
 English
English
 French
French
Methods for assessing alertness and level of vigilance in patients with obstructive sleep apnea
Méthodes d'évaluation de la vigilance et du niveau de vigilance chez les patients atteints d'apnée obstructive du sommeil
K. Bui-Diem1, D. Do Van1, S. Duong-Quy2,3
1: University of Medicine and Pharmacy at Ho Chi Minh City. Vietnam
2: Lam Dong Medical College. Dalat, Vietnam
3: Penn State Medical College. USA
Corresponding author:
Pr. Sy DUONG-QUY
Lam Dong Medical College, Dalat—Vietnam. Penn Sate University, USA
E-mail: sduongquy.jfvp@gmail.com
DOI: 10.12699/jfvpulm.11.35.2020.1
ABSTRACT
Sleep apnea is a sleep disorder which has periods of apnea or hypopnea, causing hypoxia, and associated with other systemic disorders, such as excessive daytime sleepiness, poor concentration, memory loss, metabolic disorders, uncontrolled blood pressure, blood glucose, ... Obstructive sleep apnea (OSA) is the most common in 3 types of sleep apnea, accounting for 7-24% of population.
OSA is an important risk factor for decreased concentration and affects work performance, especially associated with accidents at work or in traffic. The Multiple Sleep Latency Test (MSLT) and Maintenance of Wakefulness Test (MWT) are used to assess the ability of alertness and wakefulness of the patients. Some states in the United States use this test to check whether employees or drivers or pilots are alert enough to work. In addition, the Vigilance Test (VT) is used to evaluate the ability of a person's vigilance, also related to the ability to maintain awakening and daytime sleepiness.
Many studies have reported that daytime sleepiness, concentration, and awakening parameters in OSA patients are reduced compared to healthy individuals and improved after CPAP treatment by these tests.
KEYWORDS: Obstructive sleep apnea; Multiple leep Latency Test; Maintenance of Wakefulness Test; Vigilance Test; Psychomotor Vigilance Test.
RÉSUMÉ
L'apnée du sommeil est un trouble du sommeil qui s'accompagne de périodes d'apnée ou d'hypopnée, provoquant une hypoxie, et associé à d'autres troubles systémiques, tels qu'une somnolence diurne excessive, une faible concentration, une perte de mémoire, des troubles métaboliques, une tension artérielle non contrôlée, une glycémie, ... Obstructive l'apnée du sommeil (AOS) est la plus courante dans 3 types d'apnée du sommeil, représentant 7 à 24% de la population.
L'AOS est un facteur de risque important de diminution de la concentration et affecte les performances au travail, en particulier lors d'accidents du travail ou de la circulation. Le test de latence de sommeil multiple (MSLT) et le test de maintien de la vigilance (MWT) sont utilisés pour évaluer la capacité de vigilance et d'éveil des patients. Certains États des États-Unis utilisent ce test pour vérifier si les employés, les conducteurs ou les pilotes sont suffisamment alertes pour travailler. De plus, le test de vigilance (VT) est utilisé pour évaluer la capacité de vigilance d'une personne, également liée à la capacité à maintenir le réveil et la somnolence diurne.
De nombreuses études ont rapporté que la somnolence diurne, la concentration et les paramètres d'éveil chez les patients atteints d'AOS sont réduits par rapport aux individus en bonne santé et améliorés après un traitement CPAP par ces tests.
MOTS CLÉS: Apnée obstructive du sommeil; Test de latence du sommeil multiple; Test de maintien de l'état de veille; Test de vigilance; Test de vigilance psychomotrice.
INTRODUCTION
Sleep apnea is defined as a condition in which there are repeated sleep apnea or hypopnea that cause arousals, fragmented sleep, and decreased oxygen saturation in the blood.
Sleep apnea has 3 types:
• Obstructive sleep apnea (OSA) is sleep apnea due to obstruction of the upper airway, there are efforts of the breathing muscles, but no airflow. This is the most common form of sleep apnea.
