
 English
English
 French
French
Study of clinical characteristics of obstructive sleep apnea syndrome (OSA) in patients with COPD
Étude sur les caractéristiques cliniques du syndrome d'apnée obstructive du sommeil (SAOS) chez des patients atteints de BPCO
Luu Minh Chau1, T. Tran-Thi-Khanh2, S. Duong Quy3,4
1 ; Vietnam University of Traditional Medicine. Hanoi, Vietnam.
2; Pham Ngoc Thach University of Medicine. Ho Chi Minh city, Vietnam
3; Clinical Research Center. Lam Dong Medical College. Vietnam
4: Penn State Medical College. Hershey Medical Center. USA
Corresponding author
Dr. LUU MINH Chau
Vietnam University of Traditional Medicine. Hanoi - Vietnam
Email: minhchauytdp@gmail.com
ABSTRACT
Background. Obstructive sleep apnea syndrome (OSA) is often associated with chronic obstructive pulmonary diseases (COPD), making sleep disturbances, hypoxemia at night, and daytime hypercapnia are more severe.
Objective. This study was planned to evaluate the prevalence of OSA in COPD patients in compare to control subjects and its clinical characteristics.
Methods. 122 smokers were included and divided into 2 groups: control group (without COPD; N=31), COPD group (N=91). All subjects underwent clinical examinations, spirometry, and polysomnography, Pichot and Epworth scales.
Results. Mean ages of study subjects were not different between 2 groups. The prevalence of OSA in COPD was higher than control subject (24% vs. 9%). The micro arousals and AHI in COPD patients were higher than control subjects . Nadir SpO2 in COPD patients was significantly lower than control subjects (84±7% vs. 91±4%). The percentage of COPD patients having snoring at sleep, SpO2 <90% and <85% were higher than control group. There were significant correlations between AHI with snoring at sleeps, nysturia, and Epworth scores.
Conclusion. The prevalence of OSA is higher in COPD than general population. It is the cause of high morbidity and mortality in patients with COPD.
KEYWORDS: Sleep apnea, COPD, polysomnography, Epworth, Pichot.
RÉSUMÉ
Introduction. Le syndrome d'apnées obstructives du sommeil (SAOS) est souvent associé à la bronchopneumopathie chronique obstructive (BPCO), ce qui entraîne des troubles du sommeil, une hypoxémie nocturne et une hypercapnie diurne plus graves.
Objectif. Cette étude avait pour but d'évaluer la prévalence de l'SAOS chez les patients atteints de BPCO par rapport aux sujets témoins et ses caractéristiques cliniques.
Méthodes. 122 fumeurs aient été inclus et répartis en 2 groupes: groupe témoin (sans BPCO; N=31), groupe BPCO (N=91). Tous les sujets ont subi des examens cliniques, spirométrie et polysomnographie, échelles de Pichot et Epworth.
Résultats. L'âge moyen des sujets à l'étude n'était pas différent entre 2 groupes. La prévalence de l'SAOS dans la BPCO était supérieure à celle du sujet témoin (24 vs 9%). Les micro-éveils et l'IAH chez les patients atteints de BPCO étaient plus élevés que chez les témoins. Nadir SpO2 chez les patients atteints de BPCO était significativement plus faible que les sujets témoins (84±7% vs 91±4%). Le pourcentage de patients atteints de BPCO qui ronflait pendant leur sommeil, dont la SpO2 <90% et <85%, était supérieur à celui du groupe témoin. Il existait des corrélations significatives entre l'IAH et le ronflement au sommeil, la nysturie et les scores d'Epworth.
Conclusion. La prévalence de l'SAOS est plus élevée dans la BPCO que dans la population générale. C'est la cause d'une morbidité et d'une mortalité élevées chez les patients atteints de BPCO.
MOTS CLÉS: Apnée du sommeil, BPCO, polysomnographie, Epworth, Pichot.
