
 English
English
 French
French
The role of thoracic ultrasound guidance in supraclavicular brachial plexus block for patients with upper limb surgery at Military Central Hospital 108
Le rôle de l’échographie thoracique guide dans l’anesthésie du plexus brachial chez les patients sous l’opération des member supérieurs à l’Hôpital Militaire Central 108
T. Le Van, T. Tran Phuong
Hai Duong Medical Technical University. Hai Duong, Viet Nam
Corresponding author
Docteur LE VAN Them
Hai Duong Medical Technical University. Hai Duong. Viet Nam
Email : themlv2003@gmail.com
ABSTRACT
Objective. To assess the value of anesthesia of supraclavicular brachial plexus (ASCBP) under thoracic ultrasound guidance in upper limb surgery and to describe its side effect at 108 Military Central Hospital from April to June, 2018.
Methods. It was a perspective study.
Results. The rate of successful anesthesia reached 100%. Quality of pain reduction after anesthesia was good: 47 out of 70 (67.14%) patient without pain, 17 out of 70 (24.29%) patients with mild pain and 6 out of 70 (8.57%) patients with moderate pain.
The majority of patients was satisfied with anesthesia outcome: 45 out of 70 (64.29%) was highly satisfied, 20 out of 70 (28.57%) was satisfied. Vital signs after anesthesia and during surgery was relative stable. Only 1 out of 70 patients occurred side effect which was vascular invasive accounted for 1.43%
Conclusion. The percentage of success ASCBP was high. The quality of analgesia after anesthesia was also important for patients with ASCBP. Finally, the majority of patients were satisfied with the results of specific anesthesia.
KEYWORDS: Anesthesia, brachial plexus, thoracic ultrasound.
RÉSUMÉ
Objectif. Pour évaluer la valeur de l’anesthésie supra-claviculaire du plexus brachial sous échographie thoracique dans la chirurgie des membres supérieurs et décrire son effet secondaire à Hôpital Central Militaire 108 d’Avril à Juin 2018.
Méthodes. C’était une étude en perspective.
Résultats. Le taux d'anesthésie réussie a atteint 100%. La qualité de la réduction de la douleur après l'anesthésie était bonne: 47 patients sur 70 (67,14%) sans douleur, 17 patients sur 70 (24,29%) présentant une douleur légère et 6 patients sur 70 (8,57%) présentant une douleur modérée.
La majorité des patients étaient satisfaits du résultat de l’anesthésie: 45 sur 70 (64,29%) étaient très satisfaits, 20 sur 70 (28,57%) étaient satisfaits. Les signes vitaux après anesthésie et pendant la chirurgie étaient relativement stables. Un seul effet indésirable vasculaire invasif représentait 1,43%.
Conclusion. Le pourcentage de succès ASCBP était élevé. La qualité de l'analgésie après l'anesthésie était également importante pour les patients ayant d'ASCBP. Enfin, la majorité des patients étaient satisfaits des résultats de l’anesthésie spécifique.
MOTS CLÉS: Anesthésie, plexus brachial, échographie thoracique.
INTRODUCTION
The anesthesia of the supraclavicular brachial plexus (ASCBP) is a anesthetic method commonly used in upper limb surgeries [1]. This method has the advantages of regional anesthesia such as ensure good motor and sensitive response inhibition for the requirements of the surgery, patient safety, satisfaction of the surgeon. The patients could avoid an anesthesia and that why they will be less susceptible to respiratory and circulatory effect and postoperative bleeding [2].
In the past, ASCBP is often used as "blind technique" that is based on the anatomical features and the experience of anesthesia and anesthesia with neuromuscular stimulators. However, the nature of neuromuscular anesthesia is still a blind anesthesia according to anatomical landmarks, the pathway and destination of the anesthetic needle is unknown, so the effect is not high and complications are likely to occur [3]. Particularly for patients with obesity, identification of landmarks for local anesthesia is very difficult and there is a risk of failure or complications.
Today, with the advances of modern medicine, the method under the guidance of thoracic ultrasound is gradually being applied and results in high numbness. Under the guidance of thoracic ultrasound, anesthetist will directly observe the nervous system of the arms, arteries, veins, and top of the lung that helps to accurately anesthesia in the ASCBP, ensure the safety, avoid an accidents happening. According to Do et., they studied about ASCBP via sub-clavicle under the ultrasound guideline at Saint Paul Hospital in Hanoi showed a success rate of 100% while the complications were also very low [2].
