
 English
English
 French
French
Variations in Trans-Pulmonary Pressure During Two and One Lung Ventilation and Change of Patient's Position
Variations de la Pression Trans-Pulmonaire Pendant la Ventilation à Deux et un Poumons et Changement de Position
D. Braunold1, A. Lehavi1, B. Livshits1, M. Barak1,2
1 ; Department of Anesthesiology, Rambam Health Care Campus. Haifa, Israel
2 : Bruce and Ruth Rappaport Faculty of Medicine. Technion - Israel Institute of Technology. Haifa, Israel
Corresponding author
DR. MICHAL BARAK
Department of Anesthesiology, Rambam Health Care Campus. POB 9602, Haifa 31096 Israel
E-mail: m_barak@rambam.health.gov.il
ABSTRACT
Introduction. Esophageal manometry, using esophageal balloon catheter, allows estimation of the pleural pressure (PP). Trans-pulmonary pressure (TPP) is calculated by subtracting PP from airway pressure. TPP correlates with lung compliance. This technique is used to optimize ventilation in critical ill patients. We studied alterations in esophageal pressure (Pes) and airway pressure during two and one lung ventilation and changes of patient’s position in order to learn about TPP changes in such events.
Methods. This is a prospective longitudinal cohort study of 19 adult patients undergoing thoracoscopic surgery. Following induction of general anesthesia, an esophageal balloon device was used to measure Pes for the three phases of the respiratory cycle: peak inspiratory, plateau and end expiratory pressure. Airway pressure was recorded at the same time. We compared the pressures during ventilation of the two lungs, during one lung ventilation (OLV) in the supine position and finally in the lateral position.
Results. Trans-pulmonary pressure increased after changing from bilateral ventilation to OLV during each of the three stages of mechanical ventilation. Peak inspiration TPP increased from 10.4± 7.1 to 17.2± 5.8 cmH2O (P<0.0001). TPP during inspiratory plateau increased from 4.4± 5.6 to 11.8 ± 5.0 cmH2O (P<0.0001), and end expiratory TPP from -5.9±4.1 to 0.5±3.5 cmH2O (P<0.0001).
Conclusion. There was a significant increase in the TPP when switching from bilateral ventilation to OLV throughout the respiratory cycle. The clinical application of this finding is yet to be discovered.
KEYWORDS: Trans-pulmonary pressure; One lung ventilation; Video assisted thoracoscopic surgery; Esophageal balloon catheter.
RÉSUMÉ
Introduction. La manométrie oesophagienne, à l’aide d’un cathéter à ballonnet oesophagien, permet d’estimer la pression pleurale (PP). La pression trans-pulmonaire (PTP) est calculée en soustrayant la PP de la pression des voies respiratoires. La PTP est en corrélation avec la compliance pulmonaire. Cette technique est utilisée pour optimiser la ventilation chez les patients gravement malades. Nous avons étudié les modifications de la pression œsophagienne (Poe) et des voies respiratoires lors d’une ventilation à deux et un poumons ainsi que les modifications de la position du patient afin d’en apprendre davantage sur les modifications de la PTP lors de tels événements.
Méthodes. Il s'agit d'une étude de cohorte longitudinale prospective portant sur 19 patients adultes subissant une chirurgie thoracoscopique. Après l'induction de l'anesthésie générale, un ballon œsophagien a été utilisé pour mesurer la pesée pondérale pendant les trois phases du cycle respiratoire: pression inspiratoire maximale, plateau et pression expiratoire finale. La pression des voies aériennes a été enregistrée au même moment. Nous avons comparé les pressions lors de la ventilation des deux poumons, d'une ventilation d’un pumon (VUP) en décubitus dorsal et enfin en position latérale.
Résultats. La PTP a augmenté après le passage de la ventilation bilatérale à la VUP au cours de chacune des trois étapes de la ventilation mécanique. Le pic de PTP d'inspiration est passé de 10,4±7,1 à 17,2±5,8 cm H2O (P<0,0001). La PTP pendant le plateau inspiratoire a augmenté de 4,4±5,6 à 11,8±5,0 cm H2O (P<0,0001) et la PTP expiratoire de -5,9±4,1 à 0,5±3,5 cm H2O (P<0,0001).
Conclusion. Il y avait une augmentation significative de la PTP lors du passage d'une ventilation bilatérale à une VUP tout au long du cycle respiratoire. L'application clinique de cette découverte reste à découvrir.