• Central sleep apnea (CSA) is a condition in which there are no signals from the brain to the respiratory muscles leading to no airflow.
• Mixed sleep apnea: including the two above reasons.
Obstructive sleep apnea (OSA) – Diagnosis
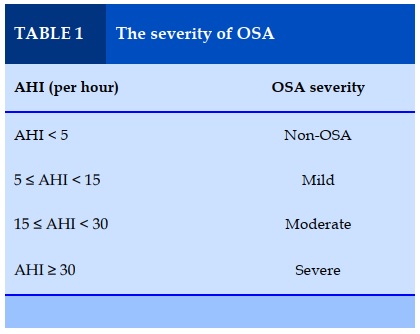
According to the ICSD-3, OSA syndrome is defined by 1 of 2 following definitions [1]
Definition 1: The polysomnography (PSG) or home sleep testing (HSAT) result has AHI ≥ 5, and Patient has at least 1 of below symptoms: documents symptoms of excessive daytime sleepiness, impaired cognition, mood disorders or insomnia, or documented hypertension, ischemic heart disease, or history of stroke
Definition 2: AHI ≥ 15, regardless of symptoms or co-morbidity. If the PSG or HSAT result is accompanied by CSA or mixed sleep apnea, an OSA ratio of more than 50% will confirm the diagnosis as OSA [2]
Obstructive sleep apnea (OSA) – Treatment
The goal of OSA treatment is to improve OSA symptoms, sleep quality, bring AHI and blood oxygen saturation to normal levels.
OSA needs to be approached as a chronic disease and requires long-term treatment, coordinated with many specialties. As recommended by the AASM and the American College of Physicians (ACP), all OSA patients should be initially treated with positive airway pressure (PAP), which is the standard treatment for moderate to severe OSA patients.
PAP is a safe, effective treatment that causes very little complications. There are no absolute contraindications to PAP, but caution should be exercised in situations with relative contraindications such as recurrent or untreated pneumothorax, unstable nasal bleeding, unstable facial fractures, surgery, or extensive burns in the face [3,4] .
For mild to moderate OSA patients who do not want to take PAP or fail with PAP, the mandibular advancement device (MAD) may be better adhered. Careful assessment of the patient is necessary to choose the appropriate type and size of instrument and the physician should guide the patient to monitor side effects [5].
Surgery may be available to patients with surgical corrective upper airway obstruction, for example tonsillar hypertrophy or craniofacial abnormality. Uvulopalatopharyngoplasty (UPPP) is one of the most commonly used methods.
UPPP alone is not recommended for patients with OSA with moderate to severe illness. UPPP cures OSA with a very low success rate, many negative consequences (painful, choking, high recurrence rate) and reduces the effectiveness of PAP [4,6].
In addition, lifestyle counseling can be prescribed for all OSA patients, including: weight loss, stopping smoking, changing sleep position (lying on one side), stopping drinking alcohol, using some drugs that inhibit the central nervous system with caution (such as benzodiazepines, barbiturates and its agonists, antiepileptic drugs, antidepressants, antihistamines, and addictive drugs) [5].
METHODS FOR ASSESSING ALERTNESS AND LEVEL OF VIGILANCE
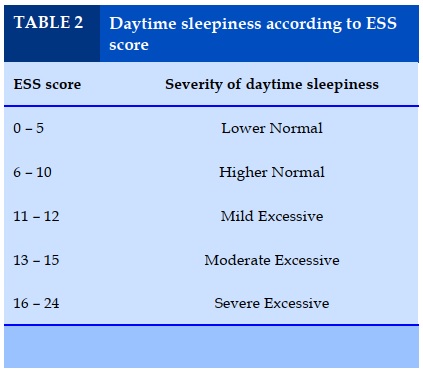
Epworth Sleepiness Scale (ESS)
The ESS is a patient’s self-administered scale and is often used to subjectively measure daytime sleepiness. The Epworth questionnaire consists of 8 questions, related to the ability to drowsiness in sedentary situations, and is evaluated by patients on a Likert scale of 0 to 3 points for each question. The higher the Epworth total score, the higher that person’s average sleep propensity in daily life [7].
