
 English
English
 French
French
Correlation between serum nitric oxide and severe OSA
Corrélation entre le monoxyde d'azote sérique et l'AOS sévère
K. Dang Thi Mai 1, V. Le Thuong 1, S. Duong Quy 3,4
1: Department of Respiratory Diseases. Cho Ray Hospital. Ho Chi Minh city, Vietnam
2: Lam Dong Medical College. Dalat, Vietnam
3: Penn State Medical College. Hershey Medical Center. PA, USA
Corresponding author
Dr. Sy DUONG-QUY
Lam Dong Medical College - Vietnam. Penn State Medical College - USA
E-mail: sduongquy.jfvp@gmail.com
DOI: 10.12699/jfvpulm.12.37.2021.7
Aims. To evaluate the correlation between serum nitric oxide markers with OSA severity and verify the change after CPAP treatment.
Methods. This was a cross-sectional study and hospital base on population. We investigate 123 OSA patients (40 mild/moderate and 83 severe OSA) in Department of Respiratory Diseases, Cho Ray hospital, Vietnam. Serum nitric oxide and blood test were performed after sleep.
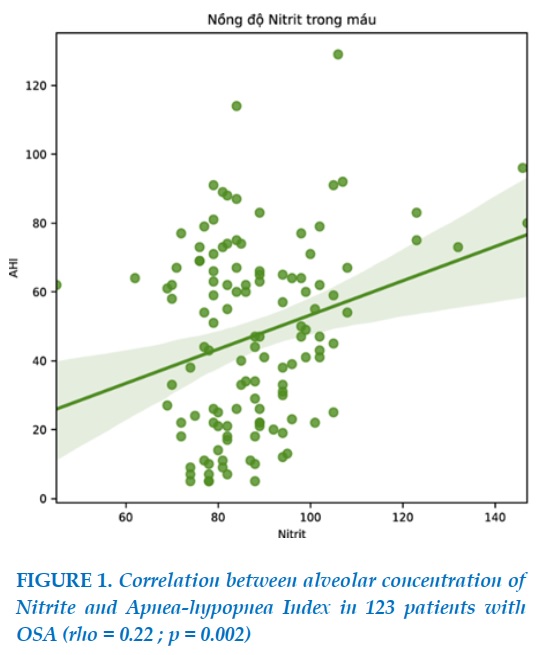
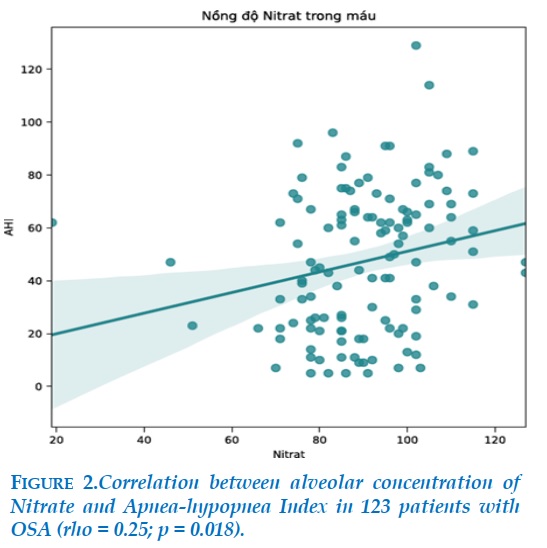
Results. Serum Nitrate were significantly different between mild/moderate, and severe OSA patient (15.5 (9.8-19.7) vs 17.1 (10.9-20.9) respectively, p<0.05). Serum Nitrite were significantly different between mild/moderate, and severe OSA patient (16.1 (13.6-20.4) vs 18.0 (12.9-27.1) respectively, p<0.05). Serum Nitrate and Nitrite (NOx) significantly increased in severe OSA patient (34.0 (27.0-37.8) vs 35.5 (26.3-43.5), p=0.006). The connection could be established between OSA severity and serum nitric oxide markers are through Nitrate, Nitrite (rho = 0.22; p = 0,002 and rho = 0.25 ; p = 0.018). There was no significant correlation between serum nitric oxide and ESS, clinical OSA severity. There were not any correlations between serum nitric oxide and nadir SpO2.
