
 English
English
 French
French
The change of ventilatory function in patients with CO2 inflating in peritoneal cavity for abdominal endoscopic anesthesia surgery
Le changement de la fonction ventilatoire chez les patients ayant le soufflement de CO2 dans la cavité péritonéale pour la chirurgie abdominale endoscopique sous l’anesthésie
T. Le Van, H. Ta Thanh
Hai Duong Medical Technical University. Hai Duong, Viet Nam
Corresponding author
Docteur LE VAN Them
Hai Duong Medical Technical University. Hai Duong. Viet Nam
Email : themlv2003@gmail.com
ABSTRACT
Objective. This study aimed to describe the change of PetC02, peak and Vt in patients with abdominal endoscopic anesthesia surgery when CO2 inflating into peritoneal cavity at Military Central Hospital.
Methods. It was a perspective and descriptive study.
Results. PetCO2 increased immediately at the time of CO2 inflating, highly increased in the first 25 minutes after CO2 inflating. Average PetCO2 maximum was increased from 31.06±2.517 to 38.92±2.114 mmHg at T5 by 25.31%. Between 30 minutes after pumping and T120, PetCO2 was slightly increased and more stable; PetCO2 slightly was decreased after 5 minutes of CO2 deflating and come to nearly normal at completed surgery. At the time of totally completed surgery, PetCO2 was persistent higher than that at the begin; the peak was highly increased at the beginning of CO2 inflating and reached the highest value during period from T10 to T25. Average peak was maximally increased from 17.24±1.762 to 25.64±3.256 cmH2O at T20 or by 48.72%. The peak was persisted highly at T120 and gradually decreased after CO2 deflating and toward to the peak value before CO2 inflating. Vt was slightly decreased from the beginning of CO2 inflating; average Vt was minimally decreased at T30 from 466.21±54.537 to 445.67±51.621 mL or 4.41%; Vt was increased immediately after CO2 deflating and gradually come to Vt value when the surgery was just completed.
KEYWORDS: PetCO2, respiratory system, anesthesia, tidal volume.
RÉSUMÉ
Introduction. Cette étude avait pour but de décrire le changement de la PetCO2, du pic et de Vt chez les patients avec une anesthésie endoscopique abdominale lorsque le CO2 est soufflé dans la cavité péritonéale à l'Hôpital Militaire Central 108.
Méthodes. Il s’agit d’une étude descriptive et perspective.
Résultats. La PetCO2 a augmenté immédiatement au moment de soufflement à CO2, fortement augmenté dans les 25 premières minutes après le soufflement de CO2. Le maximum de moyen de PetCO2 était passé de 31,06 ± 2,517 à 38,92 ± 2,114 mmHg à T5 de 25,31%. Entre 30 minutes après le soufflement et T120, PetCO2 était légèrement augmenté et plus stable; PetCO2 a été légèrement diminué après l’échappement du CO2 à 5 minutes après l’intervention chirurgicale. Au moment de la chirurgie totalement terminée, la PetCO2 était persistant plus haut que celui du début; le pic a été fortement augmenté au début de soufflement de CO2 et au plus haut niveau pendant la période allant de T10 à T25. Le pic maximal de moyen a été est passé de 17,24±1,762 à 25,64±3,256 cmH2O à T20 et de 48,72%. Le pic a été persisté fortement à T120 et a été diminué progressivement après l’échappement de CO2 et atteignait de la valeur maximale avant le soufflement de CO2. Vt a été légèrement diminué depuis le début des soufflements de CO2; Vt minimum de la valeur moyenne a été diminué à T30 de 466,21±54,537 à 445,67±51,621 mL ou à 4,41%; Vt a été augmenté immédiatement après l’échappement de CO2 et a été progressivement atteignant de la valeur Vt lorsque la chirurgie vient de s’achever.
MOTS CLÉS: PetCO2, système respiratoire, anesthésie, volume courant.