Multiple Sleep Latency Test (MSLT)
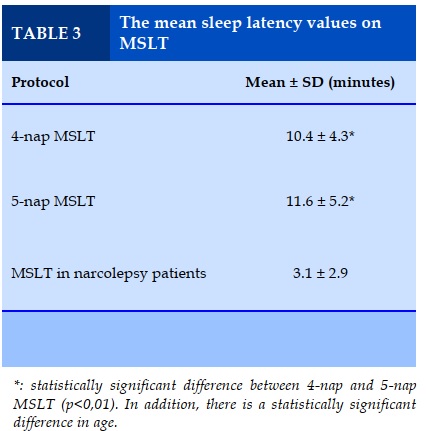
MSLT is an objective method of measuring excessive daytime sleepiness and is the main method to diagnose narcolepsy, primary hypersomnia and other causes of excessive sleepiness. MSLT measures the physiological tendencies that a person sleeps while in a quiet environment during the day.
MSLT consists of 4 or 5 naps, every 2 hours, throughout the day. Sleep stage is determined by EEG, EOG, chin EMG and ECG channels. At each session, the patient was given 20 minutes to take a nap. Before performing MSLT, the patient should have an PSG at the night before to evaluate other causes of drowsiness and ensure that patients get enough sleep the night before MSLT. Alternatively, patients may be assessed with a sleep log or an actigraphy for 1 to 2 weeks prior to MSLT, as lack of sleep can invalidate MSLT results.
Medications can also affect the outcome, for example some REM-inhibiting antidepressants or stimulants (such as caffeine). Therefore, if these drugs are intermittent, they should be discontinued at least 15 days before MSLT or 5 half-cycles to avoid the rebound effect of discontinuation. Urine screening for certain medications or narcotics should be done in the morning before MSLT to ensure the therapy is not affected by the substance.
In MSLT, sleep latency was measured at each nap and finally used to calculate average sleep latency for the whole treatment. The sleep potential is determined by the time from the beginning of the test to the onset of sleep (at any stage of sleep) on the EEG. The shorter the sleep duration, the more asleep and difficult for the patient to stay awake. In addition, the results also record the presence or absence of REM sleep via the sleep-onset REM (SOREM).
*: statistically significant difference between 4-nap and 5-nap MSLT (p<0,01). In addition, there is a statistically significant difference in age.
Maintenance Wakefulness Test (MWT)
MWT is used to evaluate a patient's ability to wake up during the day. Some states in the United States use this test to check whether employees or drivers or pilots are alert enough to work.
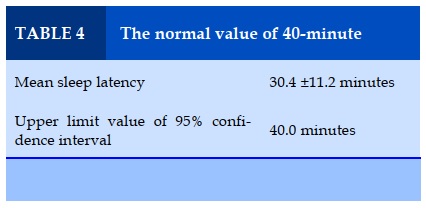
In contrast to MSLT, during MWT, the patient was asked to try to stay awake for 4 sessions, each lasting 40 minutes, every 2 hours. MWT's parameters were recorded through EEG, EOG, chin EMG channels. Patients are reclined in bed, in the sleep lab, and are not allowed to read books or watch television or do other activities during the test.
Before the MWT, the patient did not need a PSG or a sleep log. On the day of the MWT, patients were instructed not to take caffeinated foods or drugs.
The MWT recorded the duration of the awakening period (through sleep latency, if the patient slept) during 40 minutes, in all 4 sessions [8].
During the MWT, the patient cannot attempt to falsify the expected outcome (the patient is asked to try to stay awake, if health does not allow, they cannot attempt to prolong sleep latency). Meanwhile, the main expectation of MSLT is short sleep latency (the patient is asked to try to sleep, the results may vary subjectively).