Conclusion. This real-life study showed that serum nitric oxide was associated with OSA severity and relatively higher in the most severe OSA patients. In contrast, serum nitric oxide did not show a clear correlation among clinical OSA severity and neither with nadir SpO2. However, serum nitric oxide changed significantly after CPAP treatment, proposed a simple biomarker to follow up OSA treatment.
KEYWORDS: Obstructive sleep apnea; OSA; Continuous positive airway pressure; CPAP; Nitrate; Nitrite.
Objectifs. Évaluer la corrélation entre les marqueurs sériques d'oxyde nitrique et la sévérité de l'AOS et vérifier le changement après le traitement par PPC.
Méthodes. Il s'agissait d'une étude transversale et d'une base hospitalière sur la population. Nous étudions 123 patients souffrant d'AOS (40 légers/modérés et 83 d'AOS sévères) dans le service des maladies respiratoires de l'hôpital Cho Ray, au Vietnam. L'oxyde nitrique sérique et un test sanguin ont été effectués après le sommeil.
Résultats. Les nitrates sériques étaient significativement différents entre les patients souffrant d'AOS légère/modérée et sévère (15,5 (9,8-19,7) contre 17,1 (10,9-20,9) respectivement, p<0,05). Les nitrites sériques étaient significativement différents entre les patients souffrant d'AOS légère/modérée et sévère (16,1 (13,6-20,4) vs 18,0 (12,9-27,1) respectivement, p<0,05). Les nitrates et nitrites sériques (NOx) ont significativement augmenté chez les patients souffrant d'AOS sévère (34,0 (27,0-37,8) contre 35,5 (26,3-43,5), p = 0,006). Le lien a pu être établi entre la sévérité de l'AOS et les marqueurs sériques d'oxyde nitrique se font par le biais du nitrate, du nitrite (rho = 0,22 ; p = 0,002 et rho = 0,25 ; p = 0,018). Il n'y avait pas de corrélation significative entre l'oxyde nitrique sérique et l'ESS, la sévérité clinique de l'AOS. Il n’y avait pas de corrélation entre l'oxyde nitrique sérique et le nadir SpO2.
Conclusion. Cette étude en vie réelle a montré que l'oxyde nitrique sérique était associé à la sévérité de l'AOS et relativement plus élevé chez les patients atteints d'AOS les plus sévères. En revanche, l'oxyde nitrique sérique n'a pas montré de corrélation claire entre la sévérité clinique de l'AOS et ni avec le nadir SpO2. Cependant, l'oxyde nitrique sérique a changé de manière significative après le traitement PPC, a proposé un biomarqueur simple pour suivre le traitement de l'AOS.
MOTS CLÉS: Apnée obstructif du sommeil; AOS; Pression positive continue; PPC; Nitrate; Nitrite.
INTRODUCTION
OSA is characteristic by repeated many episodes of short apnea and hypopnea during sleep time. The prevalence of OSA is about 13% in male and 6% in female worldwide compare with 8,5% in Vietnam and it nowadays is increasing with the developing of obesity. Its consequence well-known is arousals and desaturations. In fact, OSA is known as an independent risk factor of cardio-vascular diseases such as: hypertension, arrythmia or stroke. OSA treated was improved blood pressure significant in some researches. Intermittent hypoxia would be a mechanism of oxidative stress, inflammation, and metabolic dysfunctions in OSA patient. Following some previous study, its cardiovascular morbidities usually developed with OSA severity. Thus, evaluation pulmonary inflammation may be useful to screen severe OSA so that conduct to evaluation by polysomnography or respiratory polygraphy and treat it then.
Nitric oxide (NO) plays an important role both as a physiological modulator of vascular tone and as a pathological pro-inflammatory biomarker implicated in many lung disorders. NO is the main vasodilating substance released from the endothelium. Endothelium dependent vascular relaxation was impaired independently of hypertension.
Direct measurements of NO or its derivatives have, however, not yet been performed in patients with OSA. However, serum NO is a gas with very short half-life, so it is difficult to measure it directly. More feasible is the measurement of the more stable derivatives of NO nitrate and nitrite in biological fluids. Nitrite and nitrate levels have been suggested as the most appropriate measure of overall NO production.
So that, we conduct this study to evaluate the relation between each serum nitric oxide and OSA severity and its response to treatment.
