
 English
English
 French
French
Study on pleural complications, techniques, and results of early gastrectomy plus lymphadenectomy D2 by endoscopic surgery in Thanh Nhan hospital
Étude des complications pleurales, des techniques et résultats d'une gastrectomie précoce associée d'une lymphadénectomie D2 par chirurgie endoscopique à l'hôpital de Thanh Nhan
M. Dao Quang
Thanh Nhan Hospital. Hanoi, Vietnam
Corresponding author
Dr. DAO QUANG Minh
Thanh Nhan Hospital. Hanoi - Vietnam
E-mail: prof.minhdao@gmail.com
DOI: 10.12699/jfvpulm.10.30.2019.1
ABSTRACT
Introduction. Researching on pleural complications, techniques, and evaluating the results of early gastrectomy plus lymphadenectomy D2 by endoscopic surgery in the treatment of gastric cancer at Thanh Nhan Hospital.
Methods. Retrospective and cross-sectional description.
Results. Twenty patients diagnosed with gastric cancer (endoscopic biopsy), gastrectomy, lymphadenectomy D2 by laparoscopic surgery at Thanh Nhan Hospital from 9/2016 to 6/2017. The patients are in the average age of 52.36 years (34 - 74 years), male / female ratio of 1.5/1. The common location of tumours is often in small curvature (BCN) 55%. Rate of successful laparoscopic surgery is 85%. Phase II is the most common (40%); Metastatic carcinoma (70%); Poor degree of differentiation (55%). The average time of an operation is 190 minutes (150 - 260 minutes); Blood loss of 97.20 ml (75–130 ml); the number of lymph nodes scraped is in the average of 35.70 nodes. The rate of accidents (10%), no patients died. Pleural effusion was 5%. All patients had little pain, early movement and duration of staying in the hospital about 11.20 ± 2.1 days.
Conclusion. Gastrectomy and lymphadenectomy D2 by laparoscopic surgery in the treatment of gastric cancer shows the initial positive results and the guarantee of cancinology. Pleural effusion is a unfrequented complication.
KEYWORDS: Pleural complications; Gastrectomy; Lymphadenectomy; Endoscopic surgery.
RÉSUMÉ
Introduction. Recherche sur les complications pleurales, les techniques et l’évaluation des résultats de la gastrectomie précoce, de la lymphadénectomie D2 par chirurgie endoscopique dans le traitement du cancer gastrique à l’hôpital Thanh Nhan.
Méthodes. Description rétrospective et transversale.
Résultats. 20 patients diagnostiqués avec un cancer gastrique (biopsie endoscopique), une gastrectomie, une lymphadénectomie D2 par chirurgie laparoscopique à l'hôpital Thanh Nhan du 9 au 6/2017. Les patients ont un âge moyen de 52,36 ans (34 - 74 ans) et un ratio hommes / femmes de 1,5 / 1. Les tumeurs ont souvent une courbure réduite (BCN) à 55%. Le taux de chirurgie laparoscopique réussie est de 85%. La phase II est la plus courante (40%); Carcinome métastatique (70%); Mauvais degré de différenciation (55%). La durée moyenne d'une opération est de 190 minutes (150 - 260 minutes); Perte de sang de 97,20 ml (75-130 ml); le nombre de ganglions lymphatiques raclés est dans la moyenne de 35,70 ganglions. Le taux d'accidents (10%), aucun patient n'est décédé. L’épanchement pleural est de 5%. Tous les patients présentaient peu de douleur, des mouvements rapides et une durée de séjour à l'hôpital d'environ 11,20 ± 2,1 jours.
Conclusion. La gastrectomie et la lymphadénectomie D2 par chirurgie laparoscopique dans le traitement du cancer gastrique montre les premiers résultats positifs et la garantie de la cancinologie. L’épanchement pleural est non fréquent.
MOTS CLÉS: Complications pleurales; Gastrectomie; Lymphdénectomie; Chirurgie endoscopique.
INTRODUCTION
Gastric cancer is one of the most common cancers in the world, considered the first- leading causes of death after lung cancer [4,5]. The distribution of this pathology is not equal across different geographical areas. This disease is more common in countries such as Japan, China, Southeast Asia, Latin America; moderate levels in European countries and low in countries such as India, USA, Australia.