MOTS CLÉS: pression trans-pulmonaire; une ventilation pulmonaire; chirurgie thoracoscopique assistée par vidéo; cathéter à ballon oesophagien.
INTRODUCTION
An esophageal balloon catheter is one of the techniques used to measure esophageal pressure (Pes), which closely correlates to the pleural pressure (Ppl) [1,2]. This can in turn be used to calculate the transpulmonary pressure (TPP), which is the difference between the airway pressure and the pleural pressure. Trans-pulmonary pressure is comparable to lung compliance, and is often used for optimizing ventilation in patients with acute respiratory distress syndrome (ARDS) [3], by adjusting positive end expiratory pressure (PEEP) to the patient's lung features and assessing lung recruitability [4]. Trials conducted in ARDS patients confirms the value of esophageal manometry in improving ventilation, which led to better clinical outcomes [5,6]. One-lung ventilation (OLV) is used in certain types of thoracic and thoracoscopic procedures. Postoperative acute lung injury (ALI) may occur in 415% of patients undergoing lung resection with OLV [7] and along with ARDS are the leading causes of post-operative mortality in these surgical patients [8,9]. Usually, the post-operative failing lung is the lung that is ventilated during the surgery, and not the operated one. This raise the question whether ventilation during the surgery cause the injury. In critically ill patients with lung injury, ventilating with low tidal volumes and low airway pressure is recommended. This technique, which is commonly referred to as “protective ventilation”, had been proven beneficial for bilateral lung ventilation. However, a debate still remains regarding the advantages of “protective ventilation” during OLV [10]. To the best of our knowledge, esophageal balloon devices have not been used in clinical setting as a guide to optimize ventilation during OLV. Furthermore, little published evidence exists about changes in TPP during OLV.
In the present trial, an esophageal balloon catheter is used to measure TPP in patients undergoing video assisted thorascopic surgery (VATS) of lung lobectomy. We examined the TPP and respiratory mechanics during tow lung ventilation, OLV and after positioning the patient to the lateral position. We assume that TPP would provide useful information to individualize the ventilator settings during OLV and optimize ventilation, thus reduce the risk for postoperative pulmonary complications.
METHODS
The study was approved by the institutional review board, and registered (Clinical Trials Registry, reference NCT03567759). This study was performed in a prospective, longitudinal cohort manner. Adult patients scheduled for elective VATS lobectomy were included in the study. All patients signed an informed consent. Exclusion criteria included patients with esophageal pathology or surgery, previous lung or chest wall resection, and difficulty in placing the esophageal catheter. Following induction of general anesthesia using fentanyl 2-5 microgram/kg; propofol 1-3 mg/kg and rocuronium 0.6-0.8 mg/kg the trachea was intubated with a left double lumen tracheal tube VivaSight (ETView Ltd. Misgav Business Park, Israel) where verification of the tube position was monitored continuously with on-line video surveillance. Mechanical ventilation in a volume controlled mode with tidal volumes of 8ml/kg and PEEP 5cm H2O was initiated with respiratory rate of 10-13 breaths per minute.
Esophageal Manometry
An esophageal balloon device (Adult Esophageal Balloon Catheter Set, Cooper Surgical, USA) [11] was placed according to the manufacturer’s instructions, as follows: The stomach was decompressed and suctioned using an 18 F orogastric tube which was also utilized to estimate the depth of the lower esophageal sphincter, a measure that was corroborated with external simulation of the approximate distance from the gastric opening to the nares. A lubricated 86 cm long closed-tip catheter with a 9.5 cm long balloon catheter at its distal end was gently inserted via one nostril and advanced into the esophagus. The balloon was placed at the lower third of the thoracic cavity at about 10 cm above the lower esophageal sphincter, as guided by catheter markings. This depth was calculated as the product of patient height x 0.288, and verified by the external measurements at described above. An extension tubing was attached to the Y piece at the proximal ending of the catheter and connected to a syringe and a pre-calibrated pressure transducer via a 3-way stopcock. One ml of air was injected into the balloon so that it became semi inflated, and the tracing on the pressure monitor was adjusted with additional small amounts of air until no flattening or damping was noted in the pressure waveform. When properly positioned, the catheter was secured with tape to prevent movement while placing the patient on lateral position. Esophageal pressure was continuously measured using a calibrated pressure transducer system (Art-Line, BioMetrix, Kiryat Mada, Jerusalem, Israel) connected to a patient monitor (Datex AS/3, Datex Ohmeda Medical Equipment, GE Healthcare, USA) and recorded using designated computer software.
