
 English
English
 French
French
Study of forced expiratory flow of 25% - 75% values (FEF25-75) in the control of asthma according to GINA
Étude du débit expiratoire forcé de 25% - 75% des valeurs (DEF25-75) dans le contrôle de l'asthme selon GINA
P. Dang The1, T. Tran Van2, S. Duong-Quy2,3,4
1: Ward 4 Hospital. Ho Chi Minh city. Vietnam
2: Internal Medicine Department. Pham Ngoc Thach University of Medicine. Vietnam
3: Clinical Research Center. Lam Dong Medical College. Vietnam
4: Division of Immuno-Allergology. Penn State Medical College. USA
Corresponding author
Dr. Dang The Phong
Ward 4 Hospital. Ho Chi Minh city. Vietnam
E-mail: phong2625488107@gmail.com
ABSTRACT
Objective. To study forced expiratory flow values of 25% - 75% (FEF25-75) in assessing the level of asthma control.
Subjects. Patients visiting the asthma management unit at the People's Hospital of Gia Dinh, have been diagnosed with asthma.
Methods. Cross-sectional description, involving 222 patients with asthma were included and received the lung function testing to compare FEF25% -75% with the control level of asthma.
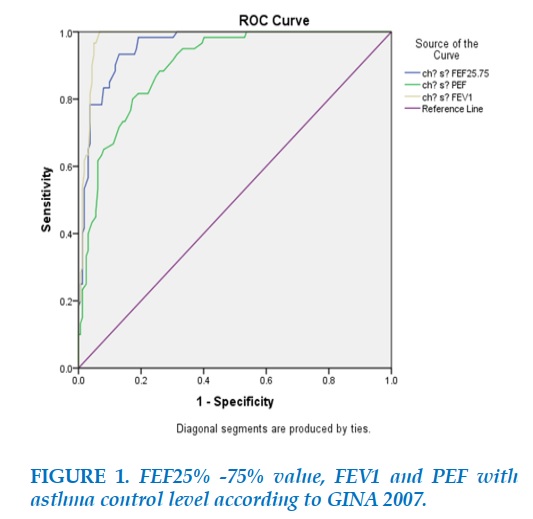
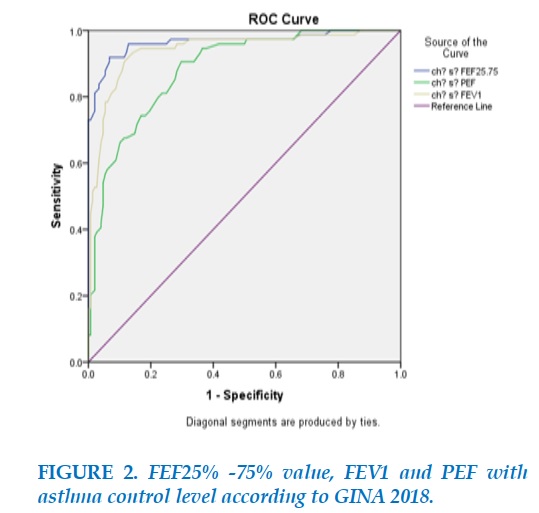
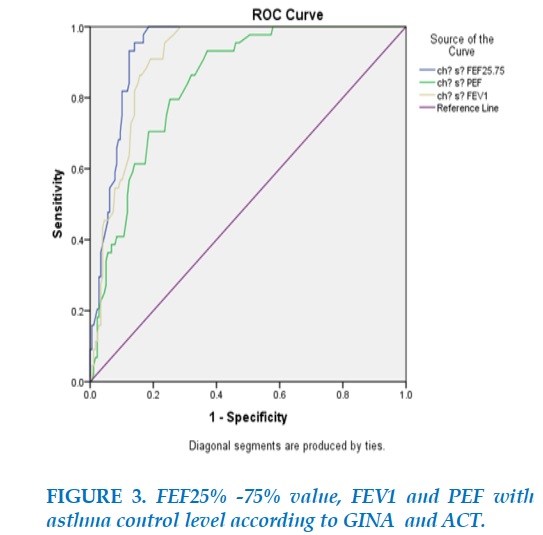
Results. FEF25% -75% values, FEV1, PEF and the level of asthma control were done according to GINA 2007. Results obtained: FEV1 (AUC = 97.9%), FEF25% -75% (AUC = 95.7 %), PEF (AUC = 89.8%). When comparing the above three indicators, FEV1 had the highest value in assessing the level of asthma control defined by GINA 2007. The values of FEF25% -75%, FEV1, PEF and the level of asthma control under GINA 2018 showed FEF25% -75% (AUC = 96.5%), FEV1 (AUC = 94.1%), PEF (AUC = 88.3%). When comparing the above three indicators, FEF25% -75% had the highest value in assessing the level of asthma control according to GINA 2018. Values of FEF25% -75%, FEV1, PEF and the assessment of asthma control level according to ACT showed FEF25% -75% (AUC = 93.5%), FEV1 (AUC = 90.0%), PEF (AUC = 84.3%). When comparing the above three indicators, FEF25 % -75% had the highest value in assessing the level of asthma control according to the ACT.