In the 108 Central Military Hospital, the ASCBP has been applied under the guidance of ultrasound from January 2014 and obtained relatively good results. The assessment of the anesthetic effects and adverse effects in patients with ASCBP is also essential for the anesthetist to monitor, detect and timely manage the events that occur in the course of anesthesia.
From that situation, we conducted this study with the aim of: 1) Evaluation of the anesthetic effect of the ASCBP under the thoracic ultrasound guideline of upper extremity surgery; 2) Describing the undesirable effects of ASCBP under the thoracic ultrasound guideline for upper extremity surgery at the 108 Central Military Hospital from April to June 2018.
METHOD
Study subjects
Criteria for selection of study subjects
• Patients with upper limb surgery by the method of ASCBP under the guidance of thoracic ultrasound.
• Patients agreed to participate in the study.
• Exclusion criteria
• Patients did not agree to participate in the study.
• Patients with neurological disorders.
Methods
Study design
It was a prospective and descriptive study.
Sample size
All patients undergoing upper limb surgery were instructed to undergo thoracic ultrasound at the 108 Central Military Hospital from April to June 2018, which was eligible for the study.
Time and place of study
Time: April to June 2018.
Location: Department of Anesthesiology of 108 Central Military Hospital.
Information gathering techniques
Refer to the combined medical records to ask the patient for information such as name, age, height, weight, ASA, history of the disease, surgical diagnosis, surgical method, satisfaction level patient.
On-line monitoring of vital signs: heart beats, blood pressure, breathing, SpO2.
Direct evaluation of the patient on the results of anesthesia, feeling of paresthesia, level of inhibitory sensation, movement, pain, unwanted effects, etc. by scoring in the collection data sheets.
Some criteria and definitions used in the study
-Hollmen score scale: assessing the degree of inhibitory sensation.
-Judging by the Pin-Prick test by unpointed needle.
Score for evaluating:
• Level 1: needle prick feeling normal.
• Level 2: insertion felt at one point but weaker than the other.
• Level 3: needle prick feels like touching.
• Level 4: needle prick feeling ignorant.
-Evaluation of Modifiel Bromage scale inhibitory activity.
Degree of inhibition
• Grade 0: no suppression - folds the elbows and wrists normally.
• Grade 1: less resistance - normal wrist fold, elbows are only curled around.
• Grade 2: incomplete induction - not elbow, wrist fold.
• Grade 3: complete suppression - complete paralysis.
-VAS pain score (10 points): highest VAS score:
• Level 1: no pain (VAS 0-1p).
• Level 2: low pain (VAS 2-4p).
• Level 3: moderate pain (VAS 5-6p).
• Level 4: severe pain (VAS 7-8p).
• Level 5: very painful (VAS 9-10p).
Data processing and analysis
Data input, processing data by statistical software SPSS 20.0. (Chicago; USA). Data are expressed as mean ± standard deviation or percentage (%).
RESULTS
Clinical characteristics of study subjects
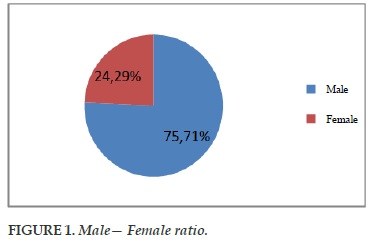
There wer 53/70 male patients, accounting for 75.71%, more than 3 times the number of female patients (17/70), accounting for 24.29% (Figure 1).
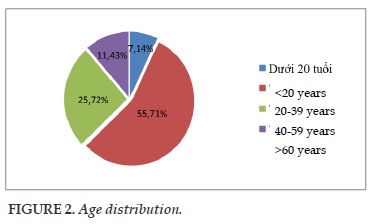
Patients with upper limd surgery were found to be 55.71% in the 20-39 age group and 25.72% in the 40-59 age group, less common in the under 20s and in the elderly (over age 60).
The median age was 37.79±14.33 years, the youngest was 12 years old and the largest was 81 years old (Figure 2).
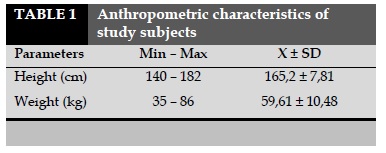
Height was 165.2±7.81 cm, the highest was 182 cm, the lowest was 140 cm. Weight was average 59.61±10.48 kg, the highest was 86 kg, the lowest is 35 kg.