Measurements
Airway pressures were recorded for the three phases of the respiratory cycle: peak inspiratory pressure (PIP); plateau pressure (Plat) and end expiratory pressure. Esophageal pressure was measured at the same time points.
After recording baseline pressures during bilateral lung ventilation (BLV), the patient was switched to OLV in the supine position and after 2 minutes of equilibration the pressures were recorded. During the change from BLV to OLV in the supine position tidal volumes were reduced from 8 ml/kg to 4 ml/ kg and the respiratory rate was increase as needed, keeping end tidal CO2 below 50 mmHg. PEEP was kept on 5 cm H2O. Than the patient was placed in the lateral position and after 2 minutes the pressures were recorded again. All measurements were recorded before the surgical procedure began. Transpulmonary pressure was calculated by subtracting Pes from airway pressure.
Statistical analysis
Descriptive statistics in terms of mean, STD, median, percentiles and ranges were performed to the whole parameters in the data. Repeated measure analysis with Bonferroni adjustment was applied for differences between the three measurements. P<0.05 was consider as significant.
RESULTS
Nineteen patients were recruited as participants, all of whom successfully completed the study. Participant’s demographics are shown in Table 1.
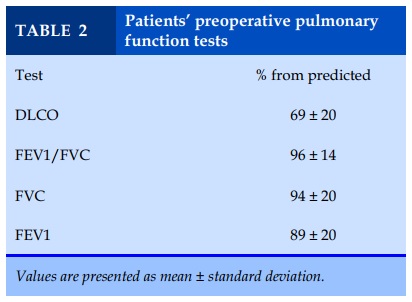
Pre-operative pulmonary function tests of all the patients were within normal limits (Table 2).
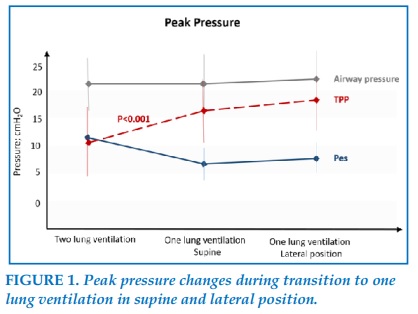
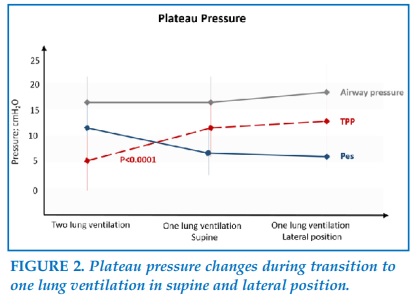
Trans-pulmonary pressures were calculated and found to be significantly higher when changing from BLV to either OLV in the supine or the lateral position but did not show any statistical significance when changing from OLV supine to lateral. These changes were consistent during all phases of the respiratory cycle. During peak inspiration, TPP increased significantly from 10.3± 7.1 cmH2O in supine BLV to 16.4± 6.4 cmH2O in supine OLV (P<0.0001) and then increased insignificantly to 17.2± 5.8 cmH2O in lateral OLV. During inspiratory plateau TPP increased from 4.4± 5.6 cmH2O to 10.5± 5.0 cmH2O (P<0.0001) and then increased insignificantly to 11.8 ± 5.0 cmH2O.
During end expirium TPP increased from -5.9±4.1 cmH2O to 0.5±3.5 cmH2O (P<0.0001). Peak and plateau airway pressure changes showed no significant difference when changing from BLT to OLV or when changing position P=0.55. Esophageal pressure showed significant difference when changing from BLT to OLV P<0.0001. Figures 1 and 2 display the changes of the airway pressure, esophageal pressure and trans-pulmonary pressure as ventilation altered from bilateral to one lung ventilation followed by a changes in patient position. The graphs clearly depict a step-wise increase in trans-pulmonary pressure throughout these stages. It can be seen that there is a little change in airway pressure, and the major component contributing to the change in the TPP is a decrease in esophageal pressure.
DISCUSSION
We demonstrated that TPP significantly increased when the ventilation was altered from supine bilateral ventilation to OLV in the lateral position. Transpulmonary pressures increased during inspiration, both peak and plateau. As shown in this study, airway pressure changed insignificantly despite substantial manipulation of the ventilation and patient positioning, whereas Pes significantly changed. This highlights that lung compliance may be changing significantly without the clinician being able to monitor it, as airway pressure stayed almost constant. We believe that by using esophageal manometry during OLV before the beginning of the surgery, the anesthesiologist may optimize mechanical ventilation parameters for the patient. This is more important in patients with significant lung disease, as implied from pre-operative poor pulmonary function tests. While improving intra-operative ventilation we seek to reduce post-operative pulmonary complications.