Vigilance Test
The Vigilance Test (VT) is used to assess a person's ability to alert. Most types of VT try to mimic a tedious situation by having the test person observe bright spots on screens or ships on the horizon. Loss of vigilance, when faced with a non-stimulating task, is particularly relevant in patients with sleep disturbances and arousals. Theoretically, the monotony of the task helps to assess the underlying drowsiness [9]. Like MWT, people with VT cannot fake to have results beyond their maximum capacity. They may try to do bad ("faking bad") but cannot "fake good".
However, the difficulty distinguishing between a lack of alertness caused by drowsiness and poor concentration may be a confounding factor in VT results. Fortunately, drowsiness and poor concentration often coexist; therefore, monotonous, prolonged, regular-paced tasks are very sensitive to insomnia and sleep disruption. The landmark studies in the 1970s, known as the Walter Reed experiments (named after the institute where the study was conducted), documented the effects of sleep deprivation on VT performance [9].
There are many types of vigilance tests, but the Psychomotor Vigilance Test (PVT) developed by Dinges et al. is currently the best proven and most widely used. PVT is a test of recognizing signals by images, about 10 minutes long, repeated 3-4 times a day, done by computer or mobile device. Results of response latency to visual stimuli (for example, the time it takes from when a light spot appears on the screen until a person presses a button to confirm it is visible).
Slowing and lapsing correlated with MSLT results. In addition, PVT results have been reported in many target groups, including normal controls, volunteers with insomnia and patients with severe sleep disturbances. PVT is highly sensitive to intrinsic measurement of individuals, with pre- and post-test design. However, the standard PVT data is still limited, making it difficult to compare between different subjects.
Another VT commonly used in sleep research is the OSLER (Oxford Sleep Resistance Test). The OSLER test method is quite similar to MWT. It is also done in 40-minute intervals, 2 hours apart, for a total of 3-4 times a day. However, instead of using EEG, ECG, and chin EMG, OSLER requires patients to recognize visual signals similar to PVT to evaluate the number of false responses. The standard data of this method have not been studied much.
EFFECTS OF OSA ON ABILITY TO MAINTAIN ALERTNESS AND LEVEL OF VIGILANCE
Compared to the general population, OSA patients have higher daytime drowsiness, difficulty maintaining awakening, impaired mood and quality of life, impaired mental function, including psychomotor function, memory, and vigilance.
Some of these impairments may improve after CPAP treatment [10].
OSA not only affects sleep, but also affects daytime alertness and work performance. Untreated OSA leads to daytime drowsiness, difficulty staying awake, poor concentration, poor reflexes, especially important for high-precision jobs or driving on the road, thus may cause work accidents or traffic accidents.
Studies in South Korea and Saudi Arabia show that 29 to 35.5% of commercial truck drivers have a high risk of sleep apnea, through subjective assessments such as Berlin and Eprworth questionnaires [11,12].
In the United States, driver drowsiness accounts for 16.5% of fatal accidents and 13.1% of accidents lead to hospitalization [13].
Federal Motor Carrier Safety Administration (FMCSA) requires that a person with a clinical diagnosis or medical history interfering with the ability to drive safely will not be licensed to operate a commercial motor vehicle, including OSA syndrome. However, once they are successfully treated and followed, they will be re-licensed [14].
In the study of Jackson et al. in 2018 [10], compared with a normal sample in the community, those with OSA were significantly more sleepy, had impaired mood and quality of life, and had impaired mental function, especially psychomotor function, working memory and vigilance.
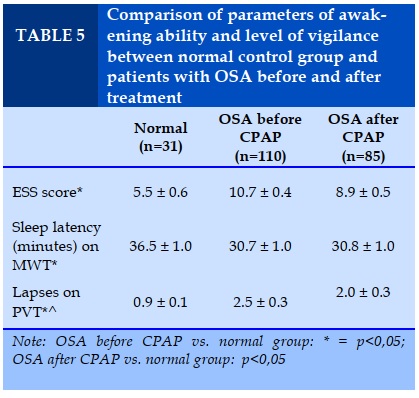
The OSA group before CPAP treatment had more daytime sleepiness (demonstrated by high ESS score and short sleep latency) and the lapses on PVT were significantly higher than the control group.
