
 English
English
 French
French
Evaluation of the management of asthma in a specialized pulmonological environment at CHU Congo-Brazzaville
Evaluation de la prise en charge de l'asthme dans un environnement pneumologique spécialisé au CHU Congo-Brazzaville
FH. Okemba Okombi1, A. Fiogbe Attanon2, P. Koumeka1, GR. Bopaka1, KB. Ossale Abacka1, ELP. Bemba1, S. Adjoh Komi2
1: Department of Pulmonology University Hospital of Brazzaville. Faculty of Health Sciences. Marien University Ngouabi. Congo
2: Department of Pneumo-Phtisiology CHU Sylvanus Olympio. Lomé. Togo
Corresponding author
Dr. OKEMBA OKOMBI Franck Hardain
Faculty of Health Sciences. Marien University Ngouabi. Congo.
Email: franckokemba@gmail.com
ABSTRACT
Introduction and Objective. Asthma is a chronic inflammatory disease of the bronchi that requires a codification of its management by pulmonologists. Due to lack of consensus of care at the national level, we have allowed ourselves to make an assessment of the care that is conducted in the respiratory department of the University Hospital of Brazzaville to better define the axes of care.
Methods. We analyzed data recording in the Asthma Crisis or Exacerbation Service and the controls performed during the study period.
Results. In total, we analyzed the management of 54 patients during this period. They were 60% women and 40% men, mostly young, with an average age of 25.6 years (extreme: 19 years and 62 years). No use of peak-flow was made for the assessment of the severity or not of the crisis. Bronchodilators in solution for nebulization were used in 35% of cases and forms for injection (subcutaneous) in 65% of cases. Systemic corticosteroids were associated in 100% of cases. In the short term, 23 patients underwent spirometry, which allowed the initiation of a long-term treatment combining long-acting bronchodilator and inhaled corticosteroid. Thirty-one patients were treated with DMARD without interacted lung function assessment. In all cases, patients used a short-acting bronchodilator as needed.
Conclusion. The management of asthma still presents some shortcomings in the respiratory department of the University Hospital of Brazzaville both on the treatment of the crisis or exacerbation as in the background treatment.
KEYWORDS: Management, asthma, pulmonological environment, Brazzaville
RÉSUMÉ
Introduction et Objectif. L'asthme est une maladie inflammatoire chronique des bronches qui nécessite une codification de sa prise en charge par des pneumologues. En raison du manque de consensus sur les soins au niveau national, nous nous sommes permis d’évaluer les soins dispensés dans le service de pneumologie de l’hôpital universitaire de Brazzaville afin de mieux définir les axes de soins.
Méthodes. Nous avons analysé les enregistrements de données du service de crise ou d'exacerbation de l'asthme et des contrôles effectués au cours de l’étude.
Résultats. Au total, nous avons analysé la prise en charge de 54 patients au cours de cette période. Ils étaient 60% de femmes et 40% d'hommes, majoritairement jeunes, avec un âge moyen de 25,6 ans (extrême: 19 ans et 62 ans). Le pic de débit n’a pas été utilisé pour évaluer la gravité ou non de la crise. Les bronchodilatateurs en solution pour nébulisation ont été utilisés dans 35% des cas et les formes injectables (sous-cutanées) dans 65% des cas. Les corticostéroïdes systémiques étaient associés dans 100% des cas. À court terme, 23 patients ont subi une spirométrie, ce qui a permis d'initier un traitement à long terme associant un bronchodilatateur à longue durée d'action et un corticostéroïde inhalé. Trente et un patients ont été traités par DMARD sans évaluation de la fonction pulmonaire dans l’intervale. Dans tous les cas, les patients ont utilisé un bronchodilatateur à courte durée d'action selon les besoins.
Conclusion. La prise en charge de l'asthme présente encore des lacunes dans le service de pneumologie de l'hôpital universitaire de Brazzaville, tant sur le traitement de la crise que sur l'exacerbation, comme dans le traitement de fond.
MOTS CLÉS: Prise en charge, asthme, environnement pneumologique, Brazzaville.
INTRODUCTION
Asthma is a health problem throughout the world. Of the 300 million people affected by this disease, it is estimated that nearly 100 million will be added by 2025 [1].