Conclusion. FEF25% -75% values were related to the degree of asthma control; therefore, the measure of this value may give a new parameter in the management of asthma.
KEYWORDS: Asthma; Asthma control; Forced expiratory flow; FEF25%-75%.
RÉSUMÉ
Objectif. Étude sur débit expiratoire forcé des valeurs de 25% - 75% (DEF25%-75%) dans l'évaluation du niveau de contrôle de l'asthme.
Sujets. Des patients étaient à l’unité de prise en charge de l'asthme de l'Hôpital Populaire de Gia Dinh.
Méthodes. Il s’agit d’une étude descriptive et transversale, impliquant 222 patients souffrant d'asthme qui ont été inclus pour la mesure de la fonction pulmonaire afin d’évaluer le degré de contrôle de l'asthme et de comparer DEF25%-75% avec le niveau de contrôle de l'asthme et VEMS, DEP des trois groupes de patients.
Résultats. DEF25%-75%, VEMS, DEP dans l'évaluation du niveau de contrôle de l'asthme selon GINA 2007: résultats obtenus: VEMS (AUC = 97,9%), DEF25%-75% (AUC = 95,7%), DEP (AUC = 89,8 %); en comparant les trois indicateurs cidessus, VEMS avait la valeur la plus élevée pour évaluer le niveau de contrôle de l'asthme selon GINA 2007. Valeurs DEF25%-75%, VEMS, DEP pour évaluer le niveau de contrôle de l'asthme selon GINA 2018: les résultats ont été: DEF25%- 75% (ASC = 96,5%), VEMS (AUC = 94,1%), DEP (AUC = 88,3%); en comparant les trois indicateurs ci-dessus, DEF25%-75% a la valeur la plus élevée dans l'évaluation du niveau de contrôle de l'asthme selon GINA 2018. Valeur de DEF25%-75%, VEMS, DEP dans l'évaluation du niveau de contrôle de l'asthme selon ACT: le résultat était: DEF25%-75% (AUC = 93,5%), VEMS (AUC = 90,0%), DEP (AUC = 84,3%); lorsque l'on compare les trois indicateurs ci-dessus, DEF25%-75% avait la valeur la plus élevée pour évaluer le niveau de contrôle de l'asthme selon l'ACT.
Conclusion. La valeur DEF25%-75% a été liée au degré de contrôle de l'asthme, donc la mesure de cette valeur ouvre une nouvelle paramètre dans la prise en charge de l'asthme.
MOTS CLÉS: Asthme; Contrôle de l’asthme; Dépit expiratoire forcé; DEF25%-75%.
INTRODUCTION
Asthma is a common chronic disease of all ages. According to the World Health Organization (WHO), an estimated 300 million people in the world today suffer from asthma, predicting that number will increase to 400 million by 2025 [1]. Well asthma control is therefore important for patients. Asthma control means that the degree of asthma effect can be observed in a patient, either diminished, or diminished by treatment. Asthma control has two issues: symptom control and risk factors that make disease outcomes worse in the future, to avoid the occurrence of asthma attacks, which are life-threatening [2]. Poor asthma control will make the disease worse and worse, lead to asthma attacks and lead to irreversible bronchial obstruction. In addition, when it has been uncontrolled, asthma can give a burden to the patient such as loss of working days, increased drug treatment costs, greatly affecting the health and quality of daily life of patients, or leading to death. It becomes a burden not only for patients and their families but also for healthcare .
