
 English
English
 French
French
Effectiveness assessment of in vivo and in vitro tests for diagnosing the causes of allergic asthma
Évaluer l'efficacité des test in vivo et in vitro pour diagnostiquer les causes de l'asthme allergique
H. Dinh Thi Dieu1, T. Pham Van2, T. Phung Chi2
1: Hai Duong University of Medical Technology. Hai Duong, Viet Nam
2: Hai Phong University of Medicine and Pharmacy. Hai Phong, Viet Nam
Corresponding author
Pr. PHAM VAN Thuc
Hai Phong University of Medicine and Pharmacy. Hai Phong, Viet Nam
Email : pvthuc@yahoo.com
DOI: 10.12699/jfvpulm.9.28.2018.35
ABSTRACT
Background. In vivo and in vitro tests are commonly used in combination to diagnose allergic conditions, including asthma.
Objectives. To assess the effectiveness of in vivo and in vitro tests in the diagnosis of allergic asthma.
Patients and Methods. There were 100 patients diagnosed with asthma at Haiphong Medical University Hospital and 100 healthy patients with no history of allergy. It was a cross-sectional, descriptive, and control study.
Results. The sensitivity of skin prick-test was 73% and the specificity was 99%; the sensitivity of the intradermal test was 73% and the specificity was 99%; the sensitivity of the leucocyte lysis test was 79%, with 98% specificity; the test of mastocyst degradation had 79% of sensitivity and 98% for specificity; the measurement of specific IgE for Dp was 98%.
Conclusion. In vivo and in vitro tests should be used to diagnose the cause of asthma in health care settings.
KEYWORDS: Allergic asthma, skin test, intradermal test, mastocyst degradation, leucocyte lysis.
RÉSUMÉ
Introduction. Les test in vivo et in vitro sont généralement combinés, appliqués pour diagnostiquer des maladies allergiques, y compris l'asthme.
Objectif. Pour évaluer l'efficacité des test in vivo et in vitro pour diagnostiquer les causes de l'asthme allergique.
Sujet et méthode de l'étude. 100 patients qui ont été diagnostiqués déterminées l'asthme allergique, examinés et traités à l'hôpital de l'Ecole de médecine de Hai Phong; et 100 personnes en bonne santé, sans antécédents d'allergie. Etude transversale décrite avec éléments de preuve.
Résultat. La sensibilité du prick-test est de 73% et la spécificité est de 99%; la sensibilité du test d'intradermoréaction est de 73% et une spécificité de 99%; la sensibilité de la réaction leucocytolyse spécifique est de 79% et une spécificité de 98%; la sensibilité de le réaction mastocytolyse est de 79% et une spécificité de 98%; le teneur d'IgE spécifique est compte de 98% pour l'allergène Dp.
Conclusion. Utiliser le test in vivo et in vitro pour le diagnostic déterminé les causes d'asthme aux établissements de santé.
MOTS CLÉS: Asthme allergique, test cutané, test intradermique, dégradation de mastocytes, lyse de leucocytes.
INTRODUCTION
Asthma is a chronic inflammatory disease of the airways with many cells and biomolecular factors involved. The study on the effective and qualitative methods of diagnosis and treatment of asthma suitable to the real situation in our country is the striving of the specialized scientists.
At present, in Hai Phong, there is no study evaluating the effectiveness of in vivo and in vitro tests for the diagnosis of allergic asthma. With the desire to contribute to improve the quality of diagnosis of asthma in real condition of Hai Phong, we conducted this study with the following two objectives: to evaluate the effectiveness of in vivo and in vitro tests in diagnosing the cause of allergic asthma.
METHOD
Study subjects
One hundred patients were diagnosed with asthma at Hai Phong Medical University Hospital. Control group: including 100 healthy people with no history of allergy.
Study materials: 20 French and Vietnamese allergens.
It was a cross-sectional, descriptive, and control study, conducted from July 2010 to Juin 2016.
RESULTS
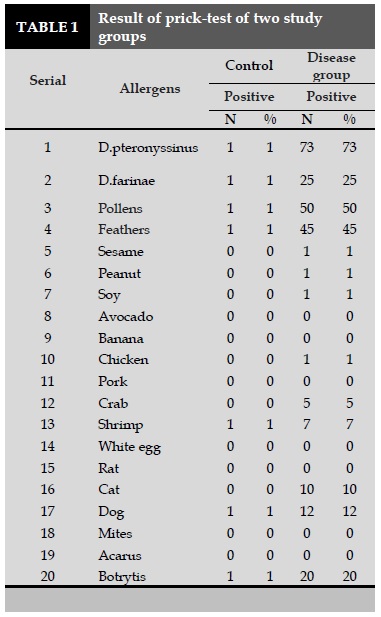
Skin prick-tests
In the control group, seven patients showed a positive reaction to the study allergens.