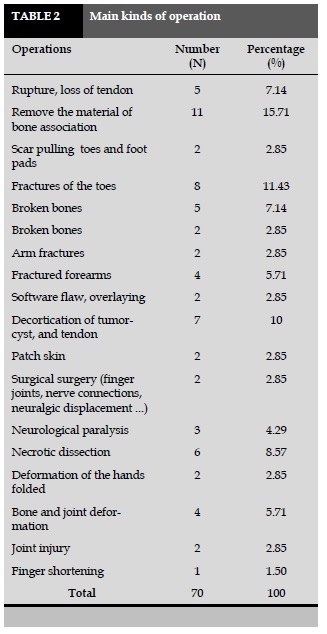
The major surgical removal of the bone (11/70 patients) accounted for 15.71%; fracture surgery (8/70 patients) accounted for 11.43%. There were also different types of surgery with lower rate (Table 2).
The major surgical removal of the bone (11/70 patients) accounted for 15.71%; fracture surgery (8/70 patients) accounted for 11.43%. There were also different types of surgery with lower rate (Table 2).
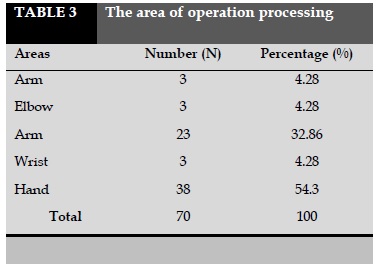
The major operations were on the hands (38/70 patients) were accounted for 54.3% and in the forearm (23/70 patients) accounted for 32.86%. Surgery in the other position was similar and lower (Table 3).
Anesthetic effective assessment
The rate of anesthesia was successful 100% of patients were successfully anesthetized, no cases of anesthesia failed.
Number of needle piercing anesthesia
One time (N=54; 77.14%), 2 times (N=13; 18.57%), 3 times (N=3; 4.29%) for total (N=70; 100%).
Anesthetic medication doses
The average dose of Marcain was 0.89±0.12 (0.6-1.14)mg/kg. The highest dose used was 1.14 mg/kg and the lowest dose used was 0.6 mg/kg.
The average dose of Lidocaine was 1.84±0.39 (1.16-3.19) mg/kg. The highest dose used was 3.19 mg/kg and the lowest dose used was 1.16 mg/kg.
Degree of sensory inhibition when performing Hollmen scale surgery
The level of inhibitory sensation when performing surgery was mainly at level 3 (57/70 patients), accounted for 81.43%. At level 2, there were 11/70 patients, accounting for 15.71% and at the lowest level was 2/70 patients accounted for 2.86%.
Mobility level when conducting surgery on a scale modifiel Bromage scale
The degree of inhibitory activity when surgery was mainly at level 1 (41/70 patients), accounted for 58.57% and the remaining level 2 (29/70 patients) was accounted for 41.43%.
Assessment of pain in surgery on a VAS scale (highest VAS score)
47 out of 70 non-painful patients were accounted for 67.14%. There were 17/70 patients with mild pain, accounting for 24.29% and 6/70 patients with moderate pain, accounting for 8.57%.
Pain relief efficacy: 6 patients with moderate pain (VAS 5-6) achieved good pain relief after taking Midazolam 1-2 mg, 30- 50 mg and Fentanyl 1-2 mcg/kg.
Time insensitivity after anesthesia
The duration of anesthesia was 6.1±1.51 minutes. Maximum time was 9 minutes and minimum was 3 minutes.
The average duration of sensory suppression was 7.49±1.51 minutes. Maximum time was 12 minutes and minimum was 5 minutes. The mean duration of median inhibition was 15.14±2.61 minutes. Maximum time was 20 minutes and minimum was 7 minutes. Average surgery time was 65.64±36.17 minutes. Maximum time was 170 minutes and minimum was 20 minutes.
Evaluation of patient satisfaction
45/70 patients were very satisfied with the anesthesia results (64.29%). There were 20/70 patients satisfied with 28.57% and 5/70 patients at acceptable level accounted for 7.14%. No patients were dissatisfied with the anesthesia.
Undesirable side effect of ASCBP
One of 70 patients with undesirable effects was vessel piercing (1.43%) and no other adverse effects were found. The management: pull out the needle, press for 5 minutes until bleeding stops, then re-put the needle at another location.
DISCUSSION
Characteristics of the study subjects
Gender characteristics
From the results shown in Figure 1, patients undergoing ASCBP under the guide of thoracic ultrasound in surgeries were mainly males with 53 patients, accounting for 75.71% and females 17 patients accounted for 24.29%. The results of another study also showed that the rate of upper limb surgeries in men was higher in women than in the case of Nguyen at the Anesthesiology Department of Hue Central Hospital was 60% and female is 40% [4]. The proportion of patients in male was higher than that in female because the male was the main occupant, therefore, there were more occupational accidents than female. In addition, men used alcohol or beer more easily.