This study in turn selected a cut-off for sleep latency (on MWT) of 36.5 minutes and an ESS score of ≥ 11 to objectively and subjectively defining daytime sleepiness.
After CPAP treatment, ESS scores and lapsing scores on PVT improved significantly.
In 2017, Martinez-Nicolas et al. reported the efficacy of CPAP on 30 patients with sleep disturbance, AHI> 15/ hour, with excessive daytime drowsiness or drug-resistant hypertension. The results showed that parameters on MWT were significantly improved after using CPAP. The average sleep latency was 23.5 ± 2.6 minutes before CPAP, compared to 34.0 ± 2.0 minutes after CPAP [15].
The Yun Li et al study on 58 untreated OSA patients showed that a high ESS score (extensive daytime sleepiness) was significantly associated with higher lapses and slower response times in PVT. But there is no relationship between PVT and MSLT [16].
A study in Japan, conducted by Tanno et al., on 1,508 people in the community, then compared a normal control group and patients with sleep-disordered breathing (SDB), showed patients with SDB have worse PVT scores than the control group. The lowest SpO2 during the night was related to the number of lapses on PVT (the lower the SpO2, the more number of lapses), but not to the reaction time on PVT[17].
Recent studies of OSA show that the decrease in SpO2 is positively correlated with slow response on PVT. In contrast, high AHI and high arousals were not associated with decreased performance on PVT. This result shows that OSA severity should not only be assessed by the AHI alone, or the need to change the OSA diagnostic threshold through AHI [18,19] .
A 1-year prospective study on psychomotor performance and alertness in severe OSA patients with Complex Reactionmeter Drenovac (CRD) assay showed significant improvement in cognitive and psychomotor performance in OSA patients following CPAP treatment [20].
According to the above studies, most of the parameters of the ability to maintain awakening and the degree of realism improved significantly after 1-3 months using CPAP,[10][20][16] Longer periods of time may lead to a higher risk of loss to follow-up in the study.
CONCLUSION
There are some potential tests for measuring the wakefulness and vigilance in OSA patients and assessing the effect of CPAP treatment, including MSLT, MWT, and PVT tests. The choice of test type is up to the research purpose.
MSLT has good value in evaluating sleep latency in patients with hypersomnia, especially narcolepsy vs. primary hypersomnia. MWT is significant in assessing the ability to remain awake, especially in assessing disease consequences and treatment effectiveness. Besides, PVT helps to assess the underlying drowsiness, can simulate some real-life situations.
CONFLICT OF INTEREST
Non
REFERENCES
1. Sateia MJ. International classification of sleep disorders-third edition highlights and modifications. Chest 2014; 146:1387–1394.
2. Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: An American academy of sleep medicine clinical practice guideline. J Clin Sleep Med 2017; 13:479–504.
3. Qaseem A, Holty JEC, Owens DK, Dallas P, Starkey M, Shekelle P. Management of obstructive sleep apnea in adults: A clinical practice guideline from the American college of physicians. Ann Intern Med 2013; 159:471–483.
4. Patil SP, Ayappa IA, Caples SM, John Kimoff R, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: An American academy of sleep medicine systematic review, metaanalysis, and GRADE assessment. J Clin Sleep Med 2019; 15:301–334.
5. Kryger MH, Roth T (Tom). Principles and Practice of Sleep Medicine 2016. 1030–1211.
6. American Academy of Sleep Medicine. Evaluation, Management and Long-Term Care of OSA in Adults Clinical Algorithm. Am Acad Sleep Med 2015; 1–6
7. About the ESS – Epworth Sleepiness Scale. https:// epworthsleepinessscale.com/about-the-ess/. Accessed 13 Aug 2020.
8. Littner MR, Kushida C, Wise M, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep 2005; 28:113–121.
9. Kryger M, Roth T, Dement WC (eds). Principles and Practice of Sleep Medicine 2017. https://doi.org/10.1016/c2012-0-03543-0.