INTRODUCTION
Laparoscopic surgery is considered to be a surgical revolution that has been used in diagnostics and treatment since the late 1980's and has been widely used in a variety of ways. In the field of obstetrics, gastrointestinal diseases, urology, or thoracic problems, etc.
Laparoscopic surgery has advantages over open surgery: less traumatic surgery, short hospital stay, minimally invasive surgery, less postoperative pain, significantly reduced complications of bacterial infection and adhesion after surgery, ensure aesthetics, and recovery time after surgery fastly [1].
Along with the advancement of laparoscopic surgery, anesthesia has many experimental and clinical studies related to laparoscopic surgery that have been conducted to address this issue. The use of CO2 pumps into the peritoneal cavity and extra-peritoneal cavity to expand the surgical site to make the anesthetists facing to the changes in circulation and respiration due to the pumping effect. The understanding of these mechanisms is essential for application in the selection of the best anesthesia, monitoring, attitudes, and care for patients with endoscopic surgery. The circulatory, respiratory and body temperature disorders are highly dependent on inflatable pressure, inflatable area (intraperitoneal or extraperitoneal) and pumping time [2].
For respiratory system, inflating the air into the peritoneal cavity or out of the peritoneal cavity can lead to hypercapnia, 30% reduction of lung compliance, increased airway pressure, decreased diaphragm movement, increase of respiratory work-load due to increase of intra-abdominal pressure [2]. In addition, CO2 that is a cold gas when injected into the body over a long period of time can lead to hypothermia. The method of laparoscopic surgery has many advantages, but it causes many disorders for patients so the anesthesia workers must always focus on monitoring, patient care, and coordination in time to ensure the safety for patients [2].
There are some studies on respiratory effects in patients with endoscopic cholecystectomy or ovarian cystoscopy. However, for other endoscopic surgeries, the level of respiratory effects is also great.
From the above situation, we conducted the study on this topic with the aim were to describe the change of PetCO2 in anesthesia patients with CO2 inflating into the peritoneal cavity and to describe the peak and Vt changes in laparotomies with CO2 inflating into the peritoneal cavity in Military Central Hospital 108.
METHODS
Study subjects
Patients undergoing laparoscopic surgery with CO2 inflating into the peritoneal cavity with general anesthetic methods by endotracheal anesthesia such as for endoscopic cholecystectomy, endoscopic appendectomy, endoscopic surgery colonoscopy, endoscopic surgery, cystic ovaries at the Surgery and Anesthesia Department of the Military Central Hospital 108 from April to June 2018.
Inclusion criteria
Age ≥ 18 years.
Patients do not have some diseases such as heart failure, coronary disease, chronic heart valvular disease, chronic lung disease, emphysema, lung bulla, increased intracranial pressure, glaucoma.
ASA: I or II according to the classification of the American Anesthesia Association.
Inflated time ≤2h.
Patients agree to participate in the study.
Exclusion criteria
Patients did not agree to participate in the study.
Patients do not have sufficient awareness to answer the survey such as: syncope, mental disease, deaf.
Methods
Study design
It was a propective and descriptive study.
Sample size and sampling methods
All included patients underwent peritoneal laparoscopic surgery with general anesthesia with endotracheal anesthesia method at the Surgery and Anesthesia Department of Military Central Hospital 108.
Time and place of study
Location: Department of Surgery and Anesthesia of Military Central Hospital 108.
Time: from April to June 2018.
Information gathering techniques
Sources of information: Medical records collected information on name, age, sex, diagnosis, indications of surgery, surgeon, surgery day, anesthesia method, anesthesiologist.
Observe, asking, examining the patient, and medical history, height, weight, …were made.
