
 English
English
 French
French
The satisfaction and adherence to inhaler devices among patients with chronic obstructive pulmonary disease and asthma at a tertiary hospital in Viet Nam
La satisfaction et l'adhésion aux dispositifs d'inhalation chez les patients atteints de maladie pulmonaire obstructive chronique et d'asthme dans un hpital tertiaire au Viet Nam
Hien Duy Thi1, Ha Pham Ngoc1, Giap Vu Van1,2
1: Respiratory Center- Bach Mai Hospital, Hanoi, Vietnam
2: Hanoi Medical University, Hanoi, Vietnam
Corresponding author:
A/Pr.Dr. Giap Vu Van, Hanoi Medical University, Hanoi, Vietnam.
E-mail: vuvangiap@hmu.edu.vn
ABSTRACT
Introduction. Satisfaction with the inhaler is an important determinant of treatment adherence in patients with chronic obstructive pulmonary disease (COPD) and asthma. Poor adherence to inhaled therapy is common in those patients. This study describes the level of satisfaction and adherence to inhaler devices among patients with COPD and asthma and determines the variables associated with high satisfaction and adherence.
Methods. A cross-sectional study of 260 Vietnamese patients (194 with COPD and 66 with asthma) was conducted. Satisfaction was assessed with the Feeling of Satisfaction with Inhaler (FSI-10) questionnaire. Adherence to inhaled therapy was assessed with the Test of Adherence to Inhaler (TAI).
Results. The study population was categorized according to a median FSI-10 score as high (59.6%) and low (40.4%) satisfaction with their inhaler. Educational level, diagnosis and the level of adherence were significantly associated with high inhaler satisfaction. The asthma group was significantly more satisfied with the inhaler (mean FSI-10 score: 43.4 (±0.5) vs. 40.2 (±0.4), p<0.001). Over half (59.6%) of the total participants were classified in the poor adherence group. In that, poor adherence group in COPD sample and asthma sample accounted for 63.9% and 50% respectively. Disease duration and time managed in Unit for Management of Asthma and COPD (UMAC) were significantly associated with the level of adherence.
Conclusions. The level of patient satisfaction with the inhaler was related to educational level, disease duration, and adherence. Disease duration, time managed in UMAC of the participant and number of inhalers using were associated with the level of adherence
KEYWORDS: COPD; Asthma; Patient satisfaction; Adherence.
RÉSUMÉ
Introduction. La satisfaction à l'égard de l'inhalateur est un déterminant important de l'observance du traitement chez les patients atteints de maladie pulmonaire obstructive chronique (MPOC) et d'asthme. Une mauvaise adhésion au traitement par inhalation est fréquente chez ces patients. Cette étude décrit le niveau de satisfaction et d'adhésion aux dispositifs d'inhalation chez les patients atteints de MPOC et d'asthme et détermine les variables associées à une satisfaction et à une adhésion élevées.
Méthodes. Une étude transversale de 260 patients vietnamiens (194 avec BPCO et 66 avec asthme) a été menée. La satisfaction a été évaluée à l'aide du questionnaire Sentiment de satisfaction avec l'inhalateur (FSI-10). L'adhésion au traitement par inhalation a été évaluée à l'aide du test d'adhésion à l'inhalateur (TAI).
Résultats. La population étudiée a été classée selon un score FSI-10 médian comme une satisfaction élevée (59,6 %) et faible (40,4 %) à l'égard de son inhalateur. Le niveau d'éducation, le diagnostic et le niveau d'observance étaient significativement associés à une satisfaction élevée de l'inhalateur. Le groupe asthmatique était significativement plus satisfait de l'inhalateur (score moyen FSI-10 : 43,4 (±0,5) contre 40,2 (±0,4), p<0,001). Plus de la moitié (59,6 %) du total des participants ont été classés dans le groupe de faible adhérence. En cela, le groupe de mauvaise adhérence dans l'échantillon de MPOC et l'échantillon d'asthme représentaient 63,9 % et 50 % respectivement. La durée de la maladie et le temps pris en charge dans l'Unité de gestion de l'asthme et de la BPCO (UMAC) étaient significativement associés au niveau d'adhésion.
