
 English
English
 French
French
Evaluating the respiratory compromise of primary liver tumor treatment by high-frequency waves under the guidelines of ultrasonic surgery in patients with normal lung function
Évaluation de complication respiratoire du traitement d'une tumeur hépatique primaire par ondes haute fréquence selon les directives de la chirurgie par ultrasons chez les patients ayant la fonction pulmonaire normale
M. Dao Quang
Thanh Nhan Hospital. Hanoi—Vietnam
Corresponding author
Dr. Dao Quang Minh
Thanh Nhan Hospital. Hanoi - Vietnam
E-mail: prof.minhdao@gmail.com
ABSTRACT
Objective. Evaluating the respiratory compromise of primary liver tumor treatment by high frequency waves in spatients with normal lung function at Thanh Nhan Hospital.
Subjects and methods. Retrospective descriptive case-study of multi-location and large-size primary liver cancer treated with high-frequency multi-electrode radiofrequency at Thanh Nhan hospital from January 2016 to December 2018.
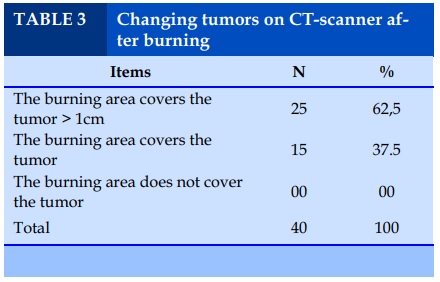
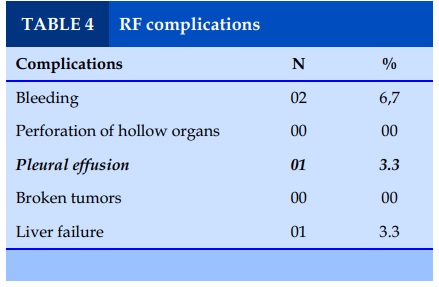
Results. 30 cases, the study group had 22 cases of endoscopic surgery, 08 cases of RFA matching through ultrasound, 08 cases of intervention in combination. 100% of the burning area covered the entire tumor on CT-scanner. The rate of complications was 13.3%. There were 2/30 cases recurring after 6 months. Average time of surviving: 12.9 ± 5.3 months.
Conclusion. Heat burning with high-frequency waves is a feasible method for cases of cancer patients without the possibility of surgery. It has been increasingly applied in our country for cancer treatment of liver cells from provincial to central hospitals.
KEYWORDS: Respiratory compromise; Lung function; Liver cancer; High-frequency wave burning.
RÉSUMÉ
Objectif. Évaluation des complications respiratoires du traitement d'une tumeur hépatique primaire par ondes haute fréquence chez les patients ayant la fonction pulmonaire normale à l'hôpital Thanh Nhan.
Sujets et méthodes. Étude de cas descriptive rétrospective d'un cancer primitif du foie de grande taille et multi-localisation traité par radiofréquence haute fréquence multi-électrodes à l'hôpital Thanh Nhan de janvier 2016 à décembre 2018.
Résultats. Dans 30 cas, le groupe d’étude avait 22 cas de chirurgie endoscopique, 08 cas d’appariement RF par échographie, 08 cas d’intervention combinée. La totalité de la zone de combustion recouvrait la totalité de la tumeur sur un scanner. Le taux de complications était de 13,3%. Il y avait 2/30 cas récurrents après 6 mois. Durée moyenne de survie: 12,9 ± 5,3 mois.
Conclusion. La combustion de chaleur avec des ondes à haute fréquence est une méthode réalisable pour les patients cancéreux sans possibilité de chirurgie. Il est de plus en plus utilisé dans notre pays pour le traitement du cancer des cellules du foie, des hôpitaux provinciaux aux hôpitaux centraux.
MOTS CLÉS: Complication respiratoire; Fonction pulmonaire; Cancer hépatique; Brûlage à haute fréquence.
INTRODUCTION
Liver cancer, mainly hepatocellular carcinoma (referred as liver epithelium cancer, is one of the most common types of cancer and the third leading cause of cancer death, after lung cancer and stomach cancer. Vietnam is among the countries with the highest prevalence of liver epithelium cancer in the world. Liver epithelium cancer is a type of cancer with a poor prognosis; most cases detect the disease in advanced or late stages, not suitable for radical treatments such as liver cutting surgery, liver transplantation. Until now, surgery is still considered the optimal treatment for liver epithelium cancer. However, this method is only applicable to about 20-30% of cases at the time of diagnosis. Therefore, most HCC patients are treated with non-surgical methods, in which methods of removing tumors by physical and chemical agents are widely used.