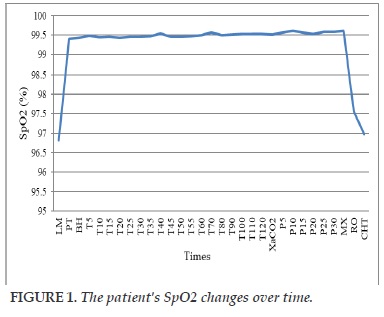
Assessment of respiratory changes (PetCO2, peak, Vt, SpO2) was based on the monitoring of the indicators on the monitoring machine, the anesthesia machine at the time of the study and recorded on the data collection form.
Data processing and analysis
The results of present study were processed according to SPSS software 20.0 (Chicago; USA). Data are expressed as mean± SD, percentage (%).
RESEARCH RESULTS
General characteristics of patients and surgery
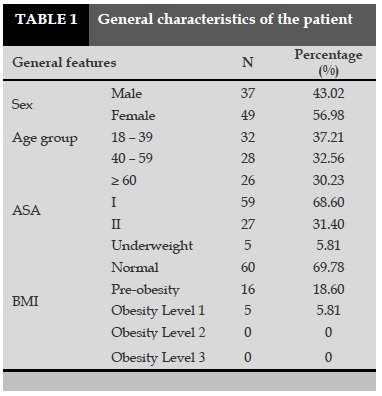
Of the 86 patients studied there were 37 patients were male accounting for 43.02%; 49 patients were female, accounting for 56.98%.
Age group: from 18 to 39 years old, there was 32 patients accounted for 37.21%; from 40 to 59 years old, there was 28 patients accounted for 32.56%; for ≥60 years old with 26 patients accounting for 30.23%.
ASA: there were 59 patients in ASA I accounting for 68.60%, 27 patients in ASA II accounted for 3.40% (Table 1).
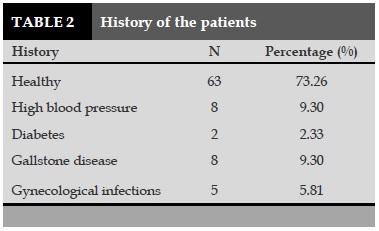
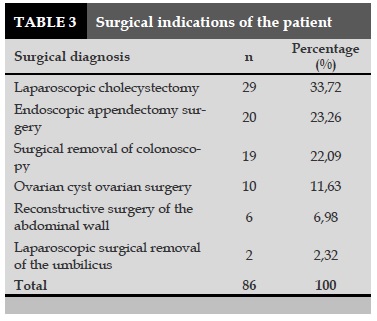
BMI: 5 patients with low weight, 5 patients with obesity level 1 accounted for 5.81%; 16 pre-obesity patients accounted for 18.60%; 60 patients in the normal state accounted for 69.78%. Of the 86 patients studied the majority of patients with a healthy history (73.26%), hypertension accounted for 9.30%, gallstones accounted for 9.30% (Table 2). 29 cases of laparoscopic surgical excision of gallbladder accounted for 33.72%, 2 patients of umbilical cord cystoscopy surgery, accounting for 2.32% (Table 3).
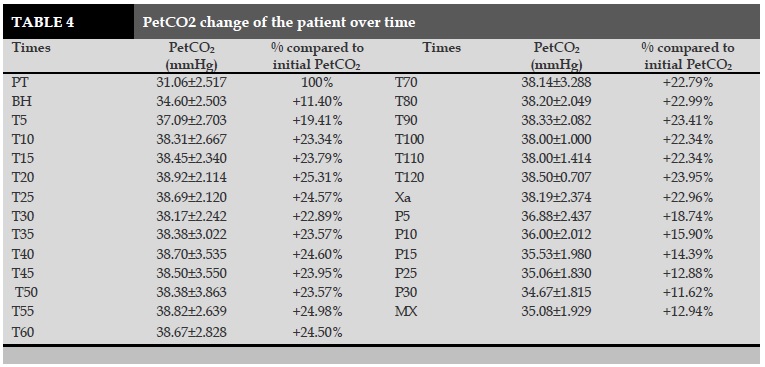
PetCO2 fluctuations of patients over time (Table 4)
PetCO2 was highest at T20; increased 25.31% in compared to PetCO2 at operation time.PetCO2 increase from the time of inflating until T120, after the deflating, PetCO2 gradually reduced.PetCO2 remained high after the end of surgery, higher than the operation time at 12.94%.
