 6 months of treatment, these symptoms tended to decrease markedly, with P<0.001 (Table 3). In particular, the number of exacerbations of patients was decreased from more than 3 times per month (60%) to once a month (46.67%) and 12 patients without difficulty breathing.
On physical examination of patients with asthma, the results showed that the patient respiratory rate was 16-20 times/min (83.34%). When auscultation to the lungs, the signs such as wheezing and snoring rales were decreased from 86.66% to 23.33% and most patients have only wheezing rale (36.67%), snoring rale (6.66%), and 12 patients without rales after 6 months of treatment.
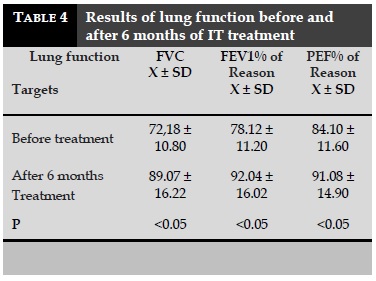
Changes in lung function parameters
When studying the change in lung function before and after treatment, the results showed that prior to treatment, FVC and FEV1% were significantly lower than normal, indicating the limited ventilation. After 6 months of treatment, FVC, FEV1 and PEF increased significantly compared to pretreatment (P <0.05; Table 4).
Result of skin prick-test before and after treatment
In the present study, the results showed that 100% positive skin test with D.pteronyssinus, mainly from 2 (+) to 4 (+), accounted for 93.34%. After 6 months of treatment, eight patients returned to negative skin test and 1% with (+) positive for progression, no patient had positive 4 (+) (Table 5).
Overall results after 6 months of IT treatment
After 6 months of IT treatment for asthmatic patients who were allergic with D.pteronyssinus, the rate is good and pretty good was 70%, the medium rate was 23.33%, and bad was less than 6.67% (Table 6).
DISCUSSION
To evaluate the effectiveness of immuno therapy in asthmatic patients, we based on the changes in both clinical and immunological parameters before and after treatment. We noticed that there was a lot of symptoms before the appearance of shortness of breath, the most common is cough (80%), itchy throat (80%), chest pain (70%), nasal itching (60% %), sneezing (60%), and runny nose (46.67%). These symptoms often coexist in a dyspnea, but the initial signs are usually felt by the patient, while other signs appear next. Most of these signs were reduced by 33 to 55% in compared with the original, with the only symptom of a runny nose in only one patient (3.33%). The changes in these symptoms were statistically significant (P<0.05).
Thus, the ability of the immune response to external stimuli to the respiratory tract increases. It proves that the local hypersensitivity of these patients is moving towards the normal human. Ameae [4] also found a marked reduction in clinical symptoms, especially dyspnea in the IT group treated with D.pteronyssinus allergens compared to the control group. On the basis of remission of dyspnea, other functional signs were also better after 6 months of treatment. Subjective symptoms are markedly reduced by the patient, which improves patient morale and improves trustworthiness with this treatment.
When looking at the clinical symptoms before and after treatment of IT, the results showed that: before treatment, the patients had difficulty breathing from 2 to ≥3 times per month, accounting for 93%. During asthma crisis, the auscultation with both wheezing and snoring rales was 86.66%, mainly with expiratory shortness of breath (86.66%) and with thinning of white mucus (80%). All of these signs are indicative of inflammation, bronchospasm, and bronchial asthma. In particular, the number of patients with asthma was closely correlated with some daily activities such as cleaning (66.66%) and shading (66.66%).
Following specific IT treatment, the number of patient with exacerbations in the month was tended to decrease significantly (P<0.01). The number of patients with exacerbations for two times a month and three times a month was significantly reduced to 6.66% and 6.66%, respectively, compared with pretreatment (P<0.001). Most patients present only one difficulty per month, accounting for 46.67%.This indicates that the level of difficulty breathing of patients tends to be milder than before treatment. In particular, the auscultation of the lungs from the patients showed that the rate of wheezing and snoring rales was significantly reduced after treatment (86.66% to 23.33%) with P<0.001; 12 patients without dyspnea and one did not hear the wheezing when the physical examination is 40%. This observation is also consistent with changes in respiratory frequency, number of dyspnea and functional signs of the patient after treatment. The remission of clinical symptoms before and after IT treatment with D.pteronyssinus has been confirmed by many other authors [4,5,9] and is also a sign for physicians and patients being aware of the treatment process.