Ventilating the patient during OLV is complex. Previous studies demonstrated that excessive endinspiratory lung volumes increased extravascular lung water and diffuse alveolar damage [12], and was associated with ALI [13]. Also, high ventilating pressures during OLV are detrimental, increasing the risk for ALI [14]. On the other hand, when using low volume and low pressure ventilation, it is difficult to avoid atelectasis, hypercapnia and hypoxia. This becomes critical during OLV when the patient is already at risk for all these hazards to begin with [15].
Another issue is the optimal PEEP to provide during OLV. An early study showed that providing 10cmH2O PEEP to the dependent lung with a PAO2 < 80mmHg showed improvement, but if was PAO2 was > 80mmHg, providing PEEP of 10cm H2O did not improve PAO2 [16]. Application of inappropriately high PEEP may increase pulmonary vascular resistance and shift blood to the non-dependent lung, worsening shunt [17,18]. Hoffman et al found that providing high PEEP during OLV gave an unpredictable impact on oxygenation with an unchanged cardiac output [19]. Further studies into treating hypoxia with PEEP during OLV divided recipients into two groups with one providing low tidal volumes
With high PEEP vs high tidal volumes and low PEEP. Results indicated that the former group experienced lower oxygenation [20].
One limitation for the use of the balloon device for measuring OLV is that once pneumothorax has been achieved, the pressure on that side of the thorax falls to 1atm and the Pes falls to 0 mmHg compared to the surrounding environment. This makes continuous monitoring of Pes throughout a VATS procedure impossible. This study may provide some help in adjusting ventilation to the high risk patient during OLV before the beginning of the surgery.
Therefore, after intubation and before incision, ventilation mechanics can be manipulated with the use of the Pes to achieve a stable TPP so that surgery can occur with minimal lung injury, and hopefully to reduce the risk of post-operative pulmonary morbidity and mortality.
Another limitation is that calculating TPP requires adopting Pes as pleural pressure. This might be accurate in the upright position but, in the supine position, the mediastinum itself will add additional pressure to the Pes [21]. Also, the esophageal balloon device measures pressure within a pliable structure that moves easily within the mediastinum. Thus, when ventilation is changed from BLV to OLV, one side of the chest is exerting less force upon the esophagus, and the esophagus will drift toward the non-dependent lung. In this situation there are two pleural pressures, one for the dependent lung and one for the non-dependent lung.
The data being read from the esophageal balloon device will give an interpretation of both these pressures together but no true value to either side. In addition, we assume that there was no change in the esophageal catheter position, nor did the pressure in the balloon. Although this may have happened, changing the consistency of the results [22].
CONCLUSION
There is a significant increase in the TPP when switching from bilateral ventilation to OLV, while airway pressure changed insignificantly. This suggests that by measuring esophageal pressures one may have more accurate estimation of lung compliance and may be able to improve ventilation. Further studies are needed to concur in order to find whether this monitoring can be used to adjust ventilation in high-risk patients with compromised respiratory mechanics for surgery requiring one lung ventilation.
Acknowledgements
The authors thank Mrs. M. Perlmutter for her assistance in preparing this manuscript. This study was not supported by any funding.
CONFLICT OF INTEREST
All author declares that they have no conflict of interest to disclose.
REFERENCES
1. Milic-Emili J, Mead J, Turner JM., Glauser EM. Improved technique for estimating pleural pressure from esophageal balloons. J Appl Physiol 1964:19: 207 -11.
2. Gattinoni L, Chiumello D, Carlesso E, Valenza F. Bench-to-bedside review: chest wall elastance in acute lung injury/acute respiratory distress syndrome patients. Crit Care 2004; 8: 350-5.
3. Akoumianaki E, Maggiore SM, Valenza F, et al. The application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med 2014:189; 520-31.
4. Brower RG, Matthay MA, Morris A, et al; Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000:342;1301-8.
5. Talmor D, Sarge T, Malhotra A, O'Donnell CR, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med 2008;359:2095104. doi: 10.1056/NEJMoa0708638.
6. Fish E, Novack V, Banner-Goodspeed VM, et al. The Esophageal Pressure-Guided Ventilation 2 (EPVent2) trial protocol: a multicentre, randomised clinical trial of mechanical ventilation guided by transpulmonary pressure. BMJ Open 2014;4:e006356. doi: 10.1136/ bmjopen-2014-006356.