METHODS
Subjects
Consecutive patients meeting the inclusion criteria were recruited for this prospective cross-sectional study. All had been referred to our sleep-disordered breathing clinic because of clinical symptoms suggestive of OSA. The patients underwent polygraphy with 4 channels at Cho Ray hospital then all patients had OSA diagnosis were concluded in this study. We excluded patients with a history of cognitive disorders, symptoms of respiratory tract infection in the 6 weeks prior to referral, NYHA III-IV heart failure, chronic respiratory failure, pregnant women. Patients were also excluded if they had received treatment with inhaled or oral corticosteroids in the last 10 days.
The study was approved by the ethics committee of our hospital, and all gave their signed, informed consent.
Study design: Individual characteristics were recorded, and a clinical questionnaire was used to collect information on smoking, medication, cardiovascular disease (hypertension, ischemic heart disease, and stroke), diabetes mellitus and dyslipidemia. Excessive daytime sleepiness was assessed using the Epworth Sleepiness Scale. All individuals were studied by overnight respiratory polygraphy in hospital. Trained staff assigned to our lung function laboratory and sleep-disordered breathing unit carried out the tests.
Patients were included in the severe OSA group consecutively if the results of the sleep study indicated they had an apnea-hypopnea index (AHI) ≥ 30. Mild-moderate OSA group individuals were found to have an AHI<30. Then next morning, each subject had a blood test for serum nitric oxide, all of which were carried out at the same hour of the day (06:00 to 7:00 a.m.).
Severe OSAS agreed to CPAP treatment then underwent a titration night study by attended polygraphy with a simplified automatic CPAP device (Phillip®, USA). After 3 months of CPAP treatment the patient came to a follow-up visit that included an interview and collection of anthropometric data as well as the blood test needed for determining serum nitric oxide. CPAP treatment adherence was assessed objectively by reading the counter that showed the operating hours since treatment was started.
Respiratory polygraphy: patients underwent respiratory polygraphy (CIDELEC, France). SpO2 was assessed by pulse oximetry and airflow by nasal flow pressure sensor. Thoracic and abdominal excursion bands and sus-sternal captor for snoring and respiratory sound and body position sensors were also in position. The same AHI criteria used in polysomnography were also used in polygraphy, with the exception that arousals were not detected by the polygraphy device.
Nitric oxide measurement: Arrowstraight ™ Nitric Oxide measurement system of Lazar Research laboratories, Inc, USA. At 06:00 to 7: 00 AM, after undergoing polygraphy, a peripheral venous blood sample was withdrawn into a tube prepared with EDTA and centrifuged at 2000 rpm for 10 minutes. The supernatant plasma was stored in a refrigerator at –20°C. The blood test for serum NO also repeated after CPAP treatment 3 months.
Statistical analysis: Data were analyzed using SPSS
20.0 (Chicago, IL, USA). Values were expressed as mean ± standard derivation (SD) for continuous parameters, number, and percentage for categorical variables. Normal distribution was determined using Kolmogorov–Smirnov test. Comparisons were made by Student’s t-test or Mann–Whitney test for quantitative variables and Chi-square test or Fisher’s exact test for qualitative variables, as appropriate. Exhaled NO levels before and after CPAP treatment were compared using Wilcoxon matched-pairs rank test. Linear correlations between exhaled NO with AHI and ST-90% were done using Spearman’s method. A multivariate linear regression was used to examine the association of AHI with exhaled NO and BMI. Statistical significance was two-sided at p<0.05.
RESULTS
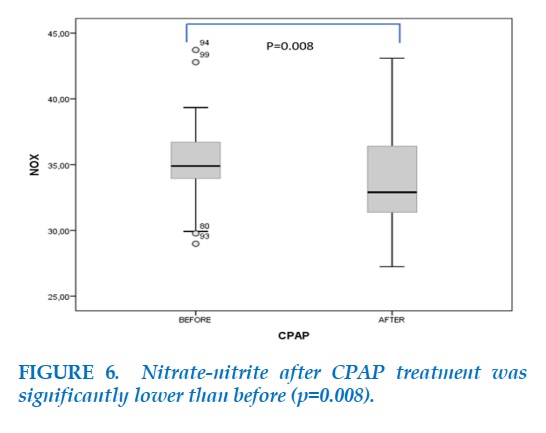
We prospectively included 123 OSA subjects (105 men) with mean age (53.6 ± 14.9 years) from January 2017 to December 2019. Characteristics of patients were presented in Table 1.