Vietnam has the second rate of stomach cancer after lung cancer in men and the third after breast cancer and Cervical cancer in women [2,3].
Surgery is mainly used in treatment of gastric cancer. Depending on the location of the tumor, there will be indications of full or partial gastrectomy. Other methods such as chemicals, radiation and immunity play auxiliary roles [3].
After successful laparoscopic surgeries for patients with early gastric cancer performed by Kitano S. in 1991, laparoscopic surgery was quickly developed in Japan and Asian countries. More and more surgeons choose gastrectomy through endoscopy because of its superiority such as early recovery, less pain, short time of staying in hospital. However, endoscopic gastrectomy still has many discussion about the ability of lymphadenectomy, small abdominal incision to bring specimens/ medical waste (bệnh phẩm )out and performing suturing.
In 2003, Department of Gastroenterology - Viet Duc Hospital and Department of Surgery - Hospital of Medicine University of Ho Chi Minh City were the first two surgical centers that performed gastrectomy with endoscopic surgery. Currently, endoscopic surgery is performed in a number of major hospitals such as Hanoi, Ho Chi Minh City, Hue ... [6].
In Thanh Nhan Hospital, we have implemented this technique since September 2015, but we have not had any evaluation reports yet. So we do this research to:
• Research on gastrectomy, lymphadenectomy D2 by endoscopic surgery at Thanh Nhan Hospital.
• Evaluating the result of early endoscopic surgery in treatment of gastric cancer at Thanh Nhan Hospital.
METHODS
Subjects
Twenty patients diagnosed with gastric cancer (endoscopic biopsy) gastrectomy, lymphadenectomy D2 with endoscopic surgery at Thanh Nhan Hospital from September 2016 to June 2017.
Methods
Research methods: retrospective, cross-sectional description. Medical equipment, patient’s postures, position of surgeons and assistants: we often use scope 30º with other supportive endoscopic devices such as: liver discard, endostapler, ultrasonic scalpel or ligasure scalpel. The patient was lying on his back, his legs were straight and spread about 20º, the surgeon stood on the right of the patient, the first assistant was standing opposite to the surgeon, the second assistant holding the camera stood side by side with the surgeon.
Surgical technique
Step 1: Put the trocart into the abdomen.
Step 2: Observe and assess injury.
Step 3: Take the entire large mesenteric along the transverse colon from the right until near the spleen, constrict the artery (arterial) connected to the right position of the branch of duodenum and right junction immediately Henler's body in front of the pancreas to get ganglion group (4, 6) in the entire stomach cut, (4sb, 4d, 6) in the partial gastric section.
Step 4: Lymphadenectomy in the hepatic stalks, along the hepatic artery, ligation of the gastric arteries must take root to get ganglion group 5, 8a, 12a to take the entire small caul.
Step 5: Tightening left vein at the root, Lymphadenectomy (around visceral arteries) (ganglion group 7, 9, 11P) with gastric partial resection, (ganglion group 7, 9p, 11d) with the whole gastric surgery.
Step 6: Lymphadenectomy (1, 3) with partial gastric resection and (1, 2, 3) with entire gastric resection.
Step 7: Laparotomy with a small hole near the navel to pull the stomach out. Step 8: Gastrectomy and repeat the gastrointestinal circulation Billroth II - Finsterer cut half stomach, Roux en - Y cut the entire stomach.
Step 9: Set drainage, clean and close the abdomen.
RESULT
Age of patients
The youngest age is 34 years, the oldest is 74 years, the average age is 52.36 ± 8.50
Clinical and endoscopy symptoms
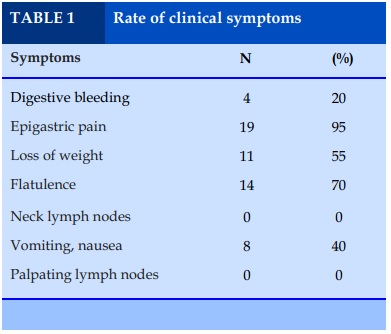
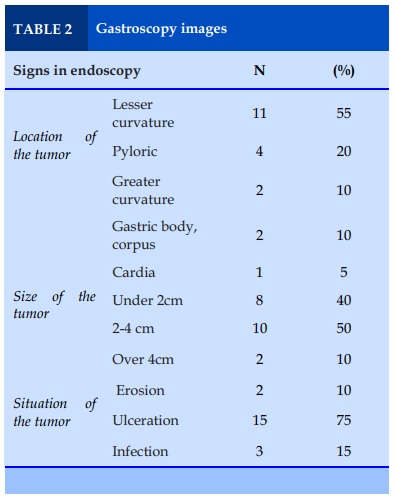
The most common symptoms are epigastric pain (95%), flatulence (70%). We have no cases of palpating the tumor itself and having lymph nodes in neck. The most common location of tumors is in small curvatures (55%). There is one case (5%) in which the tumor is in cardia. The size of tumor is usually less than 4cm (90%).