In the study group, the skin prick test showed that house dust mite was the highest positive (73%), followed by pollens (50%), feathers (45%), D. farinae (25%), dog hair (12%), cat hair (10%), and fungal allergen (20%). Many allergic patients were positive for multiple allergens (Table 1).
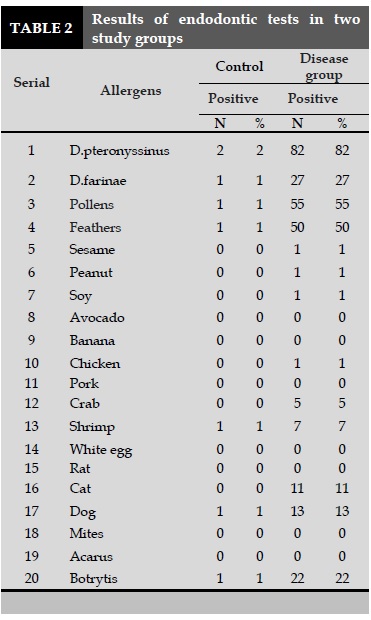
Intradermic tests
In the control group, 8 patients showed a positive reaction to the study allergens. In the study group, the endometrial test showed that D. pteronyssinus had the highest positive rate (82%), followed by pollens (55%), feathers (50%), D. farinae (27%), dog hair (13%), cat hair (11%), fungal allergens also accounted for a relatively high proportion (22%). Many patients were positive for multiple allergens.
In vitro tests
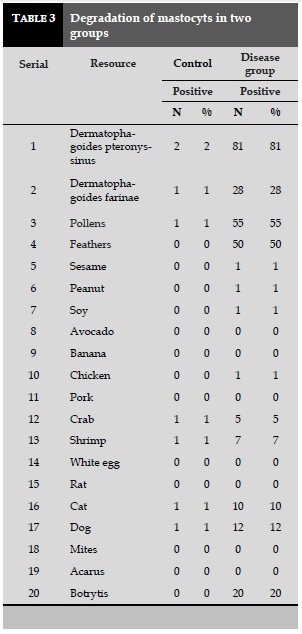
Degradation of mastocysts (Table 3)
In the control group, seven patients showed a positive reaction to the study allergens. In the study group, the degradation of mastocyts showed the highest rate with house dust mites (81%), followed by pollens (55%), and feathers (50%).
Dog hairs (12%), cat hairs (10%), and fungal allergens were also accounted for a relatively high proportion (20%). Many patients are positive for multiple allergens.
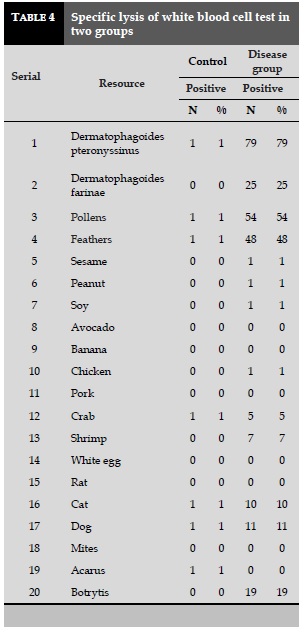
Specific lysis of white blood cells (Table 4)
In the control group, seven patients showed a positive reaction to the study allergens.
In the group of patients with specific lysis of white blood cell responses, the house dust mites were exhibited the highest positive rate (79%), followed by pollens (54%), feathers (48%).
Dog hairs (11%), cat hair (10%), fungal hyphae also accounted for a relatively high proportion (19%).
Many patients are positive for multiple allergens.
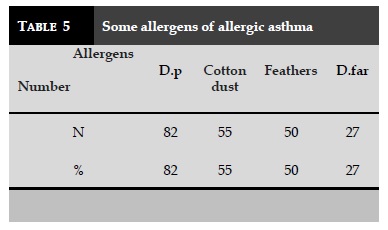
Some common allergens cause allergic asthma (Table 5)
Through a study of 100 allergic asthmatic patients questioned for medical history of allergy and in vivo and in vitro tests: skin pricks test, intradermal test, mastocyt degradation, and specific lysis of white blood cells, we found out that patients were allergic to some of allergens as presented in Table 5.
The most common allergens of allergic asthmatic patients were Dermatophagoides pteronyssinus (Dp) for 82%, 55% of pollens, 50% of feathers, and 27% with D.far (Table 5).
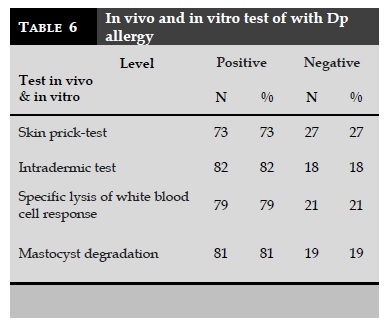
In the same patient with Dp allergy, we found that the highest rate of intradermic test was 82%, followed by mastocyst degradation was 81%, 79% of specific lysis of leukocytes, and 73% of skin prick-test.