Data remains fragmentary, especially in Africa, where few studies evaluate the quality of the care provided by general practitioners and specialists [2-4].
This is why the pulmonologists must be at the threshold of a paradigm shift taking into account all the innovations that are made in terms of care adapted by learned societies, with the absolute necessity to develop at the national level Supports adapted to asthmatic patients as shown by "4p" medicine: predictive, participatory, preventive and personalized that must emerge in chronic diseases such as asthma [5].
In Congo, despite the increase in its hospital frequency [6, 7], and the existence of a learned Congolese society, there is no consensus of care at the national level.
The chronic inflammatory nature of the bronchi in asthma requires a codification of its management. Also, its management adapted from the diagnosis makes it possible to obtain a lasting control, also prevents late complications related to remodeling thus resulting in a respiratory disability [8].
This study is part of a program to assess the attitude of the various key players, including pulmonologists, involved in the management of asthma to develop national guidelines.
Thus, to improve the management of asthma at the national level, we proposed to make an assessment in a department of pulmonology to better define the axes of care.
METHODS
The pulmonology department of the University Hospital of Brazzaville, a specialized management structure for respiratory pathology, served as the study framework.
It is structured in two sectors A and B and has six respiratory physicians, four of whom are new doctors and two doctors, they are take care of 25 beds.
Type of study
This was a retrospective, descriptive and analytical study of patients with asthma who were hospitalized for a crisis or exacerbation and followed-up in the respiratory department of the Brazzaville University Hospital.
Period of study
The study ran from January 1st 2015 to May 31th 2016, which lasted for 17 months.
Materials
We collected the records of all asthmatic patients who were admitted for asthma crisis or exacerbation and those who were followed in respiratory department during the study period.
Sampling
A large sample of 93 files was initially created and only 54 were selected taking into account the inclusion criteria.
Included folders
All records of asthmatic patients regardless of age and gender admitted for crisis or exacerbation during the study period. All records of asthmatic patients regardless of age and gender followed during the study period.
Non included folders
All incomplete folders that did not contain most of the scaning settings.
Studied variables
The data collection tool consisted of a pre-established survey sheet of patient records of asthmatic patients received during the study period.
The studied variables were socio-demographic and environmental parameters: age, sex, occupation, and level of study; Medical history: notion of atopy, ENT history, and smoking concept; The use of peak flow; The molecules (drugs) used in the treatment and their route of administration; The elements of the follow-up and the existence of a background treatment; The demand or not of spirometry; The result of the spirometry which was notified in the file.
In recent practice (5 years), the spirometer used wass the MiniSpir Light SN A23-K.00386 regularly calibrated without bronchodilator test. Its analysis taken into account the best of the three successive tests. It was also taking into account the degree of cooperation of the patient and the aspect of the flow/volume curve.
The measured parameters were forced vital capacity (FVC) in liters (L); forced expiratory volume in one second (FEV1) in liters per second (L); peak expiratory flow (PEF) in liters per second (L/s).
Their projected reference values were reported to the
African ethnic group.
The defined spirometric pathological profiles are as follows:
-The obstructive syndrome was defined as a normal
forced or forced vital capacity (FVC), a forced expiratory volume in one second (FEV1) below 80% of the theoretical value, and the FEV1/FVC coefficient less than 70%.
-The restrictive syndrome was defined by a lowering of the vital capacity (CV) and FEV1 with the normal FEV1/FVC coefficient.
The definition of small airways syndrome was based on a lowering of the median maximum expiratory flow (MEF), a reduction of the forced expiratory flow (FEF) rate to 75% and a minimum of 25% of the vital capacity (VC). The severity of the different syndromes was based on the value of FEV1.
The syndrome was either mild (FEV1>80%); moderate (50%<FEV1<80%); severe (30%<FEV1<50%); very severe (FEV1 <30%) [9].
Data analysis
The data were entered by Excel 2013 and analyzed by using the Epi info version 3.5.1 software.
The median and interquartile range were calculated for quantitative variables when the distribution was asymmetric; and the mean with the standard deviation was used when the distribution was symmetric. The Chi-square test was used for comparisons.
All tests were interpreted with a significance level of 5%.