Conclusion. Le niveau de satisfaction des patients vis-à-vis de l'inhalateur était lié au niveau d'éducation, à la durée de la maladie et à l'observance. La durée de la maladie, le temps pris en charge dans l'UMAC du participant et le nombre d'inhalateurs utilisant étaient associés au niveau d'observance.
MOTS CLÉS: BPCO; Asthme; Satisfaction des patients; Adhesion.
INTRODUCTION
Chronic Obstructive Pulmonary Disease (COPD) and asthma are chronic obstructive lung diseases that affect millions of patients and lead to a considerable burden to the health care system worldwide [1], [2], [3]. Based on current treatment guidelines, both disease asthma and COPD are treated with the maintenance of medication delivered daily by inhaler devices. Inhaled therapy is the cornerstone for treating COPD and asthma because of the advantages over oral tablet administration. It takes medication directly to the lungs at a lower dose with a rapid onset action [4] [5].
Despite the importance of inhaled therapy in the management of COPD and asthma, suboptimal adherence to inhaler therapy frequently occurs among COPD and asthma patients, resulting in poor disease control and increased morbidity and mortality [6], [7]. Some studies have shown that satisfaction with inhalers is an essential determinant of treatment adherence and disease control in such patients [8], [9]. Therefore, doctors should consider patient perspectives to the inhaler as a factor in appropriate inhaler selection for achieving optimal symptom control. Also, nurses, who are the main care provider and who manage patients long-term, should be encouraged to understand patient satisfaction with the inhaler [10].
This study aimed to describe the level of satisfaction and adherence to the inhaler devices among patients with COPD and asthma; determine the variables associated with high satisfaction and adherence.
METHODS
Study design and Participants
A cross-sectional study was conducted at the Unit for Management of Asthma and COPD (UMAC) Bach Mai Hospital, a tertiary referral hospital in Hanoi Vietnam from January 2021 to March 2021. Out of 260 patients (194 COPD and 66 asthma patients) were recruited in the study. Inclusion criteria for participants in the study were: (1) being at least 18 years old; (2) diagnosed with COPD (criteria of GOLD 2020) or asthma (criteria of GINA 2020); (3) being participated in COPD and asthma national management program; (4) being currently used at least one inhaler device for COPD and asthma treatment for at least last three months; and (5) agreeing to be participated in the study. We excluded participants that were inability to communicate.
Data collection and Outcome Assessment
We based on medical records to determine the eligibility of participants. Information about the history of the disease, prescription of inhalers at home was also collected. Face-to-face interviews were conducted to evaluate patient satisfaction and inhaler adherence by a survey questionnaire.
Patient satisfaction
The Feeling of Satisfaction with Inhaler (FSI-10) questionnaire used to evaluate patient satisfaction with their inhaler. FSI-10 was a useful tool to evaluate the level of satisfaction with inhaler devices of COPD and asthma patients [11]. It was a validated 10- item, self-completed questionnaire.
Patients answer each question with five response options on Likert scale ranging from 1 (hardly at all) to 5 (very). A total score ranged from 10 to 50 points. For this study, we calculated the median for the sample and then used this score as the cutoff value to differentiate between high and low satisfaction with the device.
Adherence to inhaler devices was assessed with the Test of Adherence to Inhalers (TAI) [12], a validated self-report instrument. There were two versions of this instrument: the TAI-10 and the TAI-12. The TAI-10 includes ten patient-rated items. The scoring range of each question is from 1 (worst adherence) to 5 (best adherence), so a total score ranges from 10 to 50. The level of patient adherence was classified as follow:
The TAI-12, which was fundamental rule to categorized patients in their type or pattern of nonadherence. The remaining two questions spend for healthcare professional taking care of the patients to evaluate patient understanding of the dosing schedule and/ or inhalation technique, with 1 or 2 points corresponding. Type or pattern of nonadherence was categorized as follows:
Items 1-5 scores < 25: "erratic non-adherence"
Items 6-10 scores < 25: "deliberate non-adherence"
Items 11-12 scores < 4: "ignorance non-adherence"
Statistical Analysis
Descriptive statistics were adopted to examine the sociodemographic and clinical characteristics of the study population. The results of analysis were described as means (standard deviation) or n (%), as appropriate.
Univariate analyses were used to determine the associated variables with patient satisfaction with the inhaler and adherence to inhaled therapy; and these were then entered into a multivariate logistic regression model.