INTRODUCTION
The combination of obstructive sleep apnea syndrome (OSA) and chronic obstructive pulmonary disease (COPD) is known as "overlapping syndrome" (OLS: overlap syndrome) was first described in the 1980s [1]. OSA is characterized by apnea – short of breath at sleep with severe hypoxemia, leading to pulmonary hypertension, chronic heart failure, and increased carbon dioxide at day time. These effects can lead to sleep disorders and disease progression of COPD patients [2-4]. The sleep disorders of patients with overlapping syndrome are more common and significant than those with COPD alone. The presence of OSA and COPD will increase the effect of each disease on sleep patterns and exacerbate hypoxia at night and increase carbon dioxide at daytime [5]. As a result, COPD patients with OSA have a higher risk for acute respiratory failure and a higher risk of cardiovascular morbidity and mortality. In Vietnam, COPD is an important public health problem because of the high prevalence associated with smoking habit. Therefore, early detection of OSA in patients with COPD is essential for timely treatment.
OBJECTIVES
This study was conducted to assess: 1) the incidence of COPD suffering from OSA; 2) clinical and functional features of OSA in COPD patients.
METHODS
Study subjects
The study subjects were 122 adult who volunteered to participate in the study. They were divided into 2 groups: control group (N=31) and COPD group (N=91). Control group: subjects without COPD; COPD: included patients with COPD and meets the following criteria: cigarette smoking, clinical COPD symptoms (cough, sputum, dyspnea on exertion), with airway obstruction, determined by standard spirometry and GOLD severity scales: forced expiratory volume in one second (FEV1) / forced vital capacity (FVC) after bronchodilator inhalation <70%.
Exclusion criteria for both groups: people with other acute or chronic diseases that have been diagnosed and treated such as diabetes, chronic kidney failure, sequelae of cerebrovascular accident, asthma, hypertension, acute sinusitis disease, symptomatic cardiovascular diseases, chronic or acute insomnia.
Methods
This was a descriptive and cross-sectional study at a given time. All parameters of clinical characteristics, function and polysomnography (PSG) were recorded for analysis.
Study subjects’ clinical examination was done; the respiratory function and ECG were measured and blood chemistry tests were done. Sleepiness and daytime fatigue were assessed using the Epworth score (0-24 points) and Pichot score (0-32 points). Measurement of respiratory function was done by Body Box (Medisoft; USA). The bronchial reversibility test was performed with Ventolin sprays, 400 μg and re-measured after 15 minutes.
Polysomnography (PSG) was performed by Alice PDx (Philippe Respironic, USA). Recognized parameters include EEG for C4-A1, C3-A2, O2-A1 and O1-A2; Electromyography (EMG), electrocardiogram (ECG); air outflow in the nose and mouth; exhalation pressure at the nose; abdominal movement; sleep position; oxygen saturation; waking and snoring index; Sleep Efficiency. Recorded parameters were processed by Alice Sleepware (Philippe Respironic, USA). Sleep periods and apnea-hypopnea indexes (AHI) were classified according to the recommendations of the American Sleep Apnea Association.
Statistical analysis
Recorded parameters were presented as mean ± SD. Statistical analysis was performed on SPSS software, version 20.0. Comparing quantitative parameters was done by t-Student test. The difference was significant when P<0.05.
RESULTS
Clinical and function characteristics of study subjects
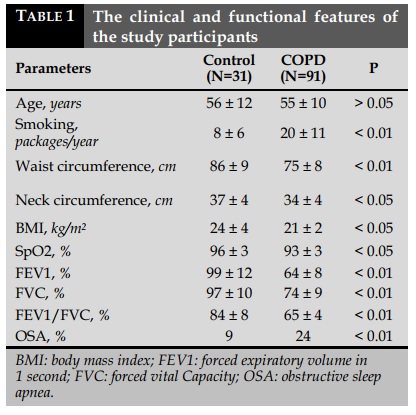
During the time of July 2016 and December 2017, a total of 121 subjects participated in the study, including 31 subjects without COPD and 91 eligible COPD patients. The clinical and functional features of the study participants are presented in Table 1.
Polysomnography (PSG) features of study participants
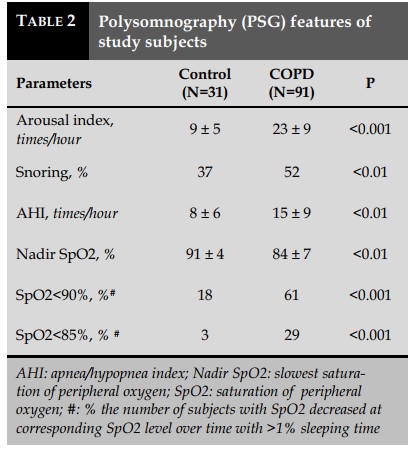
Polysomnography (PSG) features of study participants are presented in Table 2. The COPD group had a higher arousal index, a higher rate of apnea-hypopnea than the control group. The incidence of COPD patients with snoring and decreased SpO2 <90% and <85% was higher than control group.