In 1993, Rossi first reported the treatment of liver tumors by burning with high frequency waves through the skin under the guidance of ultrasound. Another study of Bilchik 2001 indicated that liver burning combined with open or endoscopic surgery for patients with multifocal large size liver tumors will achieve optimal results. In August 2002, at Gastroenterology department of Bach Mai Hospital, the method of treating liver cancer by highfrequency heat wave was conducted for many patients. In March 2003, Le Loc treated liver tumors and liver metastasis up to 10 cm by RFA through open surgery without complication and with good results [1-4].
Thanh Nhan Hospital has applied high frequency waves to treat liver tumors and liver metastases under the guidance of ultrasound and combined surgery since 2010 which initially has positive results. Research’objective is to evaluate the results of liver tumor treatment with high frequency waves at Thanh Nhan Hospital from January of 2016 to December of 2018.
SUBJECTS AND METHODS
Subjects: 30 patients with primary, multifocal and large-sized liver cancer treated by burning liver cancer by multi-electrode high-frequency heat wave combined with surgery at Thanh Nhan Hospital from January 2016 to December 2018. The research subjects include: -Group 1: cases treated with high frequency waves combined with ultrasound. -Group 2: cases treated with high frequency waves combined with endoscopic surgery.
Retrospective, cross-sectional, non-controlled descriptive studies. Processing data on SPSS 20.0 software. Extra time of surviving is calculated according to Kaplan - Meier method
RESULTS
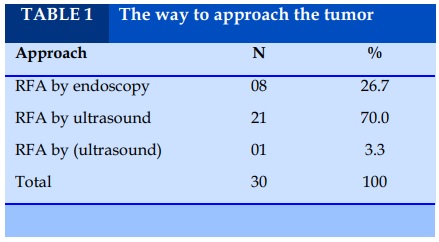
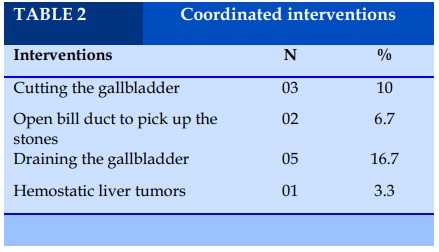
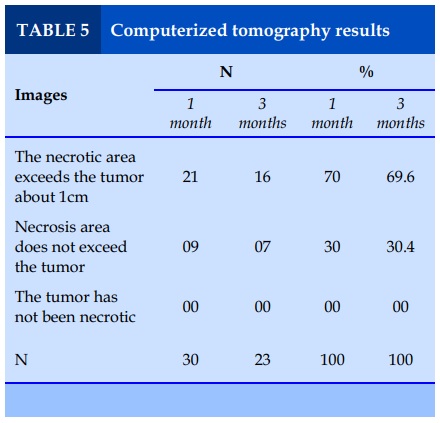
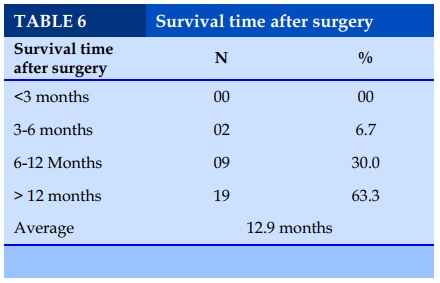
RFA characteristics (Table 1, 2, 3, 4, 5, 6)
DISCUSSIONS
In our study, there are 2 groups: EC (endoscopy) group (26.7%) and RFA group through ultrasound with 21/30 cases with navigation (70%), a case changed from endoscopic surgery to open surgery because of sticky abdominal condition.
According to the research by Zenichi Morise (2014), there are 34 endoscopic RFA cases with an average survival time of 16.9 ± 8.3 months, no deaths related to surgical complications, an additional survival time of 14, 7 ± 6.9 months, the rate of recurrence in the liver is 61.8% RFA endoscopic surgery is a minimally invasive method that causes less liver dysfunction [5].
There are 22 tumors with only one RF accounting for 55%, 13 tumors with 2 RF times (32.5%), the percentage of tumors with 3 RF times is 12.5%, and these are large tumors. Following the research by Yamakado K. Nakasuka A (2003), with tumors of 5-7cm size need at least 2 burns to ensure the necrosis area exceed the tumors even with multi-electrode needles [6].
The average RF time of under 5cm tumor group was 18 ± 2.3 minutes, the group with tumor of 5-7 cm was 25 ± 5.1 minutes and the group with tumor of over 7 cm was 33 ± 6.4 minutes. The author Shiina S, Teratani T (2005) with 52 cases of tumors below 5 cm, the maximum temperature is usually maintained for 8 minutes once and continues the burn waves after withdrawing the needle to 1.5 cm, the average time of wave burning is 14.1 ± 8.2 (8-48 minutes). Compared to other authors, our average time is lower due to the use of multi-electrode burners.