Therefore, asthma control is a key element in the management of people with asthma, and asthma management is not about cure, but good control.
Although asthma is completely manageable, only 5% of patients have achieved GINA disease control criteria (2004) [3]. In our country, only 39.7% of adults achieve asthma control. Asthma control is an important activity for asthmatics who can assess asthma control by a variety of methods. Currently, there are many methods of assessing asthma control currently applied in asthma management departments including GINA 2007 [4,5], GINA 2018 [2], ACT [6-10].
However, there are studies of scientists who suggest that 25% -75% of FEF values contribute to the diagnosis and control of asthma [11,12]. This is why we conducted this study. In Vietnam, there is currently no study on FEF value of 25-75% in asthma control, so we conducted this study with the aim of assessing the value of FEF25% -75% in controlling asthma. of the patient. The results of this project will help physicians assess the degree of asthma control for patients.
METHODS
Study subjects. The study subjects were patients who had come to the asthma management clinic at Nhan Gia Gia Dinh Hospital and who had been diagnosed with asthma.
Selection criteria. Patients > 12 years old diagnosed with asthma according to GINA 2018 criteria; patients with asthma management recorded >3 months and currently have no symptoms of an acute asthma attack; patient was measured lung function testing; patient was consulted, and agreed to participate in the present study.
Exclusion criteria. Patients with other accompanying lung diseases such as tuberculosis, COPD, or pregnant and lactating patients; patients with associated cardiovascular diseases such as heart failure, hypertension, or arrhythmia …; patients had no lung function testing with bronchodilator test was performed.
Study process
Assessing clinical and subclinical characteristics in the study group with asthma patients who were visited at the asthma management unit; assessing the degree of asthma control of the study group according to GINA 2007, GINA 2018 and the ACT questionnaire. They were divided into 3 groups of patients: well-controlled asthma patients group, partially controlled asthma patients group and uncontrolled asthma patient group; patient's measured respiratory results concerning FEF25%-75% values were compared with the above three patient groups and their FEV1 and PEF results.
Statistical analysis
Data analyzed with EPIDATA management software, process and analyze data using SPSS for Windows 10 software with p <0.05 as significant difference; ROC curve was used to compare the sensitivity and specificity of FEV1, FEF25% -75% and PEF in assessing the level of asthma control.
RESULTS
During the one year period from October 2018 to October 2019, 222 patients with asthma were eligible for the study and the results were as follows:
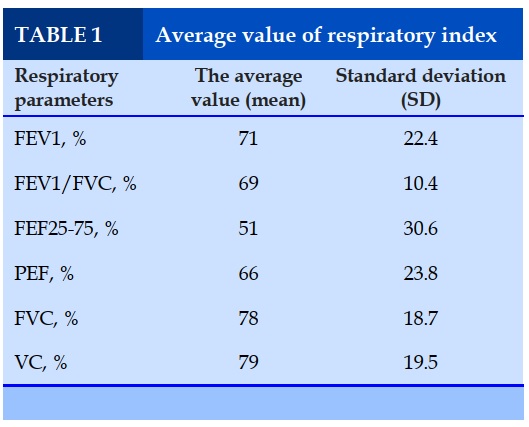
Average value of respiratory indices (FEV1, FEV1 / FVC, FEF25% -75%, PEF, VC, FVC). (Table 1)
The average index of FEV1 was 71%; the average index of FEV1 / FVC was 69%; the average index of FEF25% -75% was 51%; the average index of PEF was 66%; the average index of FVC was 78%and average of VC was 79%.