Evaluation during and after surgery
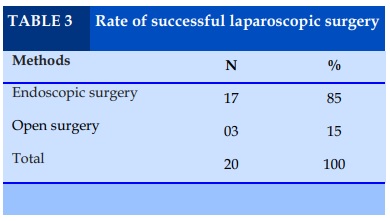
85% of patients were operated successfully with the technique of endoscopic surgery. 15% of patients were operated normally (open surgery). Table 1, 2, 3
Methods of surgery and lymphadenectomy
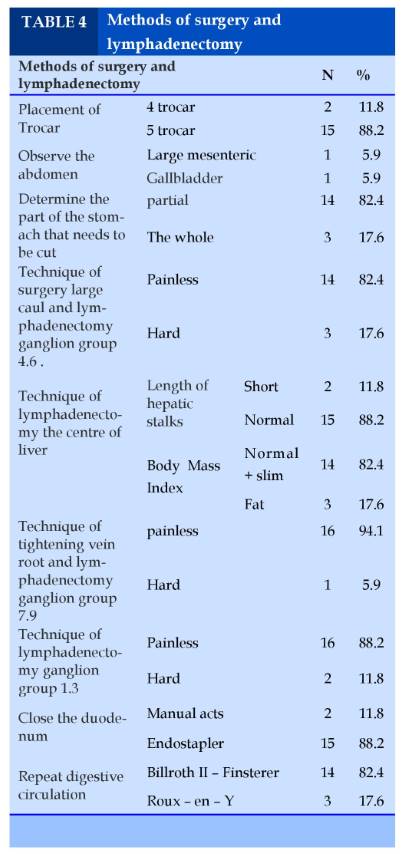
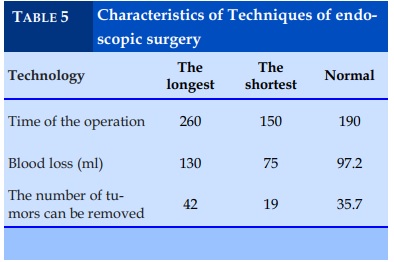
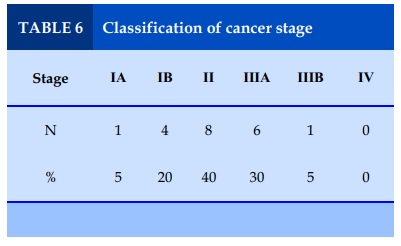
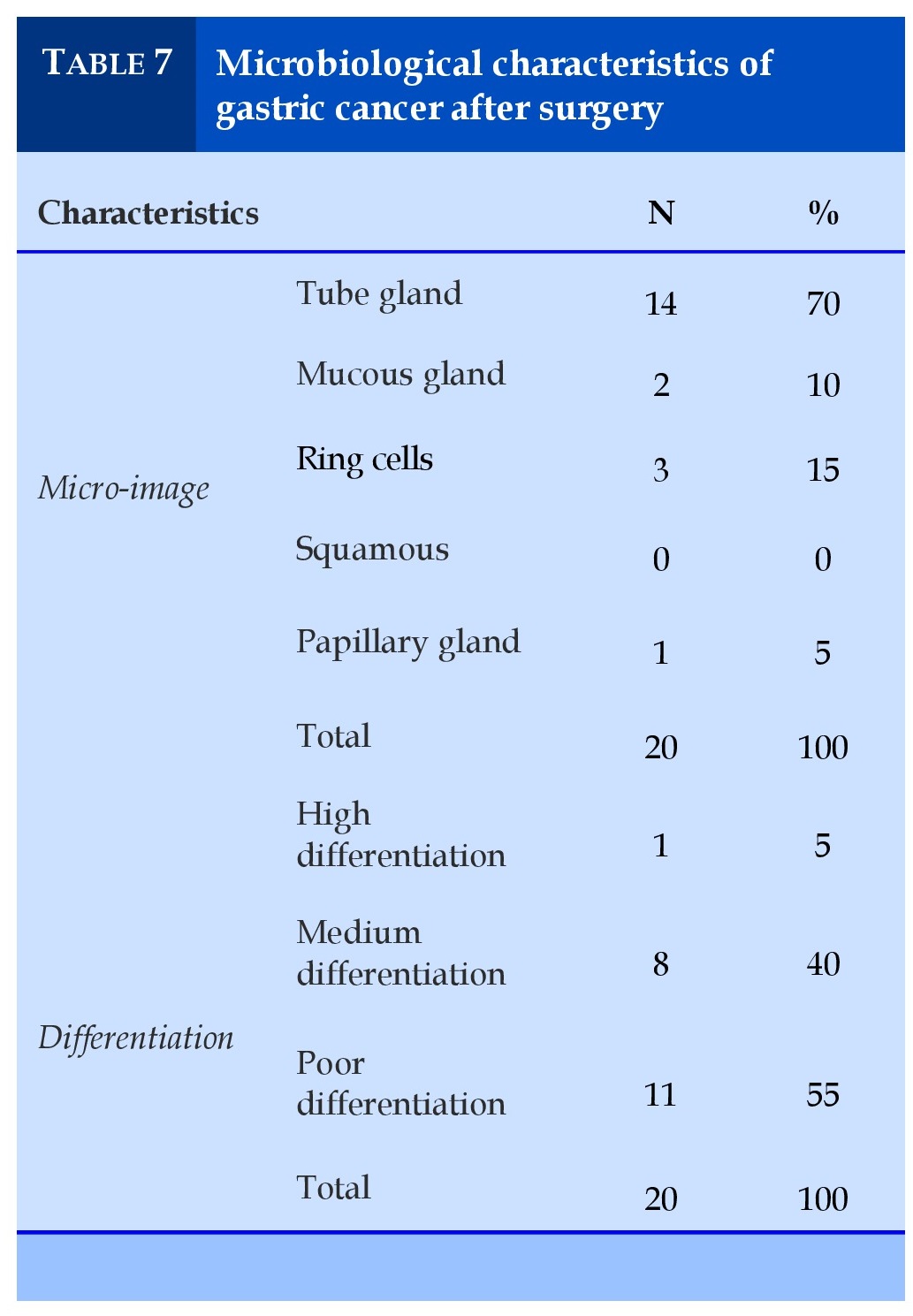
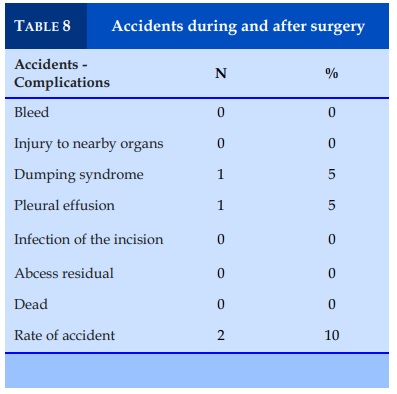
Postoperative monitoring showed an average time to fart is 3.6 ± 0.9 days. The patient was able to move around 4.2 ± 1.2. Time for postoperative analgesia: 3.9 ± 1.1. Time to stay in hospital: 11.2 ± 2.1. (Table 4, 5, 6, 7, 8, 9 , 10)
The size of the abdominal incision which gives support taking the stomach out to perform the reestablishment of circulation according to Billroth II - Finsterer in partial cutting and Roux - en - Y in the whole gastric cut is 5.2 cm in average and 6 cm in the largest.
The research on cancer detection in IB stage (20%), II (40%), IIIA (30%). We have no cases in Phase IV. The most common study that we often have is metastatic carcinoma (70%), and the low differentiation (55%).
DISCUSSION
In 1991, Kitano S. successfully performed endoscopic gastrectomy for patients with early gastric cancer, then this technique has been developed all over the world [14]. However, it is controversial when endoscopic surgery is performed to lymphadenectomy in stead of open surgery (widely accepted worldwide).