Clinical features related to OSA in patients with COPD
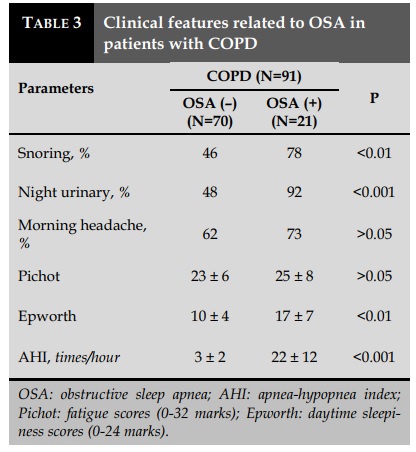
Clinical features of OSA-related to COPD patients are presented in Table 3. The proportion of COPD
DISCUSSION
The results of the study showed that the proportion of COPD patients with OSA is higher than those without COPD (Table 1). Although there is no difference in age and gender, the COPD group had lower BMI than the control group without COPD. The result also showed that patients with COPD with poor patients with OSA having snoring, nighttime urinary was significantly higher than non-OSA COPD patients. There was no significant difference between COPD patients with and without OSA in morning headache and Pichot daytime fatigue scores.
Correlation between AHI and clinical outcomes in COPD patients with OSA
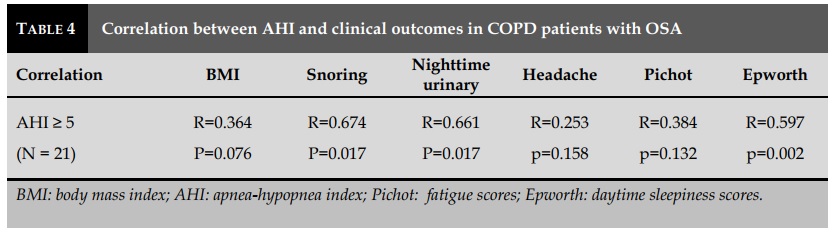
The correlation between OSA syndrome (AHI≥5) and clinical symptoms in patients with COPD is presented in Table 4. There was a significant correlation between AHI with snoring, nighttime urinary and Epworth scores sleep quality presented in arousal index was significantly higher than those in the control group (Table 2). The rate of COPD patients with snoring, AHI and hypoxemia at night was also higher than controls.
Other studies have also shown that COPD patients with OSA had significantly lower levels of oxygen saturation than non-OSA patients with COPD in spite of the same level of bronchial obstruction [6]. This is also a feature that aggravates cardiovascular disease due to hypoxemia in some patients with COPD and increases cardiovascular complications [7-12].
In terms of clinical symptoms, in COPD patients with OSA, the rates of snoring, nighttime urination and daytime sleepiness, assessed by Epworth scores, were higher and significantly correlated with AHI (Table 3-4). These are very helpful symptoms in screening OSA in COPD patients [13-17]. Other common symptoms in OSA in the general population such as obesity, morning headache, and daytime fatigue are not significantly associated with AHI in COPD patients. Therefore, PSG should be performed in COPD patients with suspected symptoms of OSA.
CONCLUSION
Obstructive sleep apnea syndrome is more common in COPD patients than in the general population. This causes more complications and mortality of patients with COPD. OSA syndrome should be routinely screened in patients with COPD for appropriate treatment [18-21].
CONFLIT OF INTEREST
Non.
REFERENCES
1. Chaouat A, Weitzenblum E, Kessler R, Schott R, Charpentier C, Levi-Valensi P, Zielinski J, Delaunois L, Cornudella R, Moutinho dos Santos J: Outcome of COPD patients with mild daytime hypoxaemia with or without sleep-related oxygen desaturation. Eur Respir J 2001; 17 : 848-55.
2. Chaouat A., Weitzenblum E., Krieger J., Ifoundza T., Oswald M., Kessler R. Association of chronic obstructive pulmonary disease and sleep apnea syndrome. Am Rev Respir Dis 1995; 151 : 82-86.