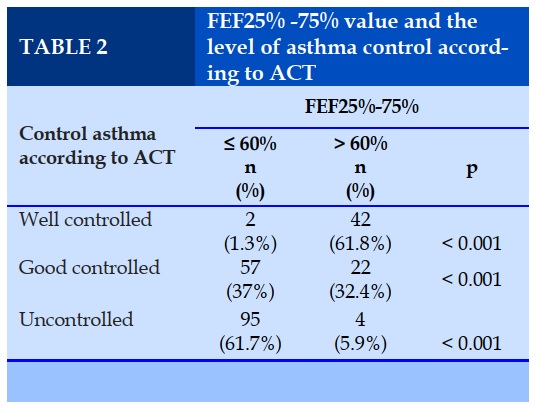
FEF25% -75% values and the level of asthma control according to the ACT (Table 2)
FEF 25% -75% values in patients with complete control of asthma according to ACT standards tended to increase (p <0.001). However, in asthmatic patients who had totally controlled asthma, there was still 1.3% incidence of asthma with FEF25% -75% ≤ 60%.
In well-controlled asthmatic patients, up to 37% of patients had FEF25% -75% ≤ 60%; and in asthmatic patients, the FEF value of 25% -75% reflected quite accurately, when 61.7% of asthma patients had FEF25% -75% ≤ 60%.
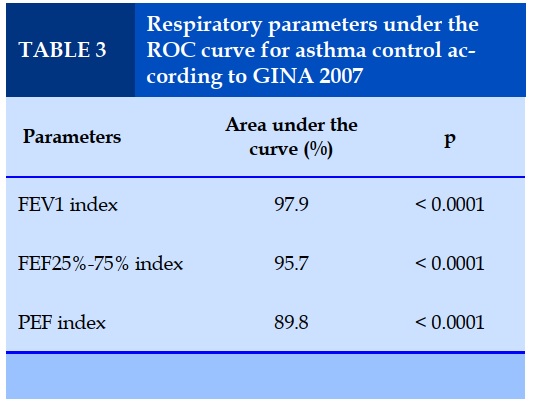
Correlation of FEF25%-75%, FEV1 and PEF with the level of asthma control according to GINA 2007
The area under the curve of FEV1 had the highest value in asthma control 2007 (AUC = 97.9%; p < 0,001) (Table 3); the cut-off point of FEV1 was 0.932, with sensitivity = 1, and specificity = 0.932. It was followed by the area under the curve of FEF25% - 75% with the second rank in asthma control (AUC = 95.7%; p <0.001) (Table 3).
The cut-off point of FEF25% -75% was 0.804, with sensitivity = 0.933, specificity = 0.87; and finally, the area under the curve of the PEF (AUC = 89.8%, p < 0,001) (Table 3); the cut-off point of the PEF was 0.627, with sensitivity = 0.8, and specificity = 0.827.
Thus, when comparing the three values with the evaluation of asthma control level under GINA 2007, FEV1 had the highest value in assessing asthma control, with AUC = 97.9%.
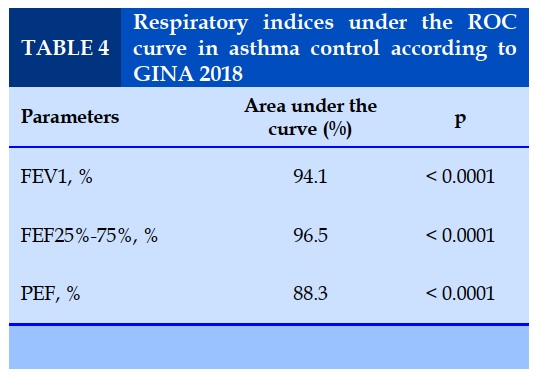
Evaluation of FEF25%-75%, FEV1 and PEF in compare to asthma control defined by GINA2018 (Table 4)
The area under the curve of FEF25% -75% had the highest value in asthma control 2018 (AUC = 96.5%; p = 0.000) (Table 5); the cut-off point of FEF25% -75% = 0.851, with sensitivity = 0.92 and specificity = 0.932. The second was the area under the curve of FEV1 in asthma control (AUC = 94.1%; p = 0,000) (Table 5); the cut-off point of FEV1: 0.791, with sensitivity = 0.990 and specificity = 0.885 .