Among 8 cases of coordinated intervention, 02 cases with gallbladder stones, the gallbladder were cut to open the main bile duct to remove stones, draining Kehr, 05 cases of child B cirrhosis with increased bilirubin jaundice before surgery, we try to drain the gallbladder to reduce the risk of cholestasis causing liver failure. In addition, there was 1 case with ruptured liver tumors in Child B Cirrhosism so we could not cut the liver. We had hemostatic surgery and burned liver tumors. We noticed in the surgery showed that RFA not only coagulated tumors but also helped increase the ability of stopping bleeding.
According to Murakami T, Imai Y, Okada M. et al. (2011) Computerized tomography is usually carried out immediately after heat burning and at times after 1, 3, 6, 9, 12 months in the first year, every 6 months in the following years. However, in order to evaluate early the effectiveness of treatment for cases of CT scans after 5 days of burning with high frequency waves. There were 18 cases (60%) that did not absorb the medicine, the burning area covered the tumor and 12 cases (40%) of the burning area covered the tumor totally [7].
The rate of complications of the two groups of open surgery and endoscopic surgery is not different; there are 2 cases of bleeding in the liver bag, accounting for 6.7%, 1 case of pleural effusion and a case of liver failure. In the case of liver failure and large size tumor of 9 cm in the central lobe central area of 8a and 8b, we have to perform RF 3 times. After 1 day of ALT surgery, AST increased above 800U/mL, bilirubin increased >400µmol/L, Prothrombin decreased below 30%. Before the surgery of cases with Child B cirrhosis, the indexes only fluctuate below 10% around the threshold. In the study by Dao Van Long with 105 cases of RF, there were 5 cases with complications accounting for 5%, in which there were cases of liver abscess.
Koda M, Ueki M et al. (2004) who burned a wave of 3554 tumors for 2320 cases, indicated a complication rate of 2.2%, including septic shock, intestinal perforation, and organ failure and bleeding. Mortality rate is 0.3%. The complication rate of Riccardo L (Italy)
treated 187 cases and Curley S with 304 cases of 2% [8].
Our results are consistent with the research results of Hechelhammer L et al. in 137 cases of liver cell cancer (average tumor size of 6.36 ± 1.1cm) to meet the requirement completely of burning tumors by high frequency waves. After 5 years of observation, the extra survival time rate without relapse was only 8.9%. Local recurrence rate was 48/137 (35.1%), the rate of new location recurrence was 39/137 (28.5%) with an average relapse time of 13 months (4-32 months). Particularly, relapses increase in cases of liver tumors> 5cm before treatment [9].
Regarding computerized tomography: At the time of 1 month of follow-up, among 30 cases with computerized tomography, there were 21 cases of necrosis excessing the tumor (70%), 9 cases (30%) of tumor necrosis, no case with tumors left. At the time of 3 months after discharge, we have not seen any confirmation of the new or relapsed liver tumors. At the time of 6 months, we found tumors in 2 cases. In the first case, the tumor had the size of 12mm x 9mm in the lower lobe 4 while the old tumor was in the lower lobe 8. In the second case, the tumor had the size of 8mm x 13mm, in the lower lobe 5 while the old tumor in the lower lobe 4. These cases received palliative treatment and support treatment. The cause of relapse in both cases is the cirrhosis of the hepatitis, a case of hepatitis B and another with a combination of hepatitis B and C.
According to Dhanasekaran R, there were 34 cases of endoscopic RF with an average survival time of 16.9 ± 28.3 months, no death related to surgical complications, an extra survival time of 14.7 ± 6.9 months , the relapse rate in the liver was 61.8% [10].
The study of Prajapati HJ (2012) 122 RFA times with primary liver cancer could not be removed from April 1997-12 / 2006. The time from diagnosis to RF implementation was 2 months (1-4.2), Kaplan-Meier average survival time was 26 months in which Child A was 28 months, Child B was 15 months, and Child C was 5 months. In our study, the average survival time after surgery was 12.9 ± 5.3 months, the shortest was 4.5 months. There were 2 cases (6.7%) with the survival time of 3-6 months, 6 cases (20%) of 6-12 months, 13 cases (43.3%) over 12 months.
CONCLUSION
Long-term survival time is the most important criterion to evaluate the effectiveness of the treatment method in cancer. For hepatocellular carcinoma, liver cutting or liver transplantation is still the most optimal treatment, enabling the longer survival life time for patients. However, the number of cases meeting with the requirements of the treatment indications is still low. Therefore, heat burning with high -frequency waves is a feasible method for cases of hepatocellular carcinoma without the possibility of surgery treatment. In fact, the method of heat burning surgery by high frequency waves has been widely applied in our country in the treatment of liver cell cancer from provincial to central hospitals.
CONFLIT OF INTERESTS
Non.