There was no significant difference in term of age, current-smoking and alcohol status, blood pressure and daytime sleepiness between the two groups. There was a significant difference of BMI, neck, and waist circumference between two group. AHI was higher and saturation was lower in severe OSA. Diabetes type 2 and heart coronary disease: hypertension, ischemic heart disease and lipid dysfunction were not significant difference between severity OSA group.
Regarding respiratory parameters, severe OSA patients had significantly higher AHI (62.2 ± 19.1 events/hour versus 16.6 ± 7.4 events/ hour, p<0.001), lower nadir nocturnal SpO2 (63.8 ± 11.8% versus 75.3 ± 10.8%, p<0.001 as compared with mild-moderate OSA subjects. Comparing anthropometric parameters, severe OSA patients had higher BMI (29.7 ± 5.0 versus 26.1 ± 4.7 kg/m2), higher neck and waist circumference (41.5 ± 3.7 and 105.1 ± 10.8 versus 38.6 ± 2.9 and 96.8 ± 13.0) than mild-moderate OSA patients.
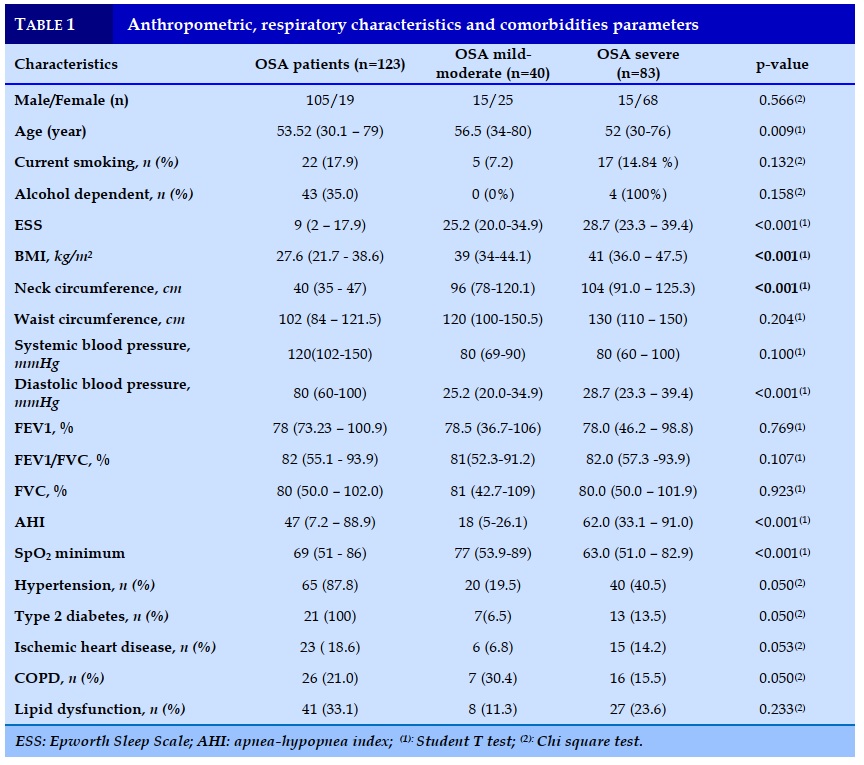
Serum nitric oxide characteristic
We evaluated the changes in serum nitric oxide markers among 2 OSA severity subgroups using a non-parametric analysis of variance. The result was presented in Table 2.
Nitrite and nitrate were significantly different between 2 OSA severity subgroups. Nitrite and Nitrate of severe OSA group were increased more than the one of mild/moderate OSA group (18 vs 16.1 and p= 0.037; 17.1 vs 15.5 and p=0.028). So, the sum of 2 substances (NOx) were also increased significantly in severe OSA group (35.5 vs 34 and p= 0.006).
Then the correlation between exhaled NO was described by scatter-dot plot graph in Figure 1 and 2.