Study on changes in respiratory function before and after treatment with IT showed that FVC and FEV1 were lower than normal, indicating limited disorder of ventilation. After 6 months of IT treatment, these parameters were increased significantly (P<0.05). Apart from the two parameters, the peak flow was also significantly improved after treatment with P <0.05.
Maestrelli [9] studied 72 patients with asthma who were allergic with house dust mites, after 1 year of IT treatment, the peak flow (PEF) of patients in both morning and evening was improved, while significantly reducing the need for medication for asthma crisis. Although our patients were only followed for 6 months after treatment, the results of FVC, FEV1 and PEF were statistically significant. This is also consistent with the changes in clinical symptoms that are no longer dyspnea or dyspnea significantly reduced in both the severity and intensity in a month.
Skin prick-test is a basic and a first test for diagnosis and treatment of allergic conditions. According to many authors, this test has greater reliability than intradermal test due to less false positive cases [1,6]. Chou et al. [6] studied the specific-IgE in diagnosis of asthmatic children in Taiwan found that patients with IgE-positive with allergens, then skin prick-test with these allergens were also positive. In the present study, all patients who were clinically examined and tested for allergens, then included in this study if the skin prick-tests were also positive with thw same allergens.
Patients with asthma prior to IT treatment had a 100% positive skin prick-test with D.pteronyssinus, mainly ranging from 2 (+) to 4 (+), suggesting the sensitivity to D.pteronyssinus accounts for 93.34%. After treatment, 26.67% of patients had negative skin prick-test and progressed to the positivity with 1 (+) to 3 (+), accounted for 73.32%; there was no patient with skin prick-test was counted for 4 (+). Compared with clinical symptoms of dyspnea, we also found a consistent remission. Ferrer et al. demonstrated that IT treatment with D.pteronyssinus after 6 months also found a marked improvement in clinical and decreased the levels of skin prick-test positivity [8].
The study realized by Wang et al. also found out that in patients without recurrent dyspnea, the intensity of skin prick-test response was reduced at the end of the IT phase, and in patients with recurrent apnea, the skin prick-test did not change [10]. Trinh [2] and Pham [3] showed that in patients treated with IT with house dust mites also obtained appropriate remission between clinical symptoms and the positivity of skin prick-test.
Many authors have suggested that skin prick-test can be used to predict the efficacy of IT treatment [1,6,8] because this is a simple test, easy to do, can be widely applied in the community. Furthermore, the main purpose of the skin prick-test is to detect the presence of specific IgE of the allergen to be tested. Thus, when the level of positivity decreases after treatment, it also suggests that the specific IgE concentration of D.pteronyssinus present on the mast cells under the skin also decreases.
CONCLUSION
After 6 months of treatment the clinical symptoms decreased markedly, the number of exacerbation was also reduced in asthmatic patients treated by immunotherapy. In addition, the lung function parameters were improved beside the improvement of the positivity of skin prick-test. Thus, immunotherapy is an effective treatment for asthmatic patients who are allergic with D.pteronyssinus.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
REFERENCES
1. Phan Quang Doan, Nguyen Nang An. Application of heterologous dust for diagnosis and treatment of asth-ma bronchial asthma. Scientific research, 1995-1996, Bach Mai Hospital, 1996;215-222.
2. Trinh Manh Hung. The results of diagnosis and treat-ment of bronchial asthma, University of Medicine, Hanoi, 2000.
3. Pham Van Thuc, Phung Minh Son. Initial application of specific hypersensitivity in patients with asthma bronchial asthma in Hai Phong, Hai Phong - Rouen, 1998;348,95-98.
4. Ameal A, Vega-Chicote JM, Fernandez S, Miranda A, Carmona MJ, Rondon MC, Reina E, Garcia-Gonzalez JJ. Double blind and placebo-controlled study of the efficacy and safety of a modified allergen extract of Dermatophagoides pteronyssinus in allergic asthma. Department, Hospital 'Carlos Haya', Malaga, Spain. 2005;60(9): 178-83.
5. Sublingual-swallow immunotherapy in patients with asthma due to house-dust mites: a double-blind, pla-cebo-controlled study. Allergy 1999; 54: 249-260.