We used Student's t-test for quantitative variables and the χ2 test for categorical variables. SPSS software version 22.0 was used to perform this statistical analysis and statistical significance was acknowledged at a p-value of less than 0.05.
Ethical approval
The participants were explained clearly about the purpose of this study, and they were willing to volunteer and orally agree to participate. Person who participates in this study was not under any pressure. The participants were explained the right to withdraw at any time they want without regard to any negative consequences, and they understand that collecting the data was only for study purposes. The result of the research was aimed exclusively at improving clinical practice, not for any other purpose. Patients' information was kept confidential. All information and comments were encoded without reveal names and no personal information was included.
RESULTS
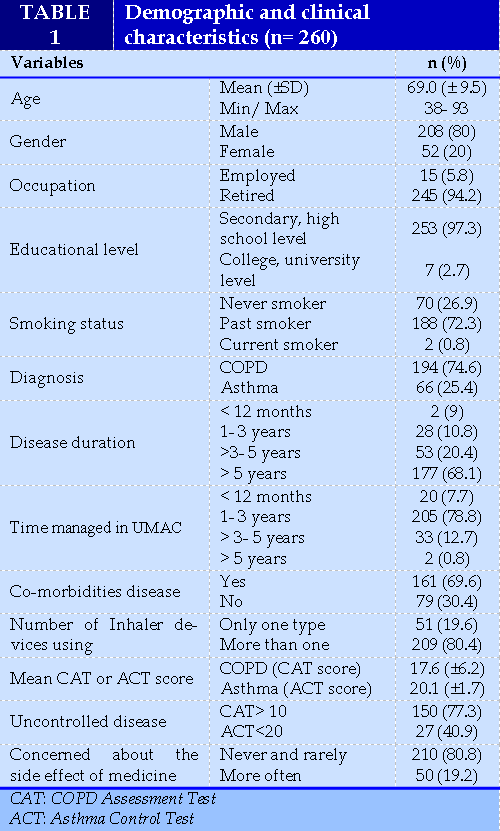
Of 260 patients, their ages ranged from 38 years old to 93 years old, with the mean age is 69.0 ± 9.5. Most of the participants (80%) were male. Many of them were retired and only 5.8% of subjects are employed. Almost of participants had secondary, high school levels (97.3%). 72.3% of them were past smokers but had quit since the diagnosis of lung disease and 26.9% of participants were nonsmokers. (TABLE 1)
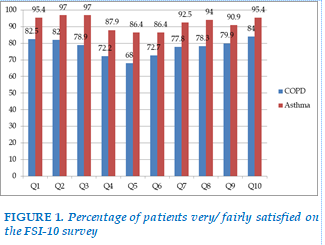
(FIGURE 1) The satisfactory result was obtained with inhaler devices among COPD and asthma patients showed that the total (median) on the FSI-10 was 40.0 points and ranged from 23 to 50 points. Based on a cutoff value of FSI-10 ≥ 40, satisfaction was considered high in 155 patients (59.6%) and low in 105 patients (40.4%).
Specifically, the asthma group was significantly more satisfied with inhaler devices compared to the COPD group (mean FSI-10 score: 43.4 vs. 40.2, p< 0.001). The difference in the proportion of very and fairly satisfied patients between the asthma group and COPD group was depicted in figure 1. It indicated the percentage of patients in each group who were very or fairly satisfied on each of the ten items on the FSI-10 survey. Over 70% of patients in asthma and COPD groups were very or fairly satisfied with the inhaler (except item 5) and the proportion of very or fairly satisfied patients was higher in the asthma group .
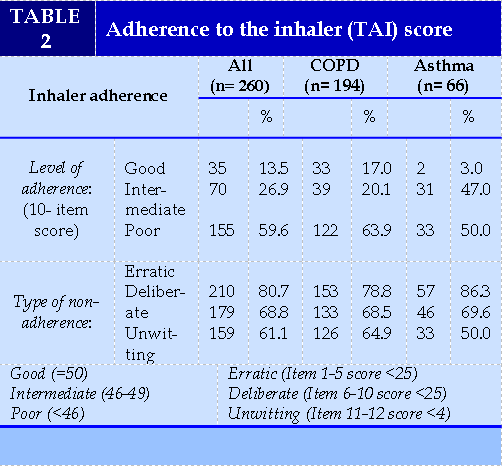
A univariate analysis was performed to identify the variables significantly associated (p <0.05) with inhaler satisfaction (FSI-10 ≥ 40). The result showed (TABLE 2)
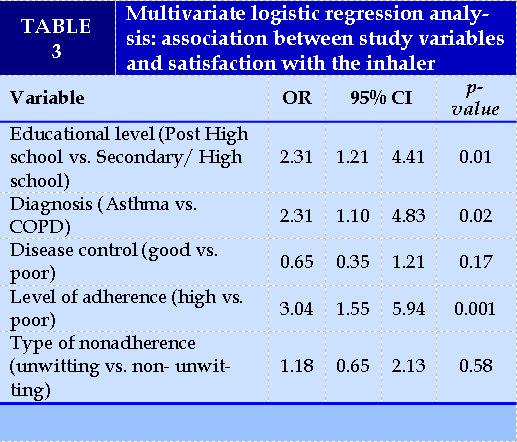
(TABLE 3) that variables: educational level, diagnosis, disease control, level of adherence and type of nonadherence are significantly associated with the level of inhaler satisfaction. On the multivariate (Table 3) shows that three variable was significantly associated with high satisfaction with the inhaler (FSI-10 ≥ 40): educational level, diagnosis, and level of adherence. Patients who obtained a higher level of education (post-high school) were more satisfied with the inhaler (with OR= 2.31, 95% CI (1.21-4.41), p= 0.01). Asthma patients were more satisfied with the inhaler than COPD patients. The odd value of the asthma group was 2.3 times higher than the COPD group (95% CI (1.1-4.83), p= 0.02). High adherence patients were more satisfied with the inhaler (with OR= 3.04, 95% CI (0.16-5.94), p= 0.001).
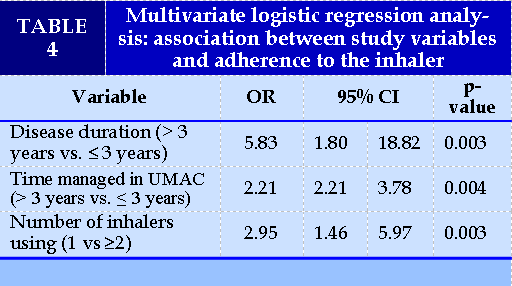
On the univariate analysis and multivariate analysis (Table 4), three variable was significantly associated with high adherence to the inhaler (TAI ≥ 46): Disease duration, time managed in UMAC, number of inhalers using. Patients with a disease duration of more than three years were more compliant (OR= 5.83; 95% CI (1.80- 18.82), p= 0.003), patients with time managed in UMAC were more compliant (OR= 2.21; 95% CI (2.21- 3.78), p= 0.004), patients using 1 inhaler were more compliant (OR= 2.95; 95% CI (1.46- 5.97), p= 0.003.
DISCUSSIONS
This research was designed to assess the inhaler satisfaction and adherence to inhaled therapy among COPD and asthma patients. Patient satisfaction with their inhaler devices has been increasingly concerned recently. Evidence linking patient satisfaction with patient adherence and improve clinical outcomes was explored [13].
Patients satisfied and preferred with their using inhalers are more likely to obtain a greater degree of satisfaction with therapy. Satisfaction with the device, although it has been considered like general satisfaction with treatment, it focuses on the usability of the device. Therefore, we chose the FSI-10 to evaluate satisfaction with the inhalers. FSI-10 questionnaire quantifies the various aspects of inhaler devices that patients concerned about when using, such as ease of use and portability.
In this study, the FSI-10 in Vietnamese was used and an interviewer also interpreted to help patients who felt difficult to understand and chose their answers. The median of the total FSI-10 score was 40, with a range from 23 (lowest satisfaction) to 50 (highest satisfaction). Thus, the FSI-10 variable categorized 155 patients (59.6%) with high satisfaction with their current inhaler maintenance (FSI-10 score ≥ 40) and 105 patients (40.4%) with low satisfaction with their current inhaler maintenance (FSI-10 <40). Two studies of Vincete Plaza et al. that were designed to evaluate the patient satisfaction with the inhaler among COPD and asthma indicated a median of the total FSI-10 score was higher than the result in our study. In particular, Vincete Plaza et al. study (2008) showed that a median FSI-10 score was 43, with 49.4% of patients were high satisfaction and 50.6% were low satisfaction. Thus, a median FSI-10 score in this study was small lower and maybe led to higher satisfaction than the previous studies. Determining patient satisfaction with the inhaler may help healthcare professionals understand and explore whether using an inhaler is suitable for patients. The prescribing physician needs to tailor the inhaler device's selection to the individual patient, considering their need, functional ability, and the complexity of the medication regimen.
The result in this study also showed that asthma patients tended to express higher feeling satisfaction with the inhaler devices than COPD patients (mean FSI-10 score: 43.4 (±0.5) vs. 40.2 (±0.4), p< 0.001). Vincete Plaza et el. study (2016) [14] also indicated that the asthma group was significantly more satisfied with the inhaler (mean FSI-10 score: 44.1 (±6.5) vs. 42.0 (±7.0), p < 0.001). In addition, a real-world design to evaluate satisfaction with a specific inhaler found that a higher percentage of patients with asthma were very satisfied with the device (52.6%) than those with COPD (33.4%) [15]. It is essential to recognize the perhaps subtle differences between what patients with asthma and COPD are looking for in an inhaler device. Our study explored those three variables: educational level, diagnosis, and level of adherence, were significantly associated with higher satisfaction. It suggests that patients with higher educational level, asthma diagnosis and good adherence were higher satisfaction with the inhaler. This finding was a partly consistent with the results of studies conducted previously by Vincete Plaza et al. In those studies younger age, disease control, previous inhaler training, absence of unwitting and treatment adherence were independently and significantly associated with higher satisfaction with the inhaler (FSI-10) [14], [16].
Poor adherence in patients with COPD and asthma was a significant concern. In this study, we used the specific tool, the Test of Adherence to Inhalers (TAI), to assess the level of adherence and type of nonadherence. The results of this survey indicated that over half (59.6%) of the total participants were classified in the poor adherence group, 26.9% of participants were intermediate adherence and 13.5% of participants were good adherence. The proportion of good adherence was lower than the previous study in other clinical settings such as in Australia (37-42%) [17], Hungary (58.2%) [18] and seven Latin American countries ( 54.1%) [19]. A study was conducted in COPD patients in the same clinical room at Bach Mai Hospital to evaluate adherence to inhalers by the MMAS-8 scale explored that 37.9% of patients were good adherence [20]. In our study, the prevalence of each nonadherence pattern "erratic", "deliberate", "unwitting" were 80.7%, 68.8% and 61.1%, respectively, for the total sample, which was considerably higher than previous studies. A study in Spain, which found that the prevalence of "erratic", "deliberate", "unwitting" types were 66.8%, 47.2% and 31.2%, respectively [21]. Another study by Ngo Quy Chau et al. was conducted in COPD patients at Bach Mai Hospital [22] showed the rate of nonadherence pattern was: "erratic" (58.6%), "deliberate" (55.7%) and "unwitting" (77.1%). In our study, the "erratic non-adherence" accounted for the highest proportion; the main reason for this type of nonadherence was patient forgetfulness; followed by "deliberate non-adherence", which occurred when patients were intentional. "Unwitting non-adherence" due to insufficient understanding of the dosing schedule and/or poor inhalation technique was the lowest proportion. These results suggest that to enhance the inhaler adherence of patients, we should educate them on the importance of treatment compliance and carefully instruct them on medication regimens and inhaler techniques. Few factors were reliably linked with treatment adherence. In a meta-analysis of adherence research on chronic disease for 50 years [18], it was shown that higher levels of adherence were allied to more circumscribed regimens (medication use versus health behavior change) and to more significant patient resources (social and emotional support). A study in Ethiopia [23] evaluate inhaler adherence among patients with asthma indicated that lack of education about the proper use of inhalational anti-asthmatic medications, polypharmacy and co-morbidities were statistically significant factors associated with nonadherence.
Thu Nguyen Hoai's study found that older age and feeling hesitant to perform inhaler technique were associated with inhaler adherence [20]. In this study, we also analyzed the association of co-morbidities, number of inhalers using, disease control, disease duration, time managed in UMAC, concern about side effect of medication with the level of adherence; the result showed the number of inhaler using, disease duration, time managed in UMAC were associated with adherence on an univariate analysis and the multivariate analysis was conducted and explored that three variables were significantly associated with the level of adherence. Patients with disease duration or time managed in UMAC more than 3 years were more compliant (OR= 5.83; 95% CI (1.80- 18.82), p= 0.003 and OR= 2.21; 95% CI (2.21- 3.78), p= 0.004 respectively) and patients using 1 inhaler were more compliant (OR= 2.95; 95% CI (1.46- 5.97), p= 0.003). It suggests that a long time of suffering disease, participating in program, patients were higher inhaler adherence and patients using 1 inhaler were higher adherence.
Some findings of our study require more investigation to get an insight assessment. Satisfaction was higher in higher educational level, asthma diagnosis and the level of adherence. Other studies found that disease control and inhaler training also were associated with higher satisfaction. In our study, we explored the disease duration, time managed in UMAC and number of inhalers using were significantly associated with the level of adherence.
A potential limitation of our study was that adherence was reported by patients, which might have led to recall bias as well as an over or under-estimation of medication utilization. However, we could have chosen other methods to assess adherence. Direct methods, including the measurement of drug plasma levels or the use of electronic devices, are more sensitive but also more complicated and expensive. Among indirect methods, validated self-reported questionnaires or scales are easy to administer. In addition, the results might not reflect the pattern of nonadherence and inhaler satisfaction in other settings.
CONCLUSIONS
High patient satisfaction with the inhaler was related to educational level, disease duration, and level of adherence. Poor adherence to inhaled therapy was common among patients with COPD and asthma. Furthermore, disease duration, time managed in UMAC and number of inhalers using were significantly associated with the level of adherence. Give associated factors of patient satisfaction and adherence to inhaled therapy; these findings underscore the need for better training and more active monitoring of inhalation using to improve satisfaction with the inhaler, adherence to inhaled therapy and get a better clinical outcome.
Acknowledgments
Our thanks to Respiratory Center of Bach Mai Hospital that gave permission and support in conducting this research. We are grateful to all patients at COPD and asthma Management Room who gave us their time to participate in this study.
Conflicts of Interest
No competing interest were disclosed.
REEFRENCES
| 1. Bahadori K., Doyle-Waters M., Marra C., et al. (2009). Economic burden of asthma: A systematic review. BMC Pulm Med, 9, 24. |
| 2. GBD 2015 Chronic Respiratory Disease Collaborators (2017). Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med, 5(9), 691–706. |
| 3. Riccioni G., D’Orazio N., Ilio C.D., et al. (2004). Quality of Life and Clinical Symptoms in Asthmatic Subjects. J Asthma, 41(1), 85–89. |
| 4. Yawn B.P., Mintz M.L., and Doherty D.E. (2021). GOLD in Practice: Chronic Obstructive Pulmonary Disease Treatment and Management in the Primary Care Setting. Int J Chron Obstruct Pulmon Dis, 16, 289–299. |
| 5. Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2020.www.ginasthma.org/ Date last accessed: May 25, 2020. Date last updated: 2020. |
| 6. Plaza V., López-Viña A., Entrenas L.M., et al. (2016). Differences in Adherence and Non-Adherence Behaviour Patterns to Inhaler Devices Between COPD and Asthma Patients. COPD J Chronic Obstr Pulm Dis, 13(5), 547–554. |
| 7. Toy E.L., Beaulieu N.U., McHale J.M., et al. (2011). Treatment of COPD: Relationships between daily dosing frequency, adherence, resource use, and costs. Respir Med, 105(3), 435–441. |
| 8. Small M., Anderson P., Vickers A., et al. (2011). Importance of inhaler-device satisfaction in asthma treatment: Real-world observations of physician-observed compliance and clinical/patient-reported outcomes. Adv Ther, 28(3), 202–212. |
| 9. Mäkelä M.J., Backer V., Hedegaard M., et al. (2013). Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med, 107(10), 1481–1490. |
| 10. Scullion J. (2018). The Nurse Practitioners’ Perspective on Inhaler Education in Asthma and Chronic Obstructive Pulmonary Disease. Can Respir J, 2018. |
| 11. Perpiñá Tordera M., Viejo J.L., Sanchis J., et al. (2008). [Assessment of patient satisfaction and preferences with inhalers in asthma with the FSI-10 Questionnaire]. Arch Bronconeumol, 44(7), 346–352. |
| 12. Plaza V., Fernández-Rodríguez C., Melero C., et al. (2016). Validation of the “Test of the Adherence to Inhalers” (TAI) for Asthma and COPD Patients. J Aerosol Med Pulm Drug Deliv, 29(2), 142–152. |
| 13. Price D., Harrow B., Small M., et al. (2015). Establishing the relationship of inhaler satisfaction, treatment adherence, and patient outcomes: A prospective, real-world, cross-sectional survey of US adult asthma patients and physicians. World Allergy Organ J, 8. |
| 14. Plaza V., Giner J., Curto E., et al. (2020). Determinants and Differences in Satisfaction with the Inhaler Among Patients with Asthma or COPD. J Allergy Clin Immunol Pract, 8(2), 645–653. |
| 15. Dias-Barbosa C., Balp M.-M., Kulich K., et al. (2012). A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence, 6, 39–48. |
| 16. Plaza V., Giner J., Calle M., et al. (2018). Impact of patient satisfaction with his or her inhaler on adherence and asthma control. Allergy Asthma Proc, 39(6), 437–444. |
| 17. Sriram K.B. and Percival M. (2016). Suboptimal inhaler medication adherence and incorrect technique are common among chronic obstructive pulmonary disease patients. Chron Respir Dis, 13(1), 13–22. |
| 18. Ágh T., Inotai A., and Mészáros Á. (2011). Factors associated with medication adherence in patients with chronic obstructive pulmonary disease. Respir Int Rev Thorac Dis, 82(4), 328–334. |
| 19. Montes de Oca M., Menezes A., Wehrmeister F.C., et al. (2017). Adherence to inhaled therapies of COPD patients from seven Latin American countries: The LASSYC study. PloS One, 12(11), e0186777. |
| 20. Nguyen Hoai Thu (2016), Assessment of the adherence treatment and inhaler technique in COPD patients at Bach Mai hospital, Thesis of Master of Science of Pharmacy, Hanoi University of Pharmacy. |
| 21. V P., A L.-V., Lm E., et al. (2016). Differences in Adherence and Non-Adherence Behaviour Patterns to Inhaler Devices Between COPD and Asthma Patients. COPD, 13(5). |
| 22. Ngo C., Phan D., Vu G., et al. (2019). Inhaler Technique and Adherence to Inhaled Medications among Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease in Vietnam. Int J Environ Res Public Health, 16. |
| 23. Ayele A.A. and Tegegn H.G. (2017). Non adherence to inhalational medications and associated factors among patients with asthma in a referral hospital in Ethiopia, using validated tool TAI. Asthma Res Pract, 3, 7. |
FIGURE - TABLES
REEFRENCES
| 1. Bahadori K., Doyle-Waters M., Marra C., et al. (2009). Economic burden of asthma: A systematic review. BMC Pulm Med, 9, 24. |
| 2. GBD 2015 Chronic Respiratory Disease Collaborators (2017). Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med, 5(9), 691–706. |
| 3. Riccioni G., D’Orazio N., Ilio C.D., et al. (2004). Quality of Life and Clinical Symptoms in Asthmatic Subjects. J Asthma, 41(1), 85–89. |
| 4. Yawn B.P., Mintz M.L., and Doherty D.E. (2021). GOLD in Practice: Chronic Obstructive Pulmonary Disease Treatment and Management in the Primary Care Setting. Int J Chron Obstruct Pulmon Dis, 16, 289–299. |
| 5. Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2020.www.ginasthma.org/ Date last accessed: May 25, 2020. Date last updated: 2020. |
| 6. Plaza V., López-Viña A., Entrenas L.M., et al. (2016). Differences in Adherence and Non-Adherence Behaviour Patterns to Inhaler Devices Between COPD and Asthma Patients. COPD J Chronic Obstr Pulm Dis, 13(5), 547–554. |
| 7. Toy E.L., Beaulieu N.U., McHale J.M., et al. (2011). Treatment of COPD: Relationships between daily dosing frequency, adherence, resource use, and costs. Respir Med, 105(3), 435–441. |
| 8. Small M., Anderson P., Vickers A., et al. (2011). Importance of inhaler