Correlation between serum nitric oxide and AHI
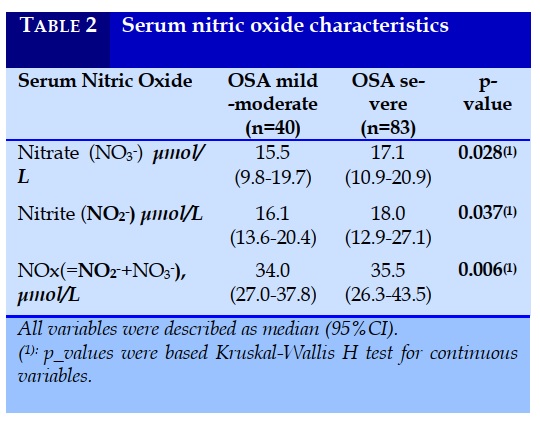
However, there was no correlation between serum NO and nadir SpO2 or ESS in this study.
Spearman’s correlation and 95%CI with bootstrap
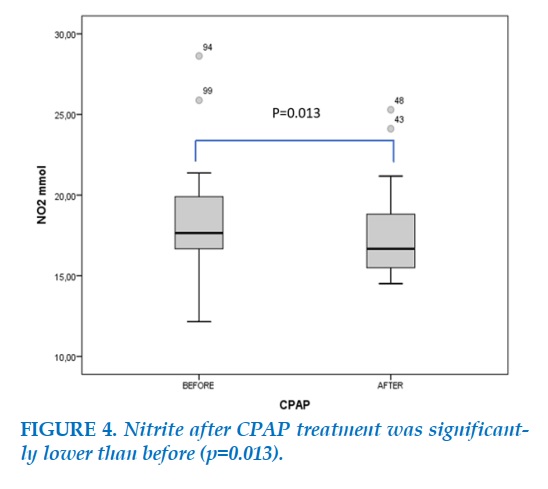
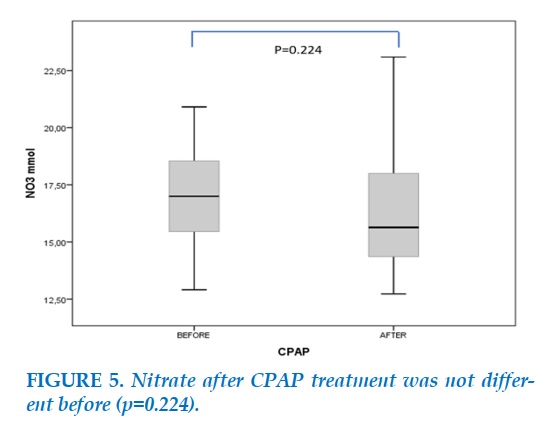
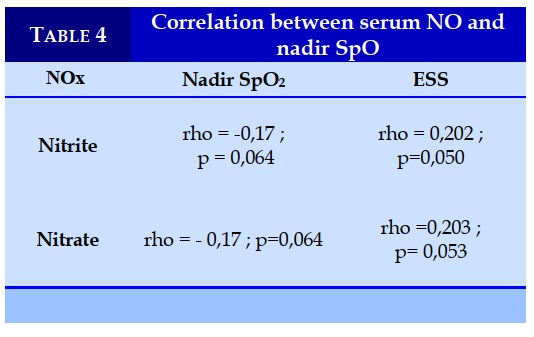
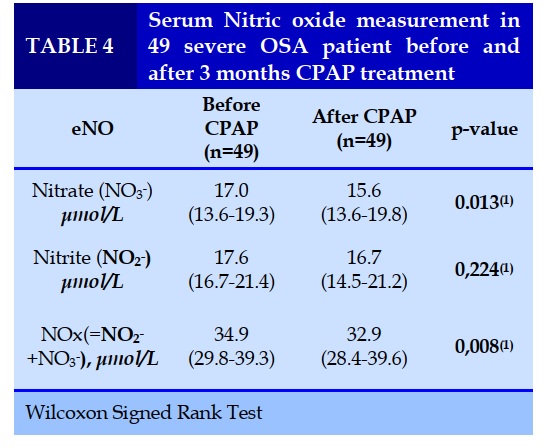
CPAP treatment was initiated in 49 of the 83 OSAS patients. At the 3-month follow-up visit, CPAP was being used for a mean of 6±1 h per night. At which time Nitrate and Nitrite levels had decreased significantly.