7. Licker MJ, Widikker I, Robert J, et al. Operative mortality and respiratory complications after lung resection for cancer: impact of chronic obstructive pulmonary disease and time trends. Ann Thorac Surg 2006;81:1830-7.
8. Licker M, Fauconnet P, Villiger Y, Tschopp JM. Acute lung injury and outcomes after thoracic surgery. Curr Opin Anaesthesiol 2009;22:61-67. doi: 10.1097/ ACO.0b013e32831b466c.
9. Iglesias M, Martinez E, Badia JR, Macchiarini P. Extrapulmonary ventilation for unresponsive severe acute respiratory distress syndrome after pulmonary resection. Ann Thorac Surg 2008;85:237-44.
10. Hedenstierna G, Edmark L, Perchiazzi G. Postoperative lung complications: have multicentre studies been of any help. Br J Anaesth 2015;114:541-3. doi: 10.1093/bja/aeu343.
11. CooperSurgical CDT, CT 06611 USA. 47-9005 • Adult Esophageal Balloon Catheter Directions for Use (English). 2014.
12. Kuzkov VV, Suborov EV, Kirov MY, et al. Extravascular lung water after pneumonectomy and one-lung ventilation in sheep. Crit Care Med 2007;35:1550-9.
13. Jeon K, Yoon JW, Suh GY, et al. Risk factors for postpneumonectomy acute lung injury/acute respiratory distress syndrome in primary lung cancer patients. Anaesth Intensive Care 2009;37:14-9.
14. Van der Werff YD, van der Houwen HK, Heijmans PJ, et al. Postpneumonectomy pulmonary edema. A retrospective analysis of incidence and possible risk factors. Chest 1997;111:1278-84.
15. Duggan M, Kavanagh BP. Atelectasis in the perioperative patient. Curr Opin Anaesthesiol 2007;20:3742.
16. Cohen E, Eisenkraft JB. Positive end-expiratory pressure during one-lung ventilation improves oxygenation in patients with low arterial oxygen tensions. J Cardiothorac Vasc Anesth 1996;10:578-82.
17. Choi YS, Bae MK, Kim SH, Park JE, Kim SY, Oh YJ. Effects of alveolar recruitment and positive endexpiratory pressure on oxygenation during one-lung ventilation in the supine position. Yonsei Med J 2015;56:1421-7. doi: 10.3349/ymj.2015.56.5.1421.
18. Inomata S, Nishikawa T, Saito S, Kihara S. ”Best” PEEP during one-lung ventilation. Br J Anaesth 1997;78:754-6.
19. Hoftman N, Canales C, Leduc M, Mahajan A. Positive end expiratory pressure during one-lung ventilation: selecting ideal patients and ventilator settings with the aim of improving arterial oxygenation. Ann Card Anaesth 2011;14:183-7. doi: 10.4103/09719784.83991.
20. Rozé H, Lafargue M, Perez P, et al. Reducing tidal volume and increasing positive end-expiratory pressure with constant plateau pressure during one-lung ventilation: effect on oxygenation. Br J Anaesth 2012;108:1022-7. doi: 10.1093/bja/aes090.
21. Pecchiari M, Loring SH, D'Angelo E. Esophageal pressure as an estimate of average pleural pressure with lung or chest distortion in rats. Respir Physiol Neurobiol 2013;186:229-35. doi: 10.1016/ j.resp.2013.02.006.
22. Mojoli F, Chiumello D, Pozzi M, et al. Esophageal pressure measurements under different conditions of intrathoracic pressure. An in vitro study of second generation balloon catheters. Minerva Anestesiol 2015; 81: 855-64.
FIGURES - TABLES

REFERENCES
1. Milic-Emili J, Mead J, Turner JM., Glauser EM. Improved technique for estimating pleural pressure from esophageal balloons. J Appl Physiol 1964:19: 207 -11.
2. Gattinoni L, Chiumello D, Carlesso E, Valenza F. Bench-to-bedside review: chest wall elastance in acute lung injury/acute respiratory distress syndrome patients. Crit Care 2004; 8: 350-5.
3. Akoumianaki E, Maggiore SM, Valenza F, et al. The application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med 2014:189; 520-31.
4. Brower RG, Matthay MA, Morris A, et al; Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000:342;1301-8.
5. Talmor D, Sarge T, Malhotra A, O'Donnell CR, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med 2008;359:2095104. doi: 10.1056/NEJMoa0708638.