And finally, the area under the curve of the PEF, which was of agreed value in asthma control 2018 (AUC = 88.3%; p = 0.000) (Table 5); the cut-off point of PEF: 0.608, with sensitivity = 0.955 and specificity = 0.703.
Thus, when comparing the above three values in the evaluation of asthma control according to GINA 2018, the FEF25% -75% was the highest value in the assessment of asthma control.
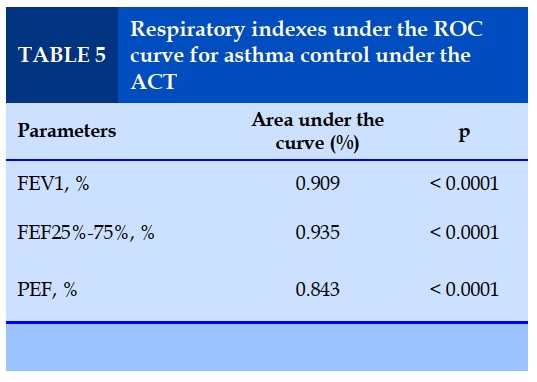
Study of the value of FEF25% -75%, FEV1 and PEF with the level of asthma control according to the ACT
The area under the curve of FEF25% -75% (AUC = 93.5%; p = 0,000) had the highest value in controlling asthma according to ACT (AUC = 93.5%; p = 0,000) (Table 5); cut-off point of FEF25% -75%: 0.814, with sensitivity = 0.96 and specificity = 0.86).
The area under the curve of FEV1 which had the second highest value in asthma control according to ACT (AUC = 90.9%; p <0.0001) (Table 5); the cut-off point of FEV1: 0.719, with sensitivity = 0.96 and specificity = 0.76.
Finally, the area under the curve of the PEF, had the lowest of the three values when compared to the level of asthma control according to the ACT (AUC = 84.3%; p <0.001) (Table 5); cut-off point of PEF: 0.561, with sensitivity = 0.932 and specificity = 0.63.
Thus, when comparing all three values in ACT control asthma, FEF25% -75% had the highest value in assessing asthma control according to ACT.
DISCUSSION
According to the study of 222 patients, and comparing the FEF25% -75% values with FEV1 and PEF in asthma control, we obtained the following results:
The area under the curve of FEF25% -75% has the second value in controlling asthma 2007 (AUC = 95.7%; p = 0.000), the cut-off point of FEF25% -75% is 0.804, with sensitivity = 0.933, specificity = 0.87.
The area under the curve of FEF25% -75% has the highest value in controlling asthma 2018 (AUC = 96.5%; p = 0,000), the cut-off point of FEF25% -75%: 0.851, with sensitivity = 0.92 and specificity = 0.932.
The area under the curve of FEF25% -75% has the highest value in controlling asthma according to ACT (AUC = 93.5%; p = 0,000), the cut-off point of FEF25% -75%: 0,814, with sensitivity = 0.96 and specificity = 0.86).
Value of FEF25% -75%, FEV1 and PEF with level of asthma control according to GINA 2007
When comparing the 3 values with the assessment of asthma control level according to GINA 2007, FEV1 has the highest value in assessing asthma control, with AUC = 97.9%, while FEF25% -75% with AUC = 95.7%, ranked as second value after FEV1. This result shows that FEF25% -75% is also valuable in use as a reference index to assess the patient's asthma control level as recommended previously [13-18].
Values of FEF25% -75%, FEV1 and PEF with level of asthma control according to GINA 2018
The area under the curve of the PEF, which is of lower value in asthma control 2018 (AUC = 88.3%; p = 0.000) (Table 3.22), the cut-off point of the PEF: 0.608, with sensitivity = 0.90% and specificity = 0.703. Thus, when comparing the above 3 values in the evaluation of asthma control according to GINA 2018, the FEF25% -75% is the highest value in the assessment of asthma control.