Age: From Figure 2, the average age of patients was highest in the age group of 20-39 years, accounting for 55.71%, followed by the age group 40-59 years, accounting for 25.72%. This can be explained by the fact that in these two age groups, the working-age and occupational accidents, occupational accidents were more than those in the age group of 20 and older (over 60 years old) because they were less engaged in labor and transport.
Weight and height
From Table 1, the mean height of the patients was moderate and was consistent with that of Asians and the weight was not evenly distributed among the patients. The average height of the patient was 165.2 ± 7.81 cm, the mean weight of the patient was 59.61± 10.48 kg, similar to that of Nguyen [4]] had an average height of 161.63±10.46 cm and the average patient weight was 60.36±12.35 kg.
Characteristics of surgery
Table 2 shows that various types of surgery in ASCBP under thoracic ultrasound guide are varied, including various types of surgery such as: dislocations, bone fractures forearm, forearm fracture, tendon rupture, stretching, peeling, cystic, necrotic cut
The surgical site is mainly 1/3 between the arms down because of the fit on the anesthetic [ first]. Specific surgery in the hands (38/70 patients) accounted for 54.3% and in the forearm (23/70 patients) accounted for 32.86%. Surgery in the other position is similar and lower.
Anesthetic effect assessment
The rate of anesthesia is successful
100% of the patients were successfully anesthetized with anesthesia under the guidance of thoracic ultrasound. The rate of successful anesthesia was very high, similar to that of Do et al. [2]. The success rate was 100% was similar to that from Nguyen [4] was 96.70% good and 3.30% fair, and in the study of Phu Cuong Union the success rate was 97.14%.
Number of needle piercing for anesthesia
The results showed that the majority of patients had needle aspiration only once (54/70 patients), accounting for 77.14%; 13/70 patients had two inserted needles, accounting for 18.57% and 3/70 patients had 3 needles inserted 4.29%. Patients with anesthesia with inserted needles had ≥2 times were mainly due to fatty patients, it was difficult to point out neuropathic plexus. Numbness of anesthesia affected the occurrence of undesirable effects but no severe adverse effects occurred fortunately.
Anesthetic dose
The results showed that the average dose of Marcain is 0.89±0.12 mg/kg, the highest dose used was 1.14 mg/kg and the lowest dose used was 0.6 mg/kg. The average Lidocaine dose was 1.84±0.39 mg/kg, the highest dose used was 3.19 mg/kg and the lowest dose used was 1.16 mg/kg. The dosage used is within the recommended range and has a good anesthetic effect.
The degree of inhibition of sensation when performing Hollmen scale
The level of inhibition of sensation during surgery was 3 (57/70 patients), accounting for 81.43%. At level 2 was 11/70 patients accounted for 15.71% and in level 4 was 2/70 patients accounted for 2.86%, in which level 3 and above were good for surgery.
Mobility inhibitory level when performing modified Bromage scale surgery
The results showed that the degree of motor inhibition was 1% (41/70 patients) at 58.57% and the rest at level 2 (29/70 patients) at 41.43%. It found out that at level 1 or more could meet for surgery.
Assessment of pain in surgery on a VAS scale (highest VAS)
The results showed that 47 out of 70 patients without pain was accounted for 67.14%, 17/70 patients had less pain, accounting for 24.29%, there were 6/70 patients with moderate pain and 8.57% showed that the quality of pain relief in ASCBP was relatively good. However, in this study, the patients had more pain than did the study by Do et al. at Saint Paul Hanoi Hospital [2]. The patients with no pain had a rate of 90.63% . Some patients with moderate pain (VAS 5-6 points) appeared in the incision at the beginning of the surgery, possibly due to lack of large number. However, after sedation, Midazolam 1-2 mg, 30-50 mg and Fentanyl 1-2 mcg/kg gave a good pain relief, patients with unmarked pain and could perform surgery normal.
Time for loss sensitivity under ASCBP and surgery
The results showed that the mean anesthesia performing time was 6.1±1.51 minutes, maximum time was 9 minutes and minimum was 3 minutes. Average surgery time was 65.64±36.17 minutes, maximum duration was 170 minutes and minimum was 20 minutes. This time of surgery was suitable for the choice of anesthesia as ASCBP.