REFERENCE
1. Rossi S, Di Stasi M, Buscarini E, et al. Percutaneous RF interstitial thermal ablation in the treatment of hepatic cancer. AJR 1996;167:759-68.
2. Bilchik AJ, Rose DM, Allegra DP, Bostick PJ, Hsueh E, Morton DL. Radiofrequency ablation: a minimally invasive with multiple applications. Cancer J Sci Am 1999;5:356-61
3. Le Loc, PhanThanh Hai. Initial treatment for primary and secondary liver cancer with Radiofrequency. Vietnamese medicine 2004;297. 19-23.
4. Le Loc, Hoang Trong Nhat Phuong, High-frequency heat burns on the way of cutting liver cancer reduces blood loss during surgery. Vietnam Liver Journal 2007. 54-58.
5. Zenichi Morise. Recent advances in the surgical treatment of hepatocellular carcinoma. World Journal of Gastroenterology 2014; 20(39):14381-1392.
6. Yamakado K, Nakasuka A, et al. Combination therapy with radiofrequency ablation and transcatheter chemoembolization for the treatmenf of hepatocellular carcinoma: Short term recurrences and survival. Oncology 2003; 11: 105-109.
7. Murakami T., Imai Y., Okada M., et al, "Ultrasonography, Computed Tomography and Magnetic Resonance Imaging of Hepatocellular Carcinoma: Toward Improved Treatment Decisions", Oncology, 2011; 81(s1):86-99.
8. Koda M, Ueki M. The influence on liver parenchymal function and complications of radiofrequency ablation or the combination with transcatheter arterial embolization for hepatocellular carcinoma. Hepatology Research. 2004;29:18- 23
9. Hechelhammer L, Pfiffner R, Marincek B, Pfammatter T. Ablation percutanée par radiofréquence de tumeurs du foie, du rein et des poumons. Forum Med Suisse 2008;8(38):710–712.
10. Dhanasekaran R., Kooby DA., Staley CA., et al. Prognostic factors for survival in patients with unresectable hepatocellular carcinoma undergoing chemoembolization with doxorubicin drug-eluting beads: a preliminary study 2009; Hpb., 12(3), pp. 174180.
TABLES
REFERENCE
1. Rossi S, Di Stasi M, Buscarini E, et al. Percutaneous RF interstitial thermal ablation in the treatment of hepatic cancer. AJR 1996;167:759-68.
2. Bilchik AJ, Rose DM, Allegra DP, Bostick PJ, Hsueh E, Morton DL. Radiofrequency ablation: a minimally invasive with multiple applications. Cancer J Sci Am 1999;5:356-61
3. Le Loc, PhanThanh Hai. Initial treatment for primary and secondary liver cancer with Radiofrequency. Vietnamese medicine 2004;297. 19-23.
4. Le Loc, Hoang Trong Nhat Phuong, High-frequency heat burns on the way of cutting liver cancer reduces blood loss during surgery. Vietnam Liver Journal 2007. 54-58.
5. Zenichi Morise. Recent advances in the surgical treatment of hepatocellular carcinoma. World Journal of Gastroenterology 2014; 20(39):14381-1392.
6. Yamakado K, Nakasuka A, et al. Combination therapy with radiofrequency ablation and transcatheter chemoembolization for the treatmenf of hepatocellular carcinoma: Short term recurrences and survival. Oncology 2003; 11: 105-109.
7. Murakami T., Imai Y., Okada M., et al, "Ultrasonography, Computed Tomography and Magnetic Resonance Imaging of Hepatocellular Carcinoma: Toward Improved Treatment Decisions", Oncology, 2011; 81(s1):86-99.
8. Koda M, Ueki M. The influence on liver parenchymal function and complications of radiofrequency ablation or the combination with transcatheter arterial embolization for hepatocellular carcinoma. Hepatology Research. 2004;29:18- 23
9. Hechelhammer L, Pfiffner R, Marincek B, Pfammatter T. Ablation percutanée par radiofréquence de tumeurs du foie, du rein et des poumons. Forum Med Suisse 2008;8(38):710–712.
10. Dhanasekaran R., Kooby DA., Staley CA., et al. Prognostic factors for survival in patients with unresectable hepatocellular carcinoma undergoing chemoembolization with doxorubicin drug-eluting beads: a preliminary study 2009; Hpb., 12(3), pp. 174180.
ARTICLE INFO
DOI: 10.12699/jfvpulm.10.30.2019.46
Conflict of Interest
Non
Date of manuscript receiving
22/01/2019
Date of publication after correction
16/3/2019
Article citation
Dao Quang M. Evaluating the respiratory compromise of primary liver tumor treatment by high-frequency waves under the guidelines of ultrasonic surgery in patients with normal lung function. J Func Vent Pulm 2019;30(10):46-49.