Studies in Japan have shown that endoscopic surgery can be performed safety and assurance in the treatment of early gastric cancer [12,13]. Early results of these studies showed the benefits of endoscopic surgery such as patients will recover quickly and have less pain and less blood loss. Besides, patients will be more aesthetics and take shorter hospital stay. Recent studies on immunology also show the advantages of endoscopic surgery compared to open surgery. However, all studies reveal the time of an endoscopic surgery is longer than an open surgery. In terms of oncology, according to Kitano S., Huscher, the number of tumors taken and the adequate level of gastrectomy is equal between open and endoscopic surgery. This difference is not statistically significant. In Vietnam, there are also some topics researching on this issue [1,8,11]. Up to now, more and more surgeons have chosen to undergo endoscopic surgery for gastrectomy.
Technique of lymphadenectomy D2
Step 1: Put the Trocart into the abdomen: we use 5 trocarts: 2 10mm-trocart put below the navel and left ribs, 3 5 mm-trocarts placed on the right flank, on either sides of flank or under the chest 4-5 cm. We found that putting 05 trocars is more convenient and easier to perform the surgery than 4 trocars. Specially, two umbilical trocars, we used two Ligasure knives (one is straight and the other is curve) for operating, partial cutting, hemostatic, then we could shorten the time of surgery and lymphadenectomy.
The placement of these first trocars has not had any problems and complications. Placing the next trocarts is quite convenient thanks to the support of observation with the camera.
Step 2: Observe and assess injury: we did not find any difficulty to observe and assess the injury. However, there was 01 case (5.9%): the large caul (large mesenteric) attached to the bottom so we must remove first before pulling it up, there was the other case (5.9%): gallbladder inflammation causing difficulties in hepatic surgery, so the surgery time is long. We must observe and evaluate the entire abdomen before operating. In small intestine or colon, the sticky spots on the large caul must be removed, the large caul must be pulled over, the small intestine must be pulled down easily… These could help facilitate surgery.
Step 3: Taking the entire large caul along the transverse colon. We often perform from outside to near the spleen, tightening the artery of caul which close to the branch of artery of duodenum and the vein of the right junction, at the position of Henler's body, in front of the pancreas to get the group of 4.6 nodes in full cut sets and 4sb, 4d, 6 in semi-stomach section. It was quite smoothly to remove the entire large caul along the transverse colon with ultrasonic scalpel or ligasure scalpel. We did not have any problems in this case. We usually cut wide large caul from the gastric body to the bottom, then pulling the stomach out easier, this is different to open surgery. However, we encountered 03 cases (17.6%) of patients with fat body status, the colon at the corner of the spleen sticking to the abdominal wall so it was more difficult than normal to liberate the large caul. It was similar to liberate the large caul from the transverse colon of the liver. It would be more convenient to use ultrasonic scalpel or ligasure when detaching large caul from the adherence of the transverse and duodenal mesenteric and colon, pancreas. Transverse and mesenteric colon is vulnerable in this stroke. The perforation of mesenteric as well as damage of riolan artery can easily occur if we do not pay any attention.
Step 4: We dissected along the hepatic artery when scraping the area of hepatic stalks, tightening the root of the pyloric artery, can remove 1 or 2 small branches of duodenal artery to take the whole small caul, and to take ganglion groups 5 , 8a, 12a. After removing the small caul, the removal of these ganglion groups is not difficult, especially in thin people with long hepatic stalks. However, we encountered two cases (11.8%) of short hepatic stalks which were quite difficult to undergoing surgery to find group of nodes 12 because they were deep and close to the portal vein. Need to be very careful at this situation.
Step 5: Tightening the left vein thrombosis, lymphadenectomy ganglion groups 7 and 9, we dissected along the hepatic artery and the upper body of the pancreas up to close to the triple junction of visceral arteries, revealing the left gastric artery at origin. We dissected along the common hepatic artery and the upper margin of the body up to the junction of the trunk artery, revealing the left arterial (coronary-gastric artery) root; take ganglion groups 7, 9 or 11p, 11d in the whole cut and 11p in the semicut section along the spleen, pair of clips close to coronary-gastric artery, cut with the ligasure scalpel. The surgery which has the help of a ligasure scalpel or ultrasonic scalpel is not difficult when going into this area. The nodes can be seen quite well and surround organization are quite loose, so removing them is quite easy. Sometimes there are short veins with thin walls that are easy to tear and bleed so it is required an ultrasonic knife or ligasure to stop bleeding. It is necessary to have active support from assistants who help to clearly reveal the surgical position.