DISCUSSION
In our study, the main result is nitrate-nitrite level was significantly different among 2 OSA severity group and asocicated with AHI, second result is nitrite level and decreased after CPAP treatment. Nevertheless, serum NO concentration depends not only on endogenous NO produce but also on other aspects of NO metabolism such as NO uptake or kidney metabolism. Then, it is difficult to evaluate this association. In our study, we didn’t eliminate cardiovascular disease comorbidities that could influence to this result. Research of Ip (2000) with 70 OSA subjects found a negative correlation among nitrate-nitrite with AHI (r=-0.389, p=0.001) [3]. Ozkan (2007) did a research with 34 OSA subjects which found only a negative correlation between nitrate-nitrite with severe OSA (r=-0,641, p=0,007) [5]. Yuksel (2013) with 51 OSA subjects which didn’t find any correlation between nitrate-nitrite and AHI (p=0,9854) [7]. In Weiss (2012) article with 38 OSA subjects, they confirmed a negative correlation among nitrate-nitrite and AHI (r=-0,42, p<0,05) [6]. Article of Canino (2015) had a similar result with correlation between AHI and nitrate-nitrite (r=-0,61, p<0,001) [1]. So, summary all subjects were pure cardiovascular diseases and negative correlation between AHI with nitrate-nitrite. Finally, endogenous NO had an association with OSA severity in our study and some previous studies.
The association between serum NO and nadir oxygen saturation did not establish in our study. Ortac and al found a negative correlation among serum NO and oxygen desaturation time (r= -0.45 and p< 0.05) [4]. IP and al confirmed the correlation between desaturation time and serum NO with r=-0.346 and p=0.004 [3]. However, Noda and al in a research did not found any correlation among nadir saturation and saturation time. Ozkan and al found only negative correlation among serum NO and nadir saturation in severe OSA (r=−0.641 và p=0.007) [5]. For summary, serum NO was not corelated with nadir oxygen similar with previous studies unfortunately, we did not found correlation with desaturstion time. The correlation between serum NO and nighttime saturation in OSA patients was not the same in previous studies. Perhaps the studied sample sizes were small or intermittent hypoxia do not correlate with nadir oxygen. Therefore, the influence of drugs on NOx levels must be considered [8-11].
Severe excessive daytime sleepiness is one of important symptom for evaluation OSA severity. However, this procedure is almost subjective. Other objective methods for this procedure are still not available in Vietnam so that serum NO is a potential biomarker. Unfortunately, we did not find any correlation between serum NO and Epworth sleepiness scale. Franco and al (2004) had the similar result with us, that they did not find any association among serum NO and Epworth sleepiness scale [2].
Physiologic serum NO levels were restored after 3 months of CPAP treatment. Classically, we used CPAP counter to evaluate treatment effect but it’s not enough. Some study demonstrated that, cardiovascular event could also affect to OSA with CPAP treatment. So in this case, serum NO: Nitrite and nitrate could be a biomarkers noninvasive measurements could eventually to provide valuable molecular signatures in severe OSA treatment for long term [12-16].
CONCLUSION
Severe OSAS patients have higher serum NO levels compared to mild-moderate, and physiologic levels are restored after 3 months of CPAP treatment.
Blood test to measure serum NO provide an easy to detect or monitor endothelial inflammation in severe OSAS patients. Use of these measures would contribute to, aiding more accurate prediction of response to treatment.
CONFLICT OF INTERESTS
Non.
REFERENCES
1. Canino Baldassare, Hopps Eugenia, Calandrino Vincenzo, et al. Nitric oxide metabolites and erythrocyte deformability in a group of subjects with obstructive sleep apnea syndrome. Clinical Hemorheology and Microcirculation2015; 59, pp. 45-52.
2. Franco C. M., Lima A. M., Ataíde L., Jr., et al. Obstructive sleep apnea severity correlates with cellular and plasma oxidative stress parameters and affective symptoms. J Mol Neurosci 2012; 47(2), pp. 300-10.
3. Ip M. S., Lam B., Chan L. Y., et al. Circulating nitric oxide is suppressed in obstructive sleep apnea and is reversed by nasal continuous positive airway pressure", Am J Respir Crit Care Med 2020; 162(6), pp. 2166-71.
4. Ortaç Ersoy E., Fırat H., Akaydın S., et al. Association of obstructive sleep apnea with homocystein, nitric oxide and total antioxidant capacity levels in patients with or without coronary artery disease. Tuberk Toraks,2014; 62(3), pp. 207-14.