10. Jackson ML, McEvoy RD, Banks S, Barnes M. Neurobehavioral impairment and CPAP treatment response in mild-moderate obstructive sleep apnea. J Clin Sleep Med 2018; 14:47–56.
11. Alahmari MD, Alanazi TM, Batawi AA, Al-Osaimi EA, Alrabeeah S, Jebakumar Z, Olaish AH, Almeneessier AS, BaHammam AS. Sleepy driving and risk of obstructive sleep apnea among truck drivers in Saudi Arabia. Traffic Inj Prev 2019; 20:498–503.
12. Sunwoo JS, Shin DS, Hwangbo Y, Kim WJ, Chu MK, Yun CH, Jang T, Yang KI. High risk of obstructive sleep apnea, insomnia, and daytime sleepiness among commercial motor vehicle drivers. Sleep Breath 2019; 23:979–985.
13. Tefft BC. Prevalence of motor vehicle crashes involving drowsy drivers, United States, 1999-2008. Accid Anal Prev 2012; 45:180–186.
14. Driving When You Have Sleep Apnea | FMCSA. https://www.fmcsa.dot.gov/driver-safety/sleep-apnea/driving-when-you-have-sleep-apnea. Accessed 4 Aug 2020.
15. Martinez-Nicolas A, Guaita M, Santamaría J, Montserrat JM, Rol MÁ, Madrid JA (2017) Circadian impairment of distal skin temperature rhythm in patients with sleep-disordered breathing: The effect of CPAP. Sleep. https://doi.org/10.1093/sleep/zsx067.
16. Li Y, Vgontzas A, Kritikou I, Fernandez-Mendoza J, Basta M, Pejovic S, Gaines J, Bixler EO. Psychomotor vigilance test and its association with daytime sleepiness and inflammation in sleep apnea: Clinical implications. J Clin Sleep Med 2017; 13:1049–1056.
17. Tanno S, Tanigawa T, Maruyama K, Eguchi E, Abe T, Saito I. Sleep-related intermittent hypoxia is associated with decreased psychomotor vigilance in Japanese community residents. Sleep Med 2017; 29:7–12.
18. Korkalainen H, Töyräs J, Nikkonen S, Leppänen T (2019) Mortality-risk-based apnea–hypopnea index thresholds for diagnostics of obstructive sleep apnea. J Sleep Res. https://doi.org/10.1111/jsr.12855.
19. Kainulainen S, Duce B, Korkalainen H, Oksenberg A, Leino A, Arnardottir ES, Kulkas A, Myllymaa S, Töyräs J, Leppänen T. Severe desaturations increase psychomotor vigilance task-based median reaction time and number of lapses in obstructive sleep apnoea patients. Eur Respir J 2020. https://doi.org/10.1183/13993003.01849-2019.
20. Pecotic R, Dodig IP, Valic M, Galic T, Kalcina LL, Ivkovic N, Dogas Z. Effects of CPAP therapy on cognitive and psychomotor performances in patients with severe obstructive sleep apnea: a prospective 1-year study. Sleep Breath 2019; 23:41–48.
TABLES
REFERENCES
1. Sateia MJ. International classification of sleep disorders-third edition highlights and modifications. Chest 2014; 146:1387–1394.
2. Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: An American academy of sleep medicine clinical practice guideline. J Clin Sleep Med 2017; 13:479–504.
3. Qaseem A, Holty JEC, Owens DK, Dallas P, Starkey M, Shekelle P. Management of obstructive sleep apnea in adults: A clinical practice guideline from the American college of physicians. Ann Intern Med 2013; 159:471–483.