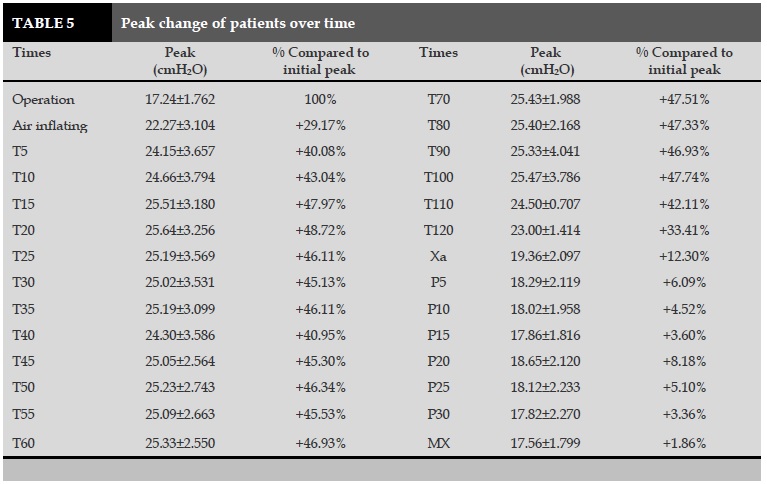
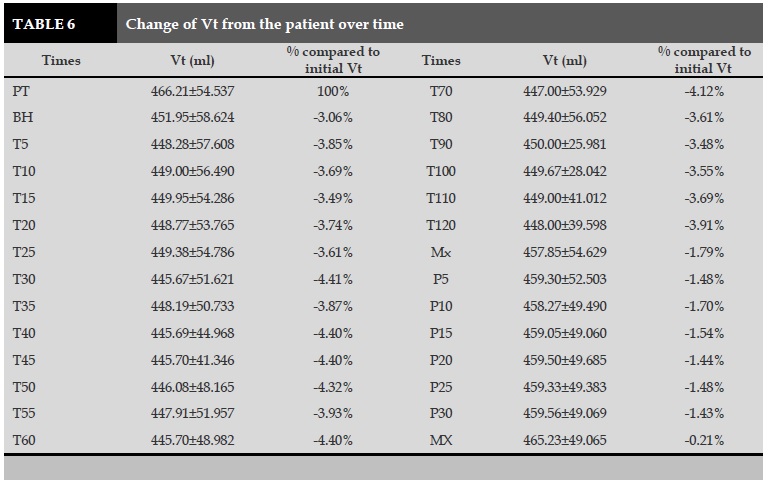
Peak and Vt change of patients over time
Peak at peak T20; increased than Peak at the time of operation was 48.72%.
Vt at the time of T30 was lowest decrease, down to 4.41% compared to at the operation time.
DISCUSSION
General characteristics of the patients
Age, gender of patients
Of the 86 patients studied, the youngest and the oldest were 22 and 73 years, divided into three age groups: 18 to 39 years old (37.21%); 40-59 years old (32.56%); ≥60 years old (30.23%). Three age groups were fairly uniform rates. Current laparoscopic surgery is performed on many different ages from young to old person. For gender: male was 37/86 patients, accounting for 43.02%; women was 49/86 patients, accounting for 56.98%. The difference in male-female ratio was due to the fact that 10 patients with ovarian cysts were selected for the study.
Health status, condition and history of patients before surgery
The patients had study criteria for this study included patients without severe respiratory and cardiovascular diseases. The results obtained with the preoperative status of the patient were as follows: 68.60% of patients with ASA I (59 patients); 31.40% patients with ASA II (27 patients).
The condition of the patients was the normal general condition was 69.78% (60 patients); 5.81% (5 patients) underweight; 18.60% (16 patients) obese; 5.81% (5 patients) was obese with grade 1 and no one with obese of grade 2, 3.