5. Ozkan Yeşim, Firat Hikmet, Simşek Bolkan, et al. Circulating nitric oxide (NO), asymmetric dimethylarginine (ADMA), homocysteine, and oxidative status in obstructive sleep apnea-hypopnea syndrome (OSAHS). Sleep & breathing 2008; 12(2), pp. 149-54.
6. Weiss J. W., Liu Y., Li X., et al. Nitric oxide and obstructive sleep apnea. Respir Physiol Neurobiol, 2012; 184(2), pp. 192-6.
7. Yüksel Meral, Okur Hacer Kuzu, Pelin Zerrin, et al. Arginase activity and nitric oxide levels in patients with obstructive sleep apnea syndrome. Clinics,2014; 69, pp. 247-52.
8. Tran-Van H, Vo-Thi-Kim A, Duong-Quy S. The Study of Correlation between Diurnal Blood Pressure with Nocturnal Oxygen Desaturation and Nitrite Production in Subjects with Obstructive Sleep Apnea (OSA). Journal of Vascular Medicine & Surgery 2017; 5 (3), 317.
9. Vo-Thi-Kim A, B Nguyen-Xuan, D Dao-Van, Duong-Quy S. The Effect of Continuous Positive Airway Pressure (CPAP) in Treatment of Patients with Refractory High Blood Pressure Associated with Severe Obstructive Sleep Apnea (OSA).J Vasc Med Surg2017;5(327), 2.
10. S Duong-Quy, P Dao, T Hua-Huy, NN Le-Dong, AT Dinh-Xuan. Impairment of Pulmonary Vasoreactivity in Response to Endothelin-1 In Patients With Chronic Obstructive Pulmonary Disease (COPD). J Vasc Med Surg 2015;3 (213), 2.
11. Duong-Quy S. Endothelial Dysfunction in Patients with Obstructive Sleep Apnea (OSA). Journal of Vascular Medicine & Surgery 2015;3 (1), 1-2.
12. Dang Thi Mai K, Y Nguyen Hoang, et al. Study of exhaled NO in subjects without apneas during sleep. J Func Vent Pulm 2015; 6 (17), 36-42.
13. Hua-Huy T, NN Le-Dong, S Duong-Quy, L Luchon, S Rouhani, et al. Increased alveolar nitric oxide concentration is related to nocturnal oxygen desaturation in obstructive sleep apnoea. Nitric Oxide 2015; 45, 27-34.
14. Dang Thi Mai K, Dang Vu T, Tran Van N, Nguyen Thi Hong A, Duong–Quy S. Obstructive Sleep Apnea (OSA) and Metabolic Syndrome (MetS). J Func Vent Pulm 2020; 11 (33), 36-41.
15. Duong-Quy S, Thong Hua-Huy, Huyen-Tran Tran-Mai-Thi, Nhat-Nam Le-Dong, Timothy J. Craig, Anh-Tuan Dinh-Xuan, (2016) "Study of Exhaled Nitric Oxide in Subjects with Suspected Obstructive Sleep Apnea: A Pilot Study in Vietnam", Pulmonary Medicine, vol. 2016, Article ID 3050918, 7 pages.
16. Dang-Thi-Mai K, Le-Dong NN, Le-Thuong V, Tran-Van N, Duong-Quy S. Exhaled Nitric Oxide as a Surrogate Marker for Obstructive Sleep Apnea Severity Grading: An In-Hospital Population Study. Nature and Science of Sleep 2021:13 763–773.
FIGURES - TABLES
REFERENCES
1. Canino Baldassare, Hopps Eugenia, Calandrino Vincenzo, et al. Nitric oxide metabolites and erythrocyte deformability in a group of subjects with obstructive sleep apnea syndrome. Clinical Hemorheology and Microcirculation2015; 59, pp. 45-52.
2. Franco C. M., Lima A. M., Ataíde L., Jr., et al. Obstructive sleep apnea severity correlates with cellular and plasma oxidative stress parameters and affective symptoms. J Mol Neurosci 2012; 47(2), pp. 300-10.