RESULTS
The hospital frequency of asthma in the department of pulmonology was 10.22%. During the study period (17 months), 54 asthma patient records were eligible for evaluation.
Our patients were aged from 19 to 62 with an average age of 25.6 years.
Women were accounted for 60% of the workforce against 40% for men (32/22).
The majority of patients were young and for most women with a significant difference (P<0.01) and were in the 19-39 age group.
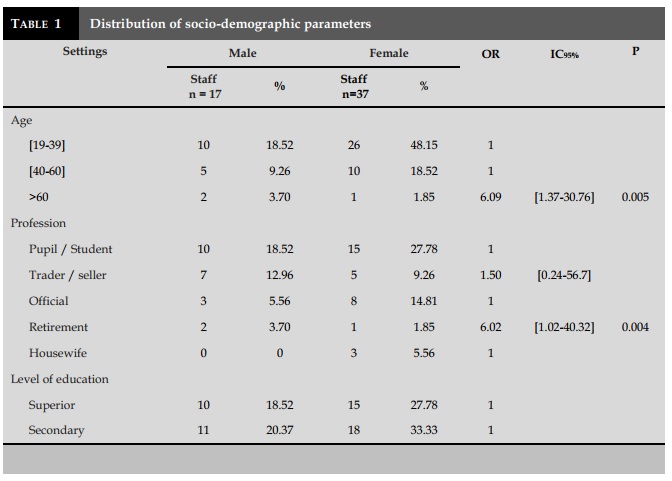
Students, civil servants, housewives and education at the expense of women were mostly concerned with a significant difference (P<0.01) (Table 1).
African ethnic group.
The defined spirometric pathological profiles are as follows:
-The obstructive syndrome was defined as a normal
forced or forced vital capacity (FVC), a forced expiratory volume in one second (FEV1) below 80% of the theoretical value, and the FEV1/FVC coefficient less than 70%.
-The restrictive syndrome was defined by a lowering of the vital capacity (CV) and FEV1 with the normal FEV1/FVC coefficient.
The definition of small airways syndrome was based on a lowering of the median maximum expiratory flow (MEF), a reduction of the forced expiratory flow (FEF) rate to 75% and a minimum of 25% of the vital capacity (VC). The severity of the different syndromes was based on the value of FEV1.
The syndrome was either mild (FEV1>80%); moderate (50%<FEV1<80%); severe (30%<FEV1<50%); very severe (FEV1 <30%) [9].
Data analysis
The data were entered by Excel 2013 and analyzed by using the Epi info version 3.5.1 software.
The median and interquartile range were calculated for quantitative variables when the distribution was asymmetric; and the mean with the standard deviation was used when the distribution was symmetric. The Chi-square test was used for comparisons.
All tests were interpreted with a significance level of 5%.
RESULTS
The hospital frequency of asthma in the department of pulmonology was 10.22%. During the study period (17 months), 54 asthma patient records were eligible for evaluation.
Our patients were aged from 19 to 62 with an average age of 25.6 years.
Women were accounted for 60% of the workforce against 40% for men (32/22).
The majority of patients were young and for most women with a significant difference (P<0.01) and were in the 19-39 age group.
Students, civil servants, housewives and education at the expense of women were mostly concerned with a significant difference (P<0.01) (Table 1).
Regarding the medical history and the concept of atopy were found in 34 cases/54 or 62.96%; ENT (ear-nose-throat) medical histories were dominated by sinusitis with 25 cases/54 or 46.30% and allergic rhinitis in 10 cases/54 or 18.52%.
Active smoking was found in 20 files/54 or 37.04%.
No peak-flow use was made to measure patients' peak expiratory flow in order to assess the severity or otherwise of their crisis or exacerbation during their admission to the service.
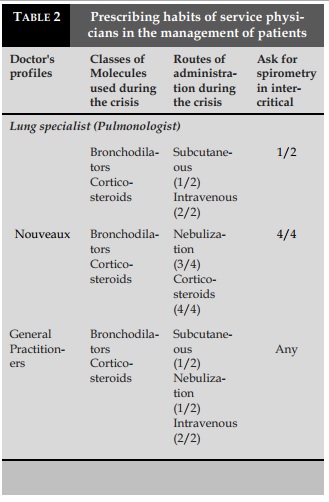
The prescribing habits taking into account the molecule (s) used, their routes of administration and the demand for spirometry in inter-critical manner are summarized in (Table 2).