Specific IgE quantification
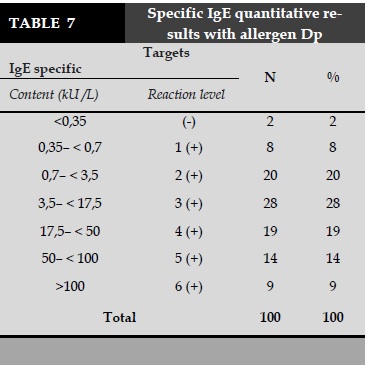
In the process of making in vivo and in vitro tests for 100 allergic asthma patients, we found that 82% of patients were allergic with common causes of allergens were caused by Dermatophagoides pteronyssinus. Thus, we only conducted the specific IgE quantification for 100 asthmatic patients with Dermatophagoides pteronyssinus as allergen to determine the exact cause of the disease.
More than 100 patients with allergic asthma who had the measurement of IgE-specific for Dp allergy, we found out 98 patients were positive or 98%. The highest positive level (+3) was 28%, followed by +2 for 20%, +4 for 19%, and +6 was significantly for 9%; while positive +1 was lowest with 5%.
DISCUSSION
All foreign authors documented that skin prick-test is a simple diagnostic method that is technically feasible, easy to apply, cheap, painless, and highly accurate. Even though many cases of skin prick-test are positive for people who do not have allergies, they may develop allergic reactions if they have a long-term follow-up. Thus, skin prick-test is the primary tool and is performed firstly to diagnose allergies. The results of skin prick-test is an important and basis evidence for the diagnosis and treatment of allergic conditions. According to many authors, this test has greater reliability than intradermal test due to less false positive cases [1,2].
Today, skin prick-test is still widely used in many countries [3,4], in our study we conducted skin prick-test with diagnostic criteria to make the basis for the recruitment. All patients who were clinically examined and were tested with standard allergens, then selected in the present study if having positive allergen confirming by skin prick-test.
The results of the skin prick-test in the present study showed that among conducted skin test for 100 normal people: 7% positive at level +1, this rate was equivalent to the result of some national and foreign authors [5].
In the group of patients, the results showed that skin prick-test for 100 asthmatic patients with 20 allergens to determine the cause of the disease. In our study, D.pteronyssinus was the causative agent of the highest proportion (73%), followed by pollens (50%), feathered (45%), D.far (25%). The fungus also played an important role in the positive rate (20%). Our result is consistent with the findings of other author [6]. It showed that when conducting skin prick test with Dp for asthmatic patients, the number of patients with positive results was 68.85%. During the test, no complications occurred. This is a safe, simple, easy-to-apply diagnostic method in medical facilities with relatively high accuracy. An intradermal test was performed for 100 asthmatic patients. The results showed that up to 82% of the patients were positive for Dp allergens, followed by pollens (55%), feathers (50%). There were many patients who were also positive for many different allergens.
The intradermal test realized for 100 healthy people who did not history of allergy or never did allergic diseases previously, the results showed that there were 8 patients positives for intradermal test, 92 patients were negatives. The specificity of this test in our study was high (92%).
Thus, intradermal the test having the result was higher than the skin prick-test. Why is there a difference in the level of skin prick-test and intradermal test? In our opinion, skin prick-test gives only minimizes skin damage and the amount of allergens is also minimal (soaking), so it is less likely to directly stimulate the skin to produce false positives. In other words, the positive result of it is that it honestly reflects the patient's true allergy status to the test antigen. In contrast, intradermal test causes much greater skin damage (due to needles); moreover, the volume of the allergen is quite large and under pressure. Therefore, the possibility of false positives is higher than that of skin prick-test.
We conducted the mastocyst degradation for 100 patients with allergic asthma, and 100 healthy subjects with no medical history of allergy and allergic diseases. The results showed that the negative control group was 93%, the positive rate was 7%. Thus, even in the control group, there was a certain positive rate of mastocyst degradation, with a specificity of 94%. In disease group, the highest positive for Dp allergen was 81%, pollens for 55%, and feathers for 50%. Mastocyst degradation is an in vitro test that is usually done in large medical facilities, due to its complex techniques and method. If the mastocyst degradation is done with standard method, the result will be with a high accuracy. According to previous authors, this is a test commonly used in the diagnosis and monitoring of specific immune therapy with special allergens in allergic diseases at the department of immunological and allergology.
In addition to conducting mastocyst degradation we conducted a specific leucocyte (white blood cell) lysis reaction for 100 asthmatic patients and 100 healthy controls. The results showed that in control subjects, there were 93% of negative and 7% of positive subjects; therefore the specificity was 93%. In disease group, the highest positive for Dp allergen was 79%, pollens for 54%, and feathers for 48%.