Step 6: Lymphadenectomy the ganglion groups 1, 3 with half-cut and 1, 2, 3 with the whole cut. These groups are located close to the right side of the esophagus. The nodes are located next to the esophagus so just using an ultrasonic scalpel or ligasure scalpel to peel the right side to get this ganglion. However, the lymph nodes located close to the esophagus have tought nerve branches X, so the right side of the esophagus must be exposed and the nerve branches must be cut as long as possible, so that the stomach can be taken out easily.
Step 7: Laparotomy with a small hole in the navel to pull the stomach out. We often slit the trocart hole under the chest down to about 4-5 cm. Abdominal incision is performed as open surgery. However, in some cases of large tumors, abdomen can be enlarged so that the tumor can be removed easily. In the case of fat patients with thick abdominal wall, it must also be widen incision for manipulating of suturing stomach easily later or it would be easier to scrape the group 1, 3 through the open surgery if it is essential.
Step 8: Gastrectomy and repeat gastric circulation in 17 cases of successful laparoscopic surgery, we have performed the connection of the gastric and duodenal sections in the form of Billroth II – Finsterer: 14 cases (82.4%), 03 cases (17.6%) connected in the form of Roux - en - Y due to the position of the tumour in the vertical part of the Lesser curvature (01 case), in the 1/3 position of the upper gastric body (01 case) and in the cardia (01 case).
Early results
Our study showed that an average time of a surgery was 190 minutes, an average blood loss of 97.2 minutes, an open surgery rate of 15%.
Some studies show that endoscopic gastrectomy has more advantages than open surgery: short incision, low blood loss, less postoperative pain, early bowel movement, shorter hospital stay, time return to daily activities sooner [12,14,15].
In our study, the average number of lymph nodes dredged is 35.7, the lowest is 19 nodes, the highest is 42 nodes. The result is similar to the author like Trieu Trieu Duong (26.2) [7], Nguyen Hoang Bac (2013) (29.3) [6]. There are no major complications related to scraping tumors. Lymphadenectomy in cancer surgery in general and gastric cancer in particular plays a very important role to ensure radical removal in cancer treatment. This is a highly debated issue when the onset of gastric cancer surgery with endoscopic surgery, so far this has been answered when most of the studies have indicated that the number of dredging nodes is equivalent to open surgery. Many authors also said that with ultrasound scalpel and the magnification of the organization on the screen, the identification and lymphadenectomy are more convenient than open surgery. Thus our study again demonstrates the safety and efficacy of lymphadenectomy during endoscopic gastrectomy.
According to WHO (2000), Microscopic images in this study showed that the metastatic carcinoma is the most common (70%). Cellular carcinoma rings ranked the second (15%). Carcinoma of the mucous glands, squamous glands, papillary glands are less common (Table 2). Cellular carcinoma rings was the most situation which Do Van Trang [4] often faced (37.1%). Do Trong Quyet [3] gave similar results to our study.
Metastatic carcinoma is also divided into 3 levels: High differentiation, moderate differentiation and poor differentiation. The results of our study: High differentiation is 5%, moderate differentiation is 40% and poor differentiation is 55%. The results of Do Trong Quyet [3]: High differentiation is 40,3%, moderate differentiation is 43% and poor differentiation is 16,7%.. There is a difference in this comparison because the subjects of the studies are different, the techniques and the perception of the damage are different. According to the classification of WHO in 2000, more than 95% of structure of tumors take form of glands was classified as high differentiation.
According to the results of classification of the disease stage that we have applied in Table 3.21, our patients are still in a relatively "early" stage (IA + IB + IIA + IIB) (65%), the late patient group ( IIIA + IIIB + IIIC + IV) (35%). This result is different from the statistics on the number of patients who have had surgery of gastric cancer at Viet Duc Friendship Hospital [2] in the past few years: 14.1% and 85.9%, respectively for the "early" and "late" groups. This difference may be due to the choice of subjects for the study, it can also be said that in recent years, thanks to the progress in early detection of diseases due to the development of endoscopic systems everywhere, but it is also impossible to explain this difference convincingly. Obviously, there is the active participation of sergeons in the selection of patients for our research to match a new surgical technique, although there are many advantages but there are also limitations in terms of designation.