3. Ip M. S., Lam B., Chan L. Y., et al. Circulating nitric oxide is suppressed in obstructive sleep apnea and is reversed by nasal continuous positive airway pressure", Am J Respir Crit Care Med 2020; 162(6), pp. 2166-71.
4. Ortaç Ersoy E., Fırat H., Akaydın S., et al. Association of obstructive sleep apnea with homocystein, nitric oxide and total antioxidant capacity levels in patients with or without coronary artery disease. Tuberk Toraks,2014; 62(3), pp. 207-14.
5. Ozkan Yeşim, Firat Hikmet, Simşek Bolkan, et al. Circulating nitric oxide (NO), asymmetric dimethylarginine (ADMA), homocysteine, and oxidative status in obstructive sleep apnea-hypopnea syndrome (OSAHS). Sleep & breathing 2008; 12(2), pp. 149-54.
6. Weiss J. W., Liu Y., Li X., et al. Nitric oxide and obstructive sleep apnea. Respir Physiol Neurobiol, 2012; 184(2), pp. 192-6.
7. Yüksel Meral, Okur Hacer Kuzu, Pelin Zerrin, et al. Arginase activity and nitric oxide levels in patients with obstructive sleep apnea syndrome. Clinics,2014; 69, pp. 247-52.
8. Tran-Van H, Vo-Thi-Kim A, Duong-Quy S. The Study of Correlation between Diurnal Blood Pressure with Nocturnal Oxygen Desaturation and Nitrite Production in Subjects with Obstructive Sleep Apnea (OSA). Journal of Vascular Medicine & Surgery 2017; 5 (3), 317.
9. Vo-Thi-Kim A, B Nguyen-Xuan, D Dao-Van, Duong-Quy S. The Effect of Continuous Positive Airway Pressure (CPAP) in Treatment of Patients with Refractory High Blood Pressure Associated with Severe Obstructive Sleep Apnea (OSA).J Vasc Med Surg2017;5(327), 2.
10. S Duong-Quy, P Dao, T Hua-Huy, NN Le-Dong, AT Dinh-Xuan. Impairment of Pulmonary Vasoreactivity in Response to Endothelin-1 In Patients With Chronic Obstructive Pulmonary Disease (COPD). J Vasc Med Surg 2015;3 (213), 2.
11. Duong-Quy S. Endothelial Dysfunction in Patients with Obstructive Sleep Apnea (OSA). Journal of Vascular Medicine & Surgery 2015;3 (1), 1-2.
12. Dang Thi Mai K, Y Nguyen Hoang, et al. Study of exhaled NO in subjects without apneas during sleep. J Func Vent Pulm 2015; 6 (17), 36-42.
13. Hua-Huy T, NN Le-Dong, S Duong-Quy, L Luchon, S Rouhani, et al. Increased alveolar nitric oxide concentration is related to nocturnal oxygen desaturation in obstructive sleep apnoea. Nitric Oxide 2015; 45, 27-34.
14. Dang Thi Mai K, Dang Vu T, Tran Van N, Nguyen Thi Hong A, Duong–Quy S. Obstructive Sleep Apnea (OSA) and Metabolic Syndrome (MetS). J Func Vent Pulm 2020; 11 (33), 36-41.
15. Duong-Quy S, Thong Hua-Huy, Huyen-Tran Tran-Mai-Thi, Nhat-Nam Le-Dong, Timothy J. Craig, Anh-Tuan Dinh-Xuan, (2016) "Study of Exhaled Nitric Oxide in Subjects with Suspected Obstructive Sleep Apnea: A Pilot Study in Vietnam", Pulmonary Medicine, vol. 2016, Article ID 3050918, 7 pages.
16. Dang-Thi-Mai K, Le-Dong NN, Le-Thuong V, Tran-Van N, Duong-Quy S. Exhaled Nitric Oxide as a Surrogate Marker for Obstructive Sleep Apnea Severity Grading: An In-Hospital Population Study. Nature and Science of Sleep 2021:13 763–773.
ARTICLE INFO
DOI: 10.12699/jfvpulm.12.37.2021.7
Conflict of Interest
Non
Date of manuscript receiving
15/6/2020
Date of publication after correction
15/7/2021
Article citation
Dang Thi Mai K., Le Thuong V., Duong Quy S. Correlation between serum nitric oxide and severe OSA. J Func Vent Pulm 2021;37(12):7-12