Bronchodilators in solution for nebulization were used in 35% of cases and forms for injection (subcutaneous) in 65% of cases.
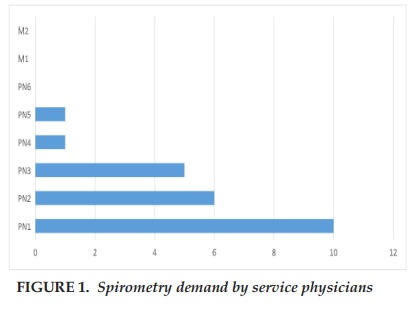
Figure 1 provides information on the demand for short-term spirometry by physicians (pulmono-logists and general practitioners).
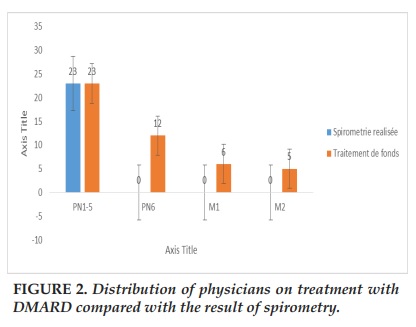
The DMARD included a long-acting bronchodilator and an inhaled corticosteroid (Figure 2).
DISCUSSION
This work has limitations related to the choice of a single center and taking into account only the pulmonologists mainly concentrated in a single service, thus limiting a global analysis of the management of asthma. But the fact that this work taken into account the therapeutic attitude according to the severity or the severity of the asthmatic disease as well as the evaluation of the intentions of treatment, one can thus have the absolute certainty that it is the exact reflection of what doctors (specialists and general practitioners) do in the field of pulmonology in practice.
The average young age of our patients reflects the initial work done in the service [6,7]. As much for the predominance of women, which is also found by other authors in the sub regions and in Europe [10-12]. Throughout life, the woman with asthma differs from the man, as the epidemiology, the evolution of the disease, sometimes punctuated by the events of the genital life such as puberty or menopause. These differences are often attributed to the sex hormones, without actually being able to formally attribute a protective or deleterious role as their biological effects are variable [12]. We found a statistically significant difference between age (19-60 years) and sex (P<0.001).
Forty-six point three percent (46.3%) of our patients were students, followed by 22.22% merchants and 20.37% of civil servants with level interference acceptable secondary school education with no statistically significant but statistically significant difference by sex (P<0.01). Kayantao et al in Mali in 2001 [10] found a similar result. This predominance in relation to the level of education could be explained by the fact that educated patients learn more about the disease and consult at the slightest sign in the specialized structures of care unlike those who would have a lower level.
The concept of atopy was found in 62.96% of cases. This result has been reported by several authors, both African and European [7,11,13]. This shows the genetic character of the disease. Thus, it is thought that the prevention of allergic asthma may be possible one day in atopic children and/or whose parents are atopic, by acting favorably on the immune system through new forms of specific immunotherapy or the use of pre or probiotics [13].
ENT medical histories were represented by sinusitis (46.30%) and allergic rhinitis (18.52%), which explains the multifactorial nature of asthma with their affinity to the respiratory sphere.
Active smoking was found in 37.04% of cases. Smoking causes chronic inflammation of the airways with predominantly neutrophils [14,15]. As it causes bronchial hyperreactivity and inflammation of allergic origin.
In our study, no use of peak flow was made to measure patients' peak expiratory flow while the positive diagnosis of asthma was based on the definition of asthma. The two characteristic elements are on the one hand clinical appreciating the chronicity of the disease, its variability and the reversible character of the symptoms and on the other hand functional appreciating the peak expiratory flow (PEF).
However, in an American study [16], the authors compared, in the context of national care programs, the treatments and fate of adult asthmatic patients according to their general practitioner physicians or pulmonologists. Thus, it was found that the possession of devices to measure peak expiratory flow was reported by 41.9% of patients of inexperienced GPs while they were 51.7% and 53.8% to own this device among patients of experienced general practitioners or specialists (pulmonologists or allergists), respectively. This is why the use of the peak flow must be integrated in the daily practice of the management of acute phases of asthmatic patients when they are admitted to a specialized respiratory care unit.