6. Chou TY, Wu KY, Shieh CC, Wang JY. The clinical efficacy of in vitro allergen-specific IgE antibody in the diagnosis of allergic children with asthma. Acta Paedi-atr Taiwan. 2002;43(1): 35-9.
7. Sullivan TJ, Wedner HJ, Shatz GS, Yecies LD, Parker CW. Skin testing to detect penicillin allergy. J Allergy Clin Immunol. 1981;68(3):171-80.
8. Ferrer A, Garcia - Selles J. Significant improvement in symtoms, skin test and specific bronchial reactivity after 6 months of treatment with a depigmented, pol-ymerized extract of D. pteronyssinus and D. farinae". J. Investig Allergol clin immunol. 2003;13(4):251-51.
9. Maestrelli P, Zanolla L, Pozzan M, Fabbri LM; Regione Veneto (2004), Effect of specific immunotherapy add-ed to pharmacologic treatment and allergen avoidance in asthmatic patients allergic to house dust mite. J Al-lergy Clin Immunol. Apr;2004;113(4): 643-9.
10. Wang H, Lin X, Hao C, Zhang C, Sun B, Zheng J, Chen P, Sheng J, Wu A, Zhong N. A double-blind, placebo-controlled study of house dust mite immunotherapy in Chinese asthmatic patients. Guangzhou Institute of Respiratory Diseases, Guangzhou, China.Feb; 2006;61 (2):191-7.
TABLES
REFERENCES
1. Phan Quang Doan, Nguyen Nang An. Application of heterologous dust for diagnosis and treatment of asth-ma bronchial asthma. Scientific research, 1995-1996, Bach Mai Hospital, 1996;215-222.
2. Trinh Manh Hung. The results of diagnosis and treat-ment of bronchial asthma, University of Medicine, Hanoi, 2000.
3. Pham Van Thuc, Phung Minh Son. Initial application of specific hypersensitivity in patients with asthma bronchial asthma in Hai Phong, Hai Phong - Rouen, 1998;348,95-98.
4. Ameal A, Vega-Chicote JM, Fernandez S, Miranda A, Carmona MJ, Rondon MC, Reina E, Garcia-Gonzalez JJ. Double blind and placebo-controlled study of the efficacy and safety of a modified allergen extract of Dermatophagoides pteronyssinus in allergic asthma. Department, Hospital 'Carlos Haya', Malaga, Spain. 2005;60(9): 178-83.
5. Sublingual-swallow immunotherapy in patients with asthma due to house-dust mites: a double-blind, pla-cebo-controlled study. Allergy 1999; 54: 249-260.
6. Chou TY, Wu KY, Shieh CC, Wang JY. The clinical efficacy of in vitro allergen-specific IgE antibody in the diagnosis of allergic children with asthma. Acta Paedi-atr Taiwan. 2002;43(1): 35-9.
7. Sullivan TJ, Wedner HJ, Shatz GS, Yecies LD, Parker CW. Skin testing to detect penicillin allergy. J Allergy Clin Immunol. 1981;68(3):171-80.
8. Ferrer A, Garcia - Selles J. Significant improvement in symtoms, skin test and specific bronchial reactivity after 6 months of treatment with a depigmented, pol-ymerized extract of D. pteronyssinus and D. farinae". J. Investig Allergol clin immunol. 2003;13(4):251-51.
9. Maestrelli P, Zanolla L, Pozzan M, Fabbri LM; Regione Veneto (2004), Effect of specific immunotherapy add-ed to pharmacologic treatment and allergen avoidance in asthmatic patients allergic to house dust mite. J Al-lergy Clin Immunol. Apr;2004;113(4): 643-9.
10. Wang H, Lin X, Hao C, Zhang C, Sun B, Zheng J, Chen P, Sheng J, Wu A, Zhong N. A double-blind, placebo-controlled study of house dust mite immunotherapy in Chinese asthmatic patients. Guangzhou Institute of Respiratory Diseases, Guangzhou, China.Feb; 2006;61 (2):191-7.
ARTICLE INFO
DOI: 10.12699/jfvpulm.9.28.2018.47
Conflict of Interest
Non
Date of manuscript receiving
Date of publication after correction
Article citation
Dinh Thi Dieu H, Pham Van T, Phung Chi T. Study of changes in the clinics, lung function and skin prick-test in asthmatic patients allergic to D.pteronyssinus under the effect of sublingual immunotherapy . J Func Vent Pulm 2018;27(9):47-52