3. Cully J.A., Graham D.P., Stanley M.A., Ferguson C.J., Sharafkhaneh A., Souchek J., et al. Quality of life in patients with chronic obstructive pulmonary disease and comorbid anxiety or depression. Psychosomatics 2006; 47 : 312-319.
4. Duran J., Esnaola S., Rubio R., Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 years. Am J Respir Crit Care Med 2001; 163: 685-9.
5. Flenley D.C. Sleep in chronic obstructive lung disease. Clin Chest Med 1985; 6 : 51-61.
6. Vos P.J.E., Folgering H.T.M., Van Herwaarden C.L.A. Predictors for nocturnal hypoxaemia (mean SaO2 <90 %) in normoxic and mildly hypoxic patients with COPD. Eur Respir J 1995; 8: 74-77.
7. Baud D. Treatment of sleep apnea syndrome by positive pressure at night. J Func Vent Pulm 2014;05(14):1824.
8. Bouchentouf R. The obstructive sleep apnea-hyponea syndrome (OSAHS). J Func Vent Pulm 2014;05(14):1217 .
9. Nguyen Xuan Bich H. Obstructive sleep apnea syndrome (OSAS) and arterial hypertension. J Func Vent Pulm 2014;05(14):1-2.
10. Duong-Quy S, Vu-Minh T, Homasson J.P, Martin F , Soyez F. Study of diagnostic value of RU Sleeping in screening of obstructive sleep apnea syndrome. J Func Vent Pulm 2013;04(13):30-34.
11. Bacha S, Habibech S , Chaouch N. Profil clinique du syndrome d’apnées obstructives du sommeil. J Func Vent Pulm 2017;24(8):18-23.
12. Ad j oh. KS, Ad a mboun ou. AS, Gbadamassi. AG,Efalou. P, Ouedraogo. AR, Aziagbe. KA, Foma. W, Dolou. W, . Dijibril. MA, Belo. M. J Func Vent Pulm 2017; 24(8): 10-17.
13. Nguyen-Thi-Hong L, Duong-Quy S. Obstructive Sleep Apnea Syndrome: The challenges in developing countries. J Func Vent Pulm 2016;22(7):1-2 .
14. A d a m b o u n o u . A S , A d j o h . K S , Aziagbé. KA, Foma. W, Gbadamassi. AG, Tougan. A, Djibril. M, Belo. M, pémissi. E, Tidjani. O; Prevalence of symptoms of sleep apnea syndrome in Lome. J Func Vent Pulm 2016; 22(7):32-39.
15. Adambounou.AS, Adjoh. KS, Ouédraogo.AR, et al. Current state of knowledge and attitudes of physicians in Lome on sleep apnea syndrome. J Fran Viet Pneu 2016;21(7):7-14.
16. Ho-Viet T.D, Soyez F. Role of mandibular advancement devices in management of obstructive sleep apnea syndrome (OSAS). J Fran Viet Pneu 2015;17(6):23.
17. Duong-Quy S. Sleep disorder in COPD: a forgotten entity. J Fran Viet Pneu 2015;19(6):1.
18. Nguyen Thi Thanh P, Mai Thi Thanh T, Kim Xuan L. The quality of sleep in patients with COPD in Pham Ngoc Thach hospital - HCM city. J Fran Viet Pneu 2015;19(6):44-48.
19. Hua-Huy T. Obstructive sleep apnoea syndrome (OSAS): on the right method for screening. J Func Vent Pulm 2014;05(15):3-4.
20. Préfaut C. Physiopathology of chronic obstructive pulmonary disease - COPD. J Func Vent Pulm 2013;04 (13):6-13.
21. D’Ortho MP. Sleep apnea syndrome in patient with heart failure. J Func Vent Pulm 2013;04(13):25-29.
TABLES
REFERENCES
1. Chaouat A, Weitzenblum E, Kessler R, Schott R, Charpentier C, Levi-Valensi P, Zielinski J, Delaunois L, Cornudella R, Moutinho dos Santos J: Outcome of COPD patients with mild daytime hypoxaemia with or without sleep-related oxygen desaturation. Eur Respir J 2001; 17 : 848-55.
2. Chaouat A., Weitzenblum E., Krieger J., Ifoundza T., Oswald M., Kessler R. Association of chronic obstructive pulmonary disease and sleep apnea syndrome. Am Rev Respir Dis 1995; 151 : 82-86.