Concerning the prescribing habits of physicians (pulmonologists and general practitioners), it appears that the old pulmonologists, although they prescribe bronchodilators and corticosteroids during the acute phases, continue to opt for subcutaneous routes for bronchodilators and intravenous for corticosteroids then that the new ones opt for nebulization solutions for bronchodilators and injectable forms of corticosteroids.
There are some variability in the choice of molecules and their routes of administration for general practitioners. These therapeutic choices and their modes of administration join the strategies of management and prevention of the asthmatic disease [17]. Thus, these variabilities between pulmonologists and general practitioners are explained by the fact that the level of knowledge of the disease is not the same, and that learned societies of pulmonology adapting the recommendations for most diseases of their specialty [18].
The demand for inter critical spirometry is more in demand by new pulmonologists than by older and general practitioners. This is explained by the fact that the level of training or acquisition of the new recommendations is not in line with the old pulmonologists and general practitioners. Thus, the severity and control of asthma are evaluated in part by the age of bronchial obstruction and its variability. PEF and spirometry, which measure FEV1 and FEV1/FVC, are the reference measures in asthma. These measures, although equivalent in the GINA recommendations, are also equivalent to the recommendations of the Society of Pulmonology of French Language (SPLF) [18,19].
Background therapy is instituted overall with more correlation in pulmonologists with respect to spirometry data. The basic treatment of asthma, validated by international consensus meetings, is based on the use of inhaled anti-inflammatory drugs in the early stages of the disease [20]. It prevents mortality from acute asthma and the decline of respiratory function.
In the majority of cases, spirometry was normal compared to the abnormalities found (P <0.005). The obstructive syndrome was more found, thus explaining the obstructive bronchial character of the disease, although the evaluation of the obstruction was not taken into account in the evaluation elements. According to the recommendations, for indicative purposes, a rate of respiratory function monitoring according to the dose of inhaled corticosteroids and the level of control of asthma is allowed. In case of acceptable control, in patients receiving inhaled corticosteroid treatment in high doses, an evaluation
will be proposed every 3 months and at least every 6 months. In patients receiving inhaled corticosteroid therapy of medium or low dose, spirometry should be performed at best every 6 months and at least every year. In periods of unacceptable control, in patients who have used short-term oral corticosteroids, spirometry should be performed within one week after discontinuation of oral corticosteroid therapy and one month later. In the absence of oral corticosteroid therapy, spirometry should be performed within 1 to 3 months of the therapeutic modification [19].
CONCLUSION
This study constitutes a first evaluation in the prac-tice of the management of asthma in a Congolese specialized environment. It has identified some difficulties in implementing international recommendations on asthma management. This study also showed that the specialization as well as the experience of the treatment of asthma are associated with a better quality of care that can impact on a more favorable prognosis for asthmatic patients.
Therefore, all these difficulties should allow the Congolese aware the society about pulmonology to adopt a policy of implementation of a manual of management of asthma taking into account all relevant international innovations in the field adapted to the Congolese respiratory context.
CONFLIT OF INTEREST
The authors declare no conflit of interest for this work.
REFERENCES
1. Miaoli M, Fabian D, Holt S, et al. The global burden of asthme : executive summary of the GINA Disselination Committee report. Allergy 2004 ; 59 :469-478.
2. Koffi N, Kouassi B, Ngom K, Kone M S, Aka Danguy E. Evaluation of the management of adult asthma in Africa A national survey of Ivorian GPs. Rev Mal Respir 2001; 18 (5): 531-536.
3. Hounkpati A, Hounkpati H Y, Kpanla E, Balogou K A, Tidjani O. Assessment of the management of asthma in Africa. National survey of doctors and interns of Togo. Rev Mal Respir 2009; 26 (1): 11-20.