6. Fish E, Novack V, Banner-Goodspeed VM, et al. The Esophageal Pressure-Guided Ventilation 2 (EPVent2) trial protocol: a multicentre, randomised clinical trial of mechanical ventilation guided by transpulmonary pressure. BMJ Open 2014;4:e006356. doi: 10.1136/ bmjopen-2014-006356.
7. Licker MJ, Widikker I, Robert J, et al. Operative mortality and respiratory complications after lung resection for cancer: impact of chronic obstructive pulmonary disease and time trends. Ann Thorac Surg 2006;81:1830-7.
8. Licker M, Fauconnet P, Villiger Y, Tschopp JM. Acute lung injury and outcomes after thoracic surgery. Curr Opin Anaesthesiol 2009;22:61-67. doi: 10.1097/ ACO.0b013e32831b466c.
9. Iglesias M, Martinez E, Badia JR, Macchiarini P. Extrapulmonary ventilation for unresponsive severe acute respiratory distress syndrome after pulmonary resection. Ann Thorac Surg 2008;85:237-44.
10. Hedenstierna G, Edmark L, Perchiazzi G. Postoperative lung complications: have multicentre studies been of any help. Br J Anaesth 2015;114:541-3. doi: 10.1093/bja/aeu343.
11. CooperSurgical CDT, CT 06611 USA. 47-9005 • Adult Esophageal Balloon Catheter Directions for Use (English). 2014.
12. Kuzkov VV, Suborov EV, Kirov MY, et al. Extravascular lung water after pneumonectomy and one-lung ventilation in sheep. Crit Care Med 2007;35:1550-9.
13. Jeon K, Yoon JW, Suh GY, et al. Risk factors for postpneumonectomy acute lung injury/acute respiratory distress syndrome in primary lung cancer patients. Anaesth Intensive Care 2009;37:14-9.
14. Van der Werff YD, van der Houwen HK, Heijmans PJ, et al. Postpneumonectomy pulmonary edema. A retrospective analysis of incidence and possible risk factors. Chest 1997;111:1278-84.
15. Duggan M, Kavanagh BP. Atelectasis in the perioperative patient. Curr Opin Anaesthesiol 2007;20:3742.
16. Cohen E, Eisenkraft JB. Positive end-expiratory pressure during one-lung ventilation improves oxygenation in patients with low arterial oxygen tensions. J Cardiothorac Vasc Anesth 1996;10:578-82.
17. Choi YS, Bae MK, Kim SH, Park JE, Kim SY, Oh YJ. Effects of alveolar recruitment and positive endexpiratory pressure on oxygenation during one-lung ventilation in the supine position. Yonsei Med J 2015;56:1421-7. doi: 10.3349/ymj.2015.56.5.1421.
18. Inomata S, Nishikawa T, Saito S, Kihara S. ”Best” PEEP during one-lung ventilation. Br J Anaesth 1997;78:754-6.
19. Hoftman N, Canales C, Leduc M, Mahajan A. Positive end expiratory pressure during one-lung ventilation: selecting ideal patients and ventilator settings with the aim of improving arterial oxygenation. Ann Card Anaesth 2011;14:183-7. doi: 10.4103/09719784.83991.
20. Rozé H, Lafargue M, Perez P, et al. Reducing tidal volume and increasing positive end-expiratory pressure with constant plateau pressure during one-lung ventilation: effect on oxygenation. Br J Anaesth 2012;108:1022-7. doi: 10.1093/bja/aes090.
21. Pecchiari M, Loring SH, D'Angelo E. Esophageal pressure as an estimate of average pleural pressure with lung or chest distortion in rats. Respir Physiol Neurobiol 2013;186:229-35. doi: 10.1016/ j.resp.2013.02.006.
22. Mojoli F, Chiumello D, Pozzi M, et al. Esophageal pressure measurements under different conditions of intrathoracic pressure. An in vitro study of second generation balloon catheters. Minerva Anestesiol 2015; 81: 855-64.
ARTICLE INFO
DOI: 10.12699/jfvpulm.10.30.2019.18
Conflict of Interest
Non
Date of manuscript receiving
10/01/2019
Date of publication after correction
15/3/2019
Article citation
Braunold D, Lehavi A, Livshits B, Barak M. Variations in Trans-Pulmonary Pressure During Two and One Lung Ventilation and Change of Patient's Position. J Func Vent Pulm 2019;30(10):18-22