FEF25% -75%, FEV1 and PEF values with ACT control degree of asthma
The area under the curve of FEV1, which has the second-highest value in asthma control according to ACT. The area under the curve of the PEF, has the lowest of the three values when compared to the level of asthma control according to the ACT (AUC = 84.3%; p = 0,000 ), PEF cutoff point: 0.561, with sensitivity = 0.932 and specificity = 0.63. Thus, when comparing all three values in ACT control asthma, FEF25% -75% has the highest value in assessing asthma control according to ACT.
CONCLUSION
FEF25% -75% has the highest value in assessing the level of asthma control according to GINA2018. When comparing to FEV1 and PEF, FEF25% -75% is the highest value in assessing the level of asthma control according to the ACT.
CONFLT OF INTEREST
Non.
REFERENCES
1. Loftus PA, Wise SK (2015), "Epidemiology and economic burden of asthma", International Forum of Allergy & Rhinology. 5(1), 7-10.
2. GINA (2018), Global Strategy for Asthma Management and Prevention.
3. Helen K. Reddel, Eric D. Bateman, Allan Becker (2015), "A summary of the new GINA strategy: a roadmap to asthma control", European Respiratory Journal. 46(3), 622-639.
4. GINA (2007), Global Strategy for Asthma Management and Prevention.
5. MD, Bethesda (2007), Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma, National Heart, Lung and Blood Institute US.
6. Grzelewska-Rzymowska IF, Mikołajczyk J, Kroczyńska-Bednarek J, Górski P (2015), "Association between asthma control test, pulmonary function tests and non-specific bronchial hyperresponsiveness in assessing the level of asthma control", Pneumonol Alergol Pol. 83(4), 266-274.
7. Nathan RA và các cộng sự. (2004), "Development of the asthma control test: a survey for assessing asthma control", The Journal of Allergy and Clinical Immunology. 113(1), 59-65.
8. Schatz M, Kosinski M, Yarlas AS, Hanlon J, Watson ME, Jhingran P (2009), "The minimally important difference of the Asthma Control Test", The Journal of Allergy and Clinical Immunology. 124(4), 719-723.e1.
9. Thomas M, Kay S, Pike J, Williams A, Rosenzweig JR, Hillyer EV, Price D (2009), "The Asthma Control Test (ACT) as a predictor of GINA guideline-defined asthma control: analysis of a multinational cross-sectional survey", Primary Care Respiratory Journal. 18(1), 41-49.
10. Waibel V, Ulmer H, Horak E (2012), "Assessing asthma control: symptom scores, GINA levels of asthma control, lung function, and exhaled nitric oxide", Pediatr Pulmonol 47(2), 113-118.
11. Ciprandi G, Cirillo I, Pasotti F, Ricciardolo FL. FEF25- 75: a marker for small airways and asthma control", Annals of Allergy, Asthma and Immunology2013;(3), 233-4.
12. E.Gibb, D. Kaplan, S.M. THyne, N.P. Ly (2012), "FEF25%-75% as a predictor of Asthma severity in children", B61 Pediatric Asthma, A6801.
13. H Dinh-Thi-Dieu, A Vo-Thi-Kim, H Tran-Van, T TangThi-Thao, S. Duong-Quy. Study of the beneficial role of exhaled nitric oxide in combination with GINA guidelines for titration of inhaled corticosteroids in children with asthma. Journal of Breath Research; 2020.
14. L Mansfield, S Duong-Quy, T Craig. Burden of Asthma and Role of 2.5 µg Tiotropium Respimat® as an AddOn Therapy: A Systematic Review of Phase 2/3 Trials. Advances in therapy,2019; 1-13.
15. S Duong-Quy. Clinical Utility Of The Exhaled Nitric Oxide (NO) Measurement With Portable Devices In The Management Of Allergic Airway Inflammation And Asthma. Journal of Asthma and Allergy2019; 12, 331.
16. T Ho-Ly-Minh, S Bui-Binh-Bao, S Duong-Quy. The meaning of sputum eosinophil in childhood asthma and its current application. Journal of Functional Ventilation and Pulmonology 2018; 9 (26), 3-7.
17. T Hua-Huy, S Duong-Quy. Lung function testing in chronic obstructive pulmonary disease (COPD). Jour Func Vent Pulm 2013; 4 (12), 22-27.