3. Cully J.A., Graham D.P., Stanley M.A., Ferguson C.J., Sharafkhaneh A., Souchek J., et al. Quality of life in patients with chronic obstructive pulmonary disease and comorbid anxiety or depression. Psychosomatics 2006; 47 : 312-319.
4. Duran J., Esnaola S., Rubio R., Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 years. Am J Respir Crit Care Med 2001; 163: 685-9.
5. Flenley D.C. Sleep in chronic obstructive lung disease. Clin Chest Med 1985; 6 : 51-61.
6. Vos P.J.E., Folgering H.T.M., Van Herwaarden C.L.A. Predictors for nocturnal hypoxaemia (mean SaO2 <90 %) in normoxic and mildly hypoxic patients with COPD. Eur Respir J 1995; 8: 74-77.
7. Baud D. Treatment of sleep apnea syndrome by positive pressure at night. J Func Vent Pulm 2014;05(14):1824.
8. Bouchentouf R. The obstructive sleep apnea-hyponea syndrome (OSAHS). J Func Vent Pulm 2014;05(14):1217 .
9. Nguyen Xuan Bich H. Obstructive sleep apnea syndrome (OSAS) and arterial hypertension. J Func Vent Pulm 2014;05(14):1-2.
10. Duong-Quy S, Vu-Minh T, Homasson J.P, Martin F , Soyez F. Study of diagnostic value of RU Sleeping in screening of obstructive sleep apnea syndrome. J Func Vent Pulm 2013;04(13):30-34.
11. Bacha S, Habibech S , Chaouch N. Profil clinique du syndrome d’apnées obstructives du sommeil. J Func Vent Pulm 2017;24(8):18-23.
12. Ad j oh. KS, Ad a mboun ou. AS, Gbadamassi. AG,Efalou. P, Ouedraogo. AR, Aziagbe. KA, Foma. W, Dolou. W, . Dijibril. MA, Belo. M. J Func Vent Pulm 2017; 24(8): 10-17.
13. Nguyen-Thi-Hong L, Duong-Quy S. Obstructive Sleep Apnea Syndrome: The challenges in developing countries. J Func Vent Pulm 2016;22(7):1-2 .
14. A d a m b o u n o u . A S , A d j o h . K S , Aziagbé. KA, Foma. W, Gbadamassi. AG, Tougan. A, Djibril. M, Belo. M, pémissi. E, Tidjani. O; Prevalence of symptoms of sleep apnea syndrome in Lome. J Func Vent Pulm 2016; 22(7):32-39.
15. Adambounou.AS, Adjoh. KS, Ouédraogo.AR, et al. Current state of knowledge and attitudes of physicians in Lome on sleep apnea syndrome. J Fran Viet Pneu 2016;21(7):7-14.
16. Ho-Viet T.D, Soyez F. Role of mandibular advancement devices in management of obstructive sleep apnea syndrome (OSAS). J Fran Viet Pneu 2015;17(6):23.
17. Duong-Quy S. Sleep disorder in COPD: a forgotten entity. J Fran Viet Pneu 2015;19(6):1.
18. Nguyen Thi Thanh P, Mai Thi Thanh T, Kim Xuan L. The quality of sleep in patients with COPD in Pham Ngoc Thach hospital - HCM city. J Fran Viet Pneu 2015;19(6):44-48.
19. Hua-Huy T. Obstructive sleep apnoea syndrome (OSAS): on the right method for screening. J Func Vent Pulm 2014;05(15):3-4.
20. Préfaut C. Physiopathology of chronic obstructive pulmonary disease - COPD. J Func Vent Pulm 2013;04 (13):6-13.
21. D’Ortho MP. Sleep apnea syndrome in patient with heart failure. J Func Vent Pulm 2013;04(13):25-29.
ARTICLE INFO
DOI: 10.12699/jfvpulm.9.29.2018.15
Conflict of Interest
Non
Date of manuscript receiving
23/6/2018
Date of publication after correction
15/12/2018
Article citation
Minh Chau Luu, Tran-Thi-Khanh T, Duong Quy S. Study of clinical characteristics of obstructive sleep apnea syndrome (OSA) in patients with COPD. J Func Vent Pulm 2018;29(9):15-18.