It is also reasonable to know that the world's first endoscopic gastric surgeries are also cases of early gastric cancer and will eventually progress to patients with gastric cancer in serious later stage. Many authors also advocate that this technique should only be reserved for cases of early gastric cancer. In our country, now when people have better cognitive conditions as well as conditions for health care, the cases of gastric cancer will be discovered early, and endoscopic gastrectomy with many benefits for patients such as less pain, patients can move them- selves early without the support of others, short time for staying in the hospital…so this will be a valuable treatment. In our study, there was no case of death. There was only 1 case of pleural effusion (5%), 01 case of dumping syndrome (5%). According to some Asian authors as well as Europe, some complications often occur after surgery such as: duodenal leakage, pancreatic leakage, postoperative bleeding, abdominal abscess ... accounting for 6.2 - 35.2%. In a comparative study, Dulucq JL and his colleagues also found that the complication rate in endoscopic surgery was comparable to open surgery [10]. In our study, follow-up of patients after 1 month was recorded on endoscopic surgery that the results of intestinal circulation are good that was similar to that of Trinh Hong Son [8].
CONCLUSION
Performing gastrectomy with Endoscopic surgery which was the initial treatment of gastric cancer showed positive results: short hospital stay, less complications, postoperative pain relief and positive results in terms of oncology.
CONFLIT OF INTEREST
Non.
REFERENCES
1. Nguyen Minh Hai. Initial assessment of supported endoscopic gastrectomy surgery. Medicine of Ho Chi Minh City, thematic endoscopic surgery, appendices 2006;10(4):109–113.
2. Do Duc Van et al. Developing appropriate treatment regimens for stages and possible surgery of gastric cancer disease. Topic of KC 10.06.05 branch of the science and technology project at KC 10.06 state; 2006.
3. Do Trong Quyet. Research on treatment of gastric cancer by surgery combining ELF chemicals and immunization for ASLEM therapy, Doctoral thesis in medicine, Hanoi Medical University; 2010.
4. Do Van Trang. Research on lymphadenopathy by laparoscopic surgery in the treatment of gastric cancer in the pyloric area, Doctor of Medicine thesis, Hanoi Medical University; 2012.
5. Hoang Manh An, Ho Chi Thanh, Dang Viet Dung. Study on gastrectomy surgery, endoscopic D2 lymphadenopathy to support the treatment of stomach cancer at Hospital 103, Surgery, 2011; 61: 19-24.
6. Nguyen Hoang Bac, Vu Duy Long. Results of surgical endoscopic gastroscopy surgery to treat lymphoma treatment, Report at Scientific Conference on endoscopic surgery - IV endoscopy, Can Tho 2013, Summary Report (Abstract, English) p. 51 - 52.
7. Trieu Trieu Duong. Research on gastric cutting techniques, D2 lymph nodes by endoscopic surgery at Hospital 108, Ho Chi Minh City. Ho Chi Minh, 2008;12:204–208.
8. Trinh Hong Son. Lymphatic dredge study in the treatment of gastric cancer surgery, Doctoral thesis in Medicine, Hanoi Medical University, 2001.
9. Danielson H., Kokkola A., Kiviluoto T., Sirén J. et al . Clinical outcome after D1 vs D2–3 gastrectomy for treatement of gastric cancer, Scandinavian Journal of Surgery, 2007:96:35–40
10. Dulucq J.L, Wintringer P, Stabilini C. Laparoscopic and open gastric resections for malignant lesions. Surg Endotsc 2005;19: 933–938.
11. Hochwald S. N., Brennan M. F. et al. Is Lymphadenectomy Necessary for Early Gastric Cancer?, Annals of Surgical Oncology, 1999;6(7):664–670.
12. Ibáňez F. J., J. S. Azagra, M. Goergen, J. M. Bordas, M. L. Almendral, J. M. Erro. Laparoscopic surgery of gastric cancer.An. Sist. Sanit. Navar. 2005; 28 (Supl. 3): 21–31.
13. Kim Min-Chan, Jung.GJ, Kim HH. Morbidity and Mortality of Laparoscopy–Assisted Gastrectomy with Extraperigastric Lymph Node Dissection for Gastric Cancer. Dig Dis Sci 2007;52: 543–548.