4. Ait-Khaled N, Odhiambo J, Pearce N, Adjoh KS, Maesano IA, Benhabyles B, Bouhayad Z, Bahati E, Camara L, Catteau C, El Sony A, Esamai FO, Hypolite IE, Melaku K, Musa OA, Ng’ang’a L, Onadeko BO, Saad O, Jerray M, Kayembe JM, Koffi NB, Khaldi F, Kuaban C, Voyi K, M’Boussa J, Sow O, Tidjani O, Zar HJ : Prevalence of symptoms of asthma, rhinitis and eczema in 13- to 14-year-old children in Africa: the international Study of Asthma and Allergies in Child Hood Phase III. Allergy 2007 ; 62 : 247-58.
5. Hood L, Friend SH. Prédictive, personnalisez, préventive, participatory(P4) cancer medicine.Nat Clin Oncol 2011 ; 8 :184-7
6. Mboussa j, Kaoudi E. Asthma of the adult in a tropical environment: its peculiarities in Brazzaville. Med. Black Afr. J. 1990; 37: 462-464.
7. Bemba Esthel, Kambourou J et al. Bronchial asthma of the adult at the department of pneumology of the CHU of Brazzaville. Rev Pneumol Trop 2014; 22: 3-10. 8. GINA guidelines(2018) www.ginaasthma.org .
9. Chung K F, Wenzel S E, Brozek J L, Bush A, Castro M, Sterk P J, et al. International ERS /ATS guidelines on définition, évaluation and treatement of severe asthma.Eur Respir J 2004 ; 43(2) :343-73
10. Hounkapti A,Glakar C A,Gbadamassi A G,Adjoh K S,Balogou K A,Tidjani O. Attitudes of private pharmacists in the management of asthma patients in lome.Int J Tuberc Lung Dis 2007 ;11 :344-349
11. Badoum G, Ouedraogo S M, Lankoande H et al. Knowledge, attitudes and practices of general practitioners on asthma in Ouagadougou. Mali Medical 2012; 27 (1): 10-13
12. Townsend E A, Miller V M, Prakash Y S.Sex differences and sex steroids in lung health and disease.Endocr Rev 2012 ; 33 :1-47.
13. Osbon D A, Sinn JK.Prebiotics in infants for prevention of allergy.Cochrane Data base Syst Rev 2013 ; 3 :CD006474. 14. Chalmers G W, Macleod K J, Thomson L, et al. Smoking and airway inflammation in patients with mild asthma.Chest 2001 ; 120 :1917-22.
15. Boulet LP, Lemiere C, Archambault F, et al.Smoking and asthma : clinical and radiologic features, lung function, and airway inflammation. Chest 2006 ; 129 :661-8.
16. Wu A, Hopkins J et al. Treatment of asthma in adults in the United States: experience prevails. Arch Intern Med 2001; 161 (21): 2554-60.
17. Global Initiative for Asthma (GINA).Global strategy for asthma management and prevention.N HLBI/ WHO workshop report. National institutes for Heath, National Heart, Lung and Blood Institute, january 1995.revision 2002.
18. Raherison C, Bourdin A, Bonniaud P, Deslée G, Garcia G, Leroyer C, et al. Updated guidelines(2015) for management and monitoring of adule and adolescent asthmatic patients (from 12 years and older) of the Société de Pneumologie de Langue Française (SPLF) (Full Length text).Rev Mal Respir 2016 ; 33(4) :279-325
19. Aubier M: Inhaled corticosteroids in asthma: when to start and how to stop it? Rev Pneumol Clin 1996; 52: 145-9.
20. Godard P, Chanez P, Siraudin L et coll. Costs of asthma are correlated with severity : a 1-yr prospective study. Eur Respir J 2002 ; 19 :61-67
FIGURES - TABLES
REFERENCES
1. Miaoli M, Fabian D, Holt S, et al. The global burden of asthme : executive summary of the GINA Disselination Committee report. Allergy 2004 ; 59 :469-478.
2. Koffi N, Kouassi B, Ngom K, Kone M S, Aka Danguy E. Evaluation of the management of adult asthma in Africa A national survey of Ivorian GPs. Rev Mal Respir 2001; 18 (5): 531-536.
3. Hounkpati A, Hounkpati H Y, Kpanla E, Balogou K A, Tidjani O. Assessment of the management of asthma in Africa. National survey of doctors and interns of Togo. Rev Mal Respir 2009; 26 (1): 11-20.