Patient's history of surgery: the majority of patients underwent surgery had the healthy history of 63 patients (73.26%), 8 patients had hypertension (9.30%), 8 patients with gallstones (9.30%), 5 patients with gonorrhea (5.81%), 2 diabetic patients (2.33%). These conditions were mild, stable under treatment and could not affect the results of the present study [4-7].
Fluctuation of PetCO2 in anesthesia patients undergoing laparoscopic surgery has CO2 inflating into the peritoneal cavity
PetCO2 is the final concentration of exhaled CO2 that is monitored through the respiratory gas analyzer.
PetCO2 monitoring is considered to indirectly measure PaCO2 in arterial blood. Numerous studies showed that the difference between PaCO2 and PetCO2 was 2.4±1.5 mmHg and there was no different between before, during and after air inflating. However, the variability of this change is greater when patients with impaired respiratory function or cardiopulmonary diseases. In this study, we performed the PetCO2 indicator and patients in the ASA I, ASA II class did not have any cardiopulmonary disease.
PetCO2 increased rapidly after inflating, increasing rapidly from 5 minutes after inflation to 25 minutes after that. The average PetCO2 in the study was at the highest level at T5: PetCO2 increased from 31.06 ±2.517 to 38.92±2.114 mmHg, increased by 25.31%. The period from 30 minutes after inflating to T120 PetCO2 increased less and more stable. This finding is consistent with that of Ton et al. [3]: PetCO2 increased rapidly in the first 10 minutes after inflating from 28.46±2.88 mmHg to 36.13±3.1 mmHg, low and stable after 30 minutes of surgery and adjusting the increase of CO2 by increasing the volume of gas flow or respiratory rate. The absorption of CO2 causes PetCO2 to rapidly increase in the first stage of the absorption by the body in a passive diffusion mechanism, from high pressure to low pressure; The second stage slows down due to increased abdominal pressure, pressure on the blood vessels, and increased blood vessel resistance.
After surgery, PetCO2 remained at a higher level than in PetCO2 at the time before operation. Therefore, monitoring patients in the recovery room is very important to avoid the risk of respiratory failure in patients after surgery in general and patients after surgery in laparoscopic surgery in particular [8-10].
In the present study, the tidal volume (circulating volume: Vt) decreased slightly from the moment after inflating, Mean Vt was decreased lowest at time T30; Vt was decreased from 466.21±54,537 to 445.67± 51,621 mL, reduction of 4.41%. After 30 minutes of air inflating, Vt was still lower than the initial Vt and more stable. Immediately after discharge of CO2 inflating, Vt gradually was increased, stabilized and approached to the value of Vt at the time of surgery.
CONCLUSION
The results of our study showed that, PetCO2 was increased from the time of CO2 inflating, increased sharply in the first 25 minutes after CO2 injection. The highest average mean PetCO2 was increased in T5. From 30 minutes after pumping to T120, PetCO2 was increased less and more stable.
In addition, PetCO2 was gradually decreased from 5 minutes after CO2 discharge to the end of surgery. At the time of operation, PetCO2 was remained at a higher level than the initial CO2 level. The peak increase from the moment of pumping CO2 and during the period from T10 to T25. The peak was remained high until T120.
The peak was reduced as soon as CO2 was released and gradually reacheed peak value before CO2 was inflated. Volume of tidal volume (Vt) was decreased slightly at the time of CO2 inflating with the average Vt fell lowest at T30. Vt was then increased immediately after CO2 discharge and gradually progresses to Vt at the time when the surgery was completed.
CONFLICT OF INTERESTS
The authors declare no conflict of interests for the present study.
REFERENCES
1. h t t p : / / w w w . v u s t a . v n / e n / n e w s / Thong_tin_Su_kien_Thanh_tuu_KH_CN/ Phau_thuat_va_phau_thuat_noi_soi_33594.html .