14. Kitano Seigo, Shiraishi Norio. Manimally invasive surgery for gastric tumors. Surg Clin N Am 2005;85: 151–164.
15. Tanimura S, M. Higashino, Y. Fukunaga, M. Takemura,Y. Tanaka, Y. Fujiwara, H. Osugi. Laparoscopic gastrectomy for gastric cancer: experience with more than 600 cases. Surg Endosc 2008;22:1161–1164.
TABLES


REFERENCES
1. Nguyen Minh Hai. Initial assessment of supported endoscopic gastrectomy surgery. Medicine of Ho Chi Minh City, thematic endoscopic surgery, appendices 2006;10(4):109–113.
2. Do Duc Van et al. Developing appropriate treatment regimens for stages and possible surgery of gastric cancer disease. Topic of KC 10.06.05 branch of the science and technology project at KC 10.06 state; 2006.
3. Do Trong Quyet. Research on treatment of gastric cancer by surgery combining ELF chemicals and immunization for ASLEM therapy, Doctoral thesis in medicine, Hanoi Medical University; 2010.
4. Do Van Trang. Research on lymphadenopathy by laparoscopic surgery in the treatment of gastric cancer in the pyloric area, Doctor of Medicine thesis, Hanoi Medical University; 2012.
5. Hoang Manh An, Ho Chi Thanh, Dang Viet Dung. Study on gastrectomy surgery, endoscopic D2 lymphadenopathy to support the treatment of stomach cancer at Hospital 103, Surgery, 2011; 61: 19-24.
6. Nguyen Hoang Bac, Vu Duy Long. Results of surgical endoscopic gastroscopy surgery to treat lymphoma treatment, Report at Scientific Conference on endoscopic surgery - IV endoscopy, Can Tho 2013, Summary Report (Abstract, English) p. 51 - 52.
7. Trieu Trieu Duong. Research on gastric cutting techniques, D2 lymph nodes by endoscopic surgery at Hospital 108, Ho Chi Minh City. Ho Chi Minh, 2008;12:204–208.
8. Trinh Hong Son. Lymphatic dredge study in the treatment of gastric cancer surgery, Doctoral thesis in Medicine, Hanoi Medical University, 2001.
9. Danielson H., Kokkola A., Kiviluoto T., Sirén J. et al . Clinical outcome after D1 vs D2–3 gastrectomy for treatement of gastric cancer, Scandinavian Journal of Surgery, 2007:96:35–40
10. Dulucq J.L, Wintringer P, Stabilini C. Laparoscopic and open gastric resections for malignant lesions. Surg Endotsc 2005;19: 933–938.
11. Hochwald S. N., Brennan M. F. et al. Is Lymphadenectomy Necessary for Early Gastric Cancer?, Annals of Surgical Oncology, 1999;6(7):664–670.
12. Ibáňez F. J., J. S. Azagra, M. Goergen, J. M. Bordas, M. L. Almendral, J. M. Erro. Laparoscopic surgery of gastric cancer.An. Sist. Sanit. Navar. 2005; 28 (Supl. 3): 21–31.
13. Kim Min-Chan, Jung.GJ, Kim HH. Morbidity and Mortality of Laparoscopy–Assisted Gastrectomy with Extraperigastric Lymph Node Dissection for Gastric Cancer. Dig Dis Sci 2007;52: 543–548.
14. Kitano Seigo, Shiraishi Norio. Manimally invasive surgery for gastric tumors. Surg Clin N Am 2005;85: 151–164.
15. Tanimura S, M. Higashino, Y. Fukunaga, M. Takemura,Y. Tanaka, Y. Fujiwara, H. Osugi. Laparoscopic gastrectomy for gastric cancer: experience with more than 600 cases. Surg Endosc 2008;22:1161–1164.
ARTICLE INFO
DOI: 10.12699/jfvpulm.10.30.2019.1
Conflict of Interest
Non
Date of manuscript receiving
06/02/2019
Date of publication after correction
15/3/2019
Article citation
Dao Quang M. Study on pleural complications, techniques, and results of early gastrectomy plus lymphadenectomy D2 by endoscopic surgery in Thanh Nhan hospital. J Func Vent Pulm 2019;30(10):1-8.