4. Ait-Khaled N, Odhiambo J, Pearce N, Adjoh KS, Maesano IA, Benhabyles B, Bouhayad Z, Bahati E, Camara L, Catteau C, El Sony A, Esamai FO, Hypolite IE, Melaku K, Musa OA, Ng’ang’a L, Onadeko BO, Saad O, Jerray M, Kayembe JM, Koffi NB, Khaldi F, Kuaban C, Voyi K, M’Boussa J, Sow O, Tidjani O, Zar HJ : Prevalence of symptoms of asthma, rhinitis and eczema in 13- to 14-year-old children in Africa: the international Study of Asthma and Allergies in Child Hood Phase III. Allergy 2007 ; 62 : 247-58.
5. Hood L, Friend SH. Prédictive, personnalisez, préventive, participatory(P4) cancer medicine.Nat Clin Oncol 2011 ; 8 :184-7
6. Mboussa j, Kaoudi E. Asthma of the adult in a tropical environment: its peculiarities in Brazzaville. Med. Black Afr. J. 1990; 37: 462-464.
7. Bemba Esthel, Kambourou J et al. Bronchial asthma of the adult at the department of pneumology of the CHU of Brazzaville. Rev Pneumol Trop 2014; 22: 3-10. 8. GINA guidelines(2018) www.ginaasthma.org .
9. Chung K F, Wenzel S E, Brozek J L, Bush A, Castro M, Sterk P J, et al. International ERS /ATS guidelines on définition, évaluation and treatement of severe asthma.Eur Respir J 2004 ; 43(2) :343-73
10. Hounkapti A,Glakar C A,Gbadamassi A G,Adjoh K S,Balogou K A,Tidjani O. Attitudes of private pharmacists in the management of asthma patients in lome.Int J Tuberc Lung Dis 2007 ;11 :344-349
11. Badoum G, Ouedraogo S M, Lankoande H et al. Knowledge, attitudes and practices of general practitioners on asthma in Ouagadougou. Mali Medical 2012; 27 (1): 10-13
12. Townsend E A, Miller V M, Prakash Y S.Sex differences and sex steroids in lung health and disease.Endocr Rev 2012 ; 33 :1-47.
13. Osbon D A, Sinn JK.Prebiotics in infants for prevention of allergy.Cochrane Data base Syst Rev 2013 ; 3 :CD006474. 14. Chalmers G W, Macleod K J, Thomson L, et al. Smoking and airway inflammation in patients with mild asthma.Chest 2001 ; 120 :1917-22.
15. Boulet LP, Lemiere C, Archambault F, et al.Smoking and asthma : clinical and radiologic features, lung function, and airway inflammation. Chest 2006 ; 129 :661-8.
16. Wu A, Hopkins J et al. Treatment of asthma in adults in the United States: experience prevails. Arch Intern Med 2001; 161 (21): 2554-60.
17. Global Initiative for Asthma (GINA).Global strategy for asthma management and prevention.N HLBI/ WHO workshop report. National institutes for Heath, National Heart, Lung and Blood Institute, january 1995.revision 2002.
18. Raherison C, Bourdin A, Bonniaud P, Deslée G, Garcia G, Leroyer C, et al. Updated guidelines(2015) for management and monitoring of adule and adolescent asthmatic patients (from 12 years and older) of the Société de Pneumologie de Langue Française (SPLF) (Full Length text).Rev Mal Respir 2016 ; 33(4) :279-325
19. Aubier M: Inhaled corticosteroids in asthma: when to start and how to stop it? Rev Pneumol Clin 1996; 52: 145-9.
20. Godard P, Chanez P, Siraudin L et coll. Costs of asthma are correlated with severity : a 1-yr prospective study. Eur Respir J 2002 ; 19 :61-67
ARTICLE INFO
DOI: 10.12699/jfvpulm.9.29.2018.19
Conflict of Interest
Non
Date of manuscript receiving
14/7/2018
Date of publication after correction
16/12/2018
Article citation
Okemba Okombi FH, Fiogbe Attanon A, Koumeka P, Bopaka GR, Ossale Abacka KB, Bemba ELP, Adjoh Komi S. Evaluation of the management of asthma in a specialized pulmonological environment at CHU Congo-Brazzaville. J Func Vent Pulm 2018;29(9):19-25