Mean duration of sensory suppression was 7.49± 1.51 minutes. Maximum time was 12 minutes and minimum was 5 minutes. The mean duration of median inhibition was 15.14±2.61 minutes. Maximum time was 20 minutes and minimum was 7 minutes. This time difference from the study by Nguyen [4] showed that the duration of sensory inhibition was 5.3±1.53 minutes and the time delay for inhibitory effect the average was 17.76±3.58 minutes. This difference may be due to the use of anesthesia and the volume of anesthetics differed between the two studies [5-7].
Evaluation of patient satisfaction
The results showed that 45 of 70 patients were satisfied with the results of anesthesia, accounting for 64.29%, 20/70 patients were satisfied with 28.57% and 5/70 patients were acceptable, representing 7.14%. No patients were dissatisfied with the anesthesia. The results were nearly equivalent to that of Do et al [2] with 59.38% satisfied patients respectively 37.5% satisfied and 3.12% acceptable.
In a total of 70 patients undergoing anesthesia with ASCBP, there was a case of a patient with a history of vessel piercing but well managed and no unfortunate complications.
CONCLUSION
The percentage of success ASCBP was high. The quality of analgesia after anesthesia was also important for patients with ASCBP. Finally, the majority of patients were satisfied with the results of specific anesthesia.
CONFLICT OF INTERESTS
The authors declare no conflict of interests.
REFERENCES
1. Cong-Quyet T. Anesthesia of brachial plexus. Anes-thesia Resuscitation, Medical Publishing House, Hanoi 2009.
2. Do Thi H. Initial evaluation of the results of neuro-muscular anesthesia on the arm under ultrasoundat Saint Paul Hanoi Hospital", Practical medicine 2013, 860(3):10.
3. Sarkar D, Khurana G, Chaudhary A et al. A Compara-tive Study on the Effects of Adding Fentanyl and Bu-prenorphine to Local Anaesthetics In Brachial Plexus Block. Journal of Clinical and Diagnostic Research 2010. 4: 3337- 3343.
4. Nguyen Viet Q. Evaluating initial results of anesthesia under the guidance of ultrasonography," Medicine Practice 2014,902(1):21-25.
5. Meyer Saklad, M.D., Emery Rovenstine, M.D., and Ivan Taylor, M.D. ASA Physical status Classification System, American Society of Anesthesiologists, Ameri-can 1993.
6. Oates JD, Snowdon SL Failure of pain relief after sur-gery, Anaesthesia 1994, 44:755-758.
7. Paul Warman, Conn D., Nicholls B.et al. Regional An-aesthesia, Stimulation, and Ultrasound Techniques, Oxford Specialist Handbooks in Anaesthesia, Oxford University 2014:79- 96.
FIGURES/TABLES
REFERENCES
1. Cong-Quyet T. Anesthesia of brachial plexus. Anes-thesia Resuscitation, Medical Publishing House, Hanoi 2009.
2. Do Thi H. Initial evaluation of the results of neuro-muscular anesthesia on the arm under ultrasoundat Saint Paul Hanoi Hospital", Practical medicine 2013, 860(3):10.
3. Sarkar D, Khurana G, Chaudhary A et al. A Compara-tive Study on the Effects of Adding Fentanyl and Bu-prenorphine to Local Anaesthetics In Brachial Plexus Block. Journal of Clinical and Diagnostic Research 2010. 4: 3337- 3343.
4. Nguyen Viet Q. Evaluating initial results of anesthesia under the guidance of ultrasonography," Medicine Practice 2014,902(1):21-25.
5. Meyer Saklad, M.D., Emery Rovenstine, M.D., and Ivan Taylor, M.D. ASA Physical status Classification System, American Society of Anesthesiologists, Ameri-can 1993.
6. Oates JD, Snowdon SL Failure of pain relief after sur-gery, Anaesthesia 1994, 44:755-758.
7. Paul Warman, Conn D., Nicholls B.et al. Regional An-aesthesia, Stimulation, and Ultrasound Techniques, Oxford Specialist Handbooks in Anaesthesia, Oxford University 2014:79- 96.
ARTICLE INFO
DOI: 10.12699/jfvpulm.9.28.2018.15
Conflict of Interest
Non
Date of manuscript receiving
Date of publication after correction
Article citation
Le Van T, Tran Phuong T . The role of thoracic ultrasound guidance in supraclavicular brachial plexus block for patients with upper limb surgery at Military Central Hospital 108. J Func Vent Pulm 2018;27(9):15-20.