18. S Duong-Quy, NN Le-Dong, AT Dinh-Xuan. Measurement of exhaled nitric oxide (NO) as a marker of airway inflammation. Journal of Functional Ventilation and Pulmonology 2013;4 (11), 16-22.
FIGURES - TABLES
REFERENCES
1. Loftus PA, Wise SK (2015), "Epidemiology and economic burden of asthma", International Forum of Allergy & Rhinology. 5(1), 7-10.
2. GINA (2018), Global Strategy for Asthma Management and Prevention.
3. Helen K. Reddel, Eric D. Bateman, Allan Becker (2015), "A summary of the new GINA strategy: a roadmap to asthma control", European Respiratory Journal. 46(3), 622-639.
4. GINA (2007), Global Strategy for Asthma Management and Prevention.
5. MD, Bethesda (2007), Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma, National Heart, Lung and Blood Institute US.
6. Grzelewska-Rzymowska IF, Mikołajczyk J, Kroczyńska-Bednarek J, Górski P (2015), "Association between asthma control test, pulmonary function tests and non-specific bronchial hyperresponsiveness in assessing the level of asthma control", Pneumonol Alergol Pol. 83(4), 266-274.
7. Nathan RA và các cộng sự. (2004), "Development of the asthma control test: a survey for assessing asthma control", The Journal of Allergy and Clinical Immunology. 113(1), 59-65.
8. Schatz M, Kosinski M, Yarlas AS, Hanlon J, Watson ME, Jhingran P (2009), "The minimally important difference of the Asthma Control Test", The Journal of Allergy and Clinical Immunology. 124(4), 719-723.e1.
9. Thomas M, Kay S, Pike J, Williams A, Rosenzweig JR, Hillyer EV, Price D (2009), "The Asthma Control Test (ACT) as a predictor of GINA guideline-defined asthma control: analysis of a multinational cross-sectional survey", Primary Care Respiratory Journal. 18(1), 41-49.
10. Waibel V, Ulmer H, Horak E (2012), "Assessing asthma control: symptom scores, GINA levels of asthma control, lung function, and exhaled nitric oxide", Pediatr Pulmonol 47(2), 113-118.
11. Ciprandi G, Cirillo I, Pasotti F, Ricciardolo FL. FEF25- 75: a marker for small airways and asthma control", Annals of Allergy, Asthma and Immunology2013;(3), 233-4.
12. E.Gibb, D. Kaplan, S.M. THyne, N.P. Ly (2012), "FEF25%-75% as a predictor of Asthma severity in children", B61 Pediatric Asthma, A6801.
13. H Dinh-Thi-Dieu, A Vo-Thi-Kim, H Tran-Van, T TangThi-Thao, S. Duong-Quy. Study of the beneficial role of exhaled nitric oxide in combination with GINA guidelines for titration of inhaled corticosteroids in children with asthma. Journal of Breath Research; 2020.
14. L Mansfield, S Duong-Quy, T Craig. Burden of Asthma and Role of 2.5 µg Tiotropium Respimat® as an AddOn Therapy: A Systematic Review of Phase 2/3 Trials. Advances in therapy,2019; 1-13.
15. S Duong-Quy. Clinical Utility Of The Exhaled Nitric Oxide (NO) Measurement With Portable Devices In The Management Of Allergic Airway Inflammation And Asthma. Journal of Asthma and Allergy2019; 12, 331.
16.T Ho-Ly-Minh, S Bui-Binh-Bao, S Duong-Quy. The meaning of sputum eosinophil in childhood asthma and its current application. Jour Func Vent Pulm 2018; 9 (26), 3-7.
17. T Hua-Huy, S Duong-Quy. Lung function testing in chronic obstructive pulmonary disease (COPD). Jour Func Vent Pulm 2013; 4 (12), 22-27.
18. S Duong-Quy, NN Le-Dong, AT Dinh-Xuan. Measurement of exhaled nitric oxide (NO) as a marker of airway inflammation. Jour Func Vent Pulm 2013;4 (11), 16-22.
ARTICLE INFO DOI: 10.12699/jfvpulm.10.30.2020.42 Conflict of Interest