As the same with mastocyst degradation, the reaction of white blood cells lysis is tested or done at centers specializing in allergy, high-value test when done by experienced technicians. Combined with skin prick-test, intradermal test, and mastocyst degradation, the leucocyte lysis testing are used for the diagnosis and monitoring of the efficacy of allergic immunodeficiency with allergens.
The specific IgE quantitative measurement is a specific method in the field of immunologic diagnosis. This is the 'gold standard' that confirms the diagnosis of an allergy to any allergen. This test is usually done when conventional, easy-to-perform tests such as skin prick-test, intradermal test, mastocyst degradation, and specific or non-specific white blood cell lysis have a suspected results. Thus, when the history of the disease is consistent with in vivo and in vitro testing, specific IgE levels are not needed to confirm the diagnosis if the economic condition is difficult due to the specific IgE quantification technique that is expensive.
However, this test have many advantages due to here is no incident for the patient; it can detect the false positive of skin prick-test (eg. dermatographisme); it is not affected by drugs used by patients; it can be performed in patients with skin conditions. The IgE quantification technique have also some disadvantages such as it is costly and time consumable; the results of specific IgE quantitative test are based on some following factors such as the quality allergens or the quality of the technique. During in vivo and in vitro tests for 100 patients with allergic asthma, there was 82% of patients with asthma were allergic to Dermatophagoides pteronyssinus allergens. Therefore, we only conducted the specific IgE measurement with Dp allergens in 100 patients with allergic asthma. The result showed that up to 98% of serum IgE-positive in asthmatic patients were positive for Dp. The highest positive rate at +3 was 28%, +2 was 20%, +4 was 19%, and positive with +1 had the lowest rate of 8%.Comparing IgE specificity measurement with other in vivo and in vitro tests, we found out the significant differences with P <0.01. Thus, IgE dosage is the most accurate, it is considered the gold standard in the diagnosis, monitoring, and prognosis of allergic diseases, including allergic asthma.
CONCLUSION
Based on the results of some in vivo and in vi- tro tests in the diagnosis of bronchial asthma in Hai Phong with 200 subjects, we conclude that the skin prick-test has a high sensitive and specificity as the same with intradermal test for Dp allergen. Where as the mastocyst degradation and specific IgE measurement also have the high specificity for Dp allergens.
CONFLICT OF INTERESTS
The authors declare no conflict of interest.
REFERENCES
1. Nguyen The Hung, Le Tuan Linh, Nguyen Trong Hieu et al. Applying some specific allergy diagnostic methods for detecting bronchial asthma due to house dust; 1999.
2. Robison D.S, Durham S.R. Mechanisms in asthma, Medicine International, 1995;9 (31), 265-269.
3. Vu Minh Thuc, Pham Van Thuc. Laboratory Methods in Immuno-allergy Research, Medical Publishing House 2005.
4. American Academy of Allergy. Asthma and Immu-nology" The allergy report. Miwaukee, WI: AAAAI; 2006.
5. Trinh Manh Hung. Some initial results on the diagno-sis and treatment of asthma bronchial asthma, disser-tation doctor of medicine, Hanoi Medical University 2000.
6. Vu Minh Thuc. Clinical characteristics and value of in vivo test for diagnosis of occupational asthma bron-chial asthma due to dust" Occupational health and environment, Vietnamese medicine 2005; 40-49.
TABLES
REFERENCES
1. Nguyen The Hung, Le Tuan Linh, Nguyen Trong Hieu et al. Applying some specific allergy diagnostic methods for detecting bronchial asthma due to house dust; 1999.
2. Robison D.S, Durham S.R. Mechanisms in asthma, Medicine International, 1995;9 (31), 265-269.
3. Vu Minh Thuc, Pham Van Thuc. Laboratory Methods in Immuno-allergy Research, Medical Publishing House 2005.
4. American Academy of Allergy. Asthma and Immu-nology" The allergy report. Miwaukee, WI: AAAAI; 2006.
5. Trinh Manh Hung. Some initial results on the diagno-sis and treatment of asthma bronchial asthma, disser-tation doctor of medicine, Hanoi Medical University 2000.
6. Vu Minh Thuc. Clinical characteristics and value of in vivo test for diagnosis of occupational asthma bron-chial asthma due to dust" Occupational health and environment, Vietnamese medicine 2005; 40-49.
ARTICLE INFO
DOI: 10.12699/jfvpulm.9.28.2018.35
Conflict of Interest
Non
Date of manuscript receiving
Date of publication after correction
Article citation
Dinh Thi Dieu H, Pham Van T, Phung Chi T. Effectiveness assessment of in vivo and in vitro tests for diagnosing the causes of allergic asthma . J Func Vent Pulm 2018;27(9):35-40.