4. Patil SP, Ayappa IA, Caples SM, John Kimoff R, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: An American academy of sleep medicine systematic review, metaanalysis, and GRADE assessment. J Clin Sleep Med 2019; 15:301–334.
5. Kryger MH, Roth T (Tom). Principles and Practice of Sleep Medicine 2016. 1030–1211.
6. American Academy of Sleep Medicine. Evaluation, Management and Long-Term Care of OSA in Adults Clinical Algorithm. Am Acad Sleep Med 2015; 1–6
7. About the ESS – Epworth Sleepiness Scale. https:// epworthsleepinessscale.com/about-the-ess/. Accessed 13 Aug 2020.
8. Littner MR, Kushida C, Wise M, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep 2005; 28:113–121.
9. Kryger M, Roth T, Dement WC (eds). Principles and Practice of Sleep Medicine 2017. https://doi.org/10.1016/c2012-0-03543-0.
10. Jackson ML, McEvoy RD, Banks S, Barnes M. Neurobehavioral impairment and CPAP treatment response in mild-moderate obstructive sleep apnea. J Clin Sleep Med 2018; 14:47–56.
11. Alahmari MD, Alanazi TM, Batawi AA, Al-Osaimi EA, Alrabeeah S, Jebakumar Z, Olaish AH, Almeneessier AS, BaHammam AS. Sleepy driving and risk of obstructive sleep apnea among truck drivers in Saudi Arabia. Traffic Inj Prev 2019; 20:498–503.
12. Sunwoo JS, Shin DS, Hwangbo Y, Kim WJ, Chu MK, Yun CH, Jang T, Yang KI. High risk of obstructive sleep apnea, insomnia, and daytime sleepiness among commercial motor vehicle drivers. Sleep Breath 2019; 23:979–985.
13. Tefft BC. Prevalence of motor vehicle crashes involving drowsy drivers, United States, 1999-2008. Accid Anal Prev 2012; 45:180–186.
14. Driving When You Have Sleep Apnea | FMCSA. https://www.fmcsa.dot.gov/driver-safety/sleep-apnea/driving-when-you-have-sleep-apnea. Accessed 4 Aug 2020.
15. Martinez-Nicolas A, Guaita M, Santamaría J, Montserrat JM, Rol MÁ, Madrid JA (2017) Circadian impairment of distal skin temperature rhythm in patients with sleep-disordered breathing: The effect of CPAP. Sleep. https://doi.org/10.1093/sleep/zsx067.
16. Li Y, Vgontzas A, Kritikou I, Fernandez-Mendoza J, Basta M, Pejovic S, Gaines J, Bixler EO. Psychomotor vigilance test and its association with daytime sleepiness and inflammation in sleep apnea: Clinical implications. J Clin Sleep Med 2017; 13:1049–1056.
17. Tanno S, Tanigawa T, Maruyama K, Eguchi E, Abe T, Saito I. Sleep-related intermittent hypoxia is associated with decreased psychomotor vigilance in Japanese community residents. Sleep Med 2017; 29:7–12.
18. Korkalainen H, Töyräs J, Nikkonen S, Leppänen T (2019) Mortality-risk-based apnea–hypopnea index thresholds for diagnostics of obstructive sleep apnea. J Sleep Res. https://doi.org/10.1111/jsr.12855.
19. Kainulainen S, Duce B, Korkalainen H, Oksenberg A, Leino A, Arnardottir ES, Kulkas A, Myllymaa S, Töyräs J, Leppänen T. Severe desaturations increase psychomotor vigilance task-based median reaction time and number of lapses in obstructive sleep apnoea patients. Eur Respir J 2020. https://doi.org/10.1183/13993003.01849-2019.
20. Pecotic R, Dodig IP, Valic M, Galic T, Kalcina LL, Ivkovic N, Dogas Z. Effects of CPAP therapy on cognitive and psychomotor performances in patients with severe obstructive sleep apnea: a prospective 1-year study. Sleep Breath 2019; 23:41–48.