2. Department of Anesthesia, Hanoi Medical University. Anesthesia in Laparoscopic Laparoscopy. Anesthesia Lecture, Medical Publishing House, 2002;311-318.
3. Ton That Quang et al. Clinical characteristics and anesthesia for resuscitation in endoscopic ovarian cysts with intraperitoneal ovary pump. Medical Research, HCMC Medical Publishing House Ho Chi Minh City, 2011;111-140.
4. Huynh Thi Binh et al. (2004), Clinical Technique for Anesthesia, Medical Publishing House, Vol. 31-32.
5. Nguyen Van Chung (2011) "Anesthesia for Resuscitation for Laparoscopic Laparoscopy", Anesthesia Fundamental Anesthesia, Medical Publishing House, Tr 290-307.
6. Tran Binh Giang and Ton That Bach. Laparoscopic Laparoscopic Surgery, Medical Publishing House, 2012; 423.
7. Nguyen Manh Hong and Cong Quyet Thang. Anesthesia for Resuscitation in Laparoscopy, Huu Nghi Hospital in Hanoi; 2008.
8. Le Thi Viet Hoa. Monitoring and care of patients with mechanical ventilation, 01/03/2018, chuabenh.net / hoi-suc-cap-cuu / theo-do-va-cham-soc-benh -nhantho-may.html.
9. Hayel Gharaaibeh. Anaesthetic management of laparoscopic surgery", Eastern Mediterranean Health Journal, 1998;4:185-188.
10. Viale. J-P. La ventilation peropératoire", Congrès national d'anesthésie et de resanimation. Les Essentiels, 2007; 303-313.
FIGURE/TABLES
REFERENCES
1. h t t p : / / w w w . v u s t a . v n / e n / n e w s / Thong_tin_Su_kien_Thanh_tuu_KH_CN/ Phau_thuat_va_phau_thuat_noi_soi_33594.html .
2. Department of Anesthesia, Hanoi Medical University. Anesthesia in Laparoscopic Laparoscopy. Anesthesia Lecture, Medical Publishing House, 2002;311-318.
3. Ton That Quang et al. Clinical characteristics and anesthesia for resuscitation in endoscopic ovarian cysts with intraperitoneal ovary pump. Medical Research, HCMC Medical Publishing House Ho Chi Minh City, 2011;111-140.
4. Huynh Thi Binh et al. (2004), Clinical Technique for Anesthesia, Medical Publishing House, Vol. 31-32.
5. Nguyen Van Chung (2011) "Anesthesia for Resuscitation for Laparoscopic Laparoscopy", Anesthesia Fundamental Anesthesia, Medical Publishing House, Tr 290-307.
6. Tran Binh Giang and Ton That Bach. Laparoscopic Laparoscopic Surgery, Medical Publishing House, 2012; 423.
7. Nguyen Manh Hong and Cong Quyet Thang. Anesthesia for Resuscitation in Laparoscopy, Huu Nghi Hospital in Hanoi; 2008.
8. Le Thi Viet Hoa. Monitoring and care of patients with mechanical ventilation, 01/03/2018, chuabenh.net / hoi-suc-cap-cuu / theo-do-va-cham-soc-benh -nhantho-may.html.
9. Hayel Gharaaibeh. Anaesthetic management of laparoscopic surgery", Eastern Mediterranean Health Journal, 1998;4:185-188.
10. Viale. J-P. La ventilation peropératoire", Congrès national d'anesthésie et de resanimation. Les Essentiels, 2007; 303-313.
ARTICLE INFO
DOI: 10.12699/jfvpulm.9.28.2018.9
Conflict of Interest
Non
Date of manuscript receiving
Date of publication after correction
Article citation
Le Van T, Ta Thanh H. The change of ventilatory function in patients with CO2 inflating in peritoneal cavity for abdominal endoscopic anesthesia surgery. J Func Vent Pulm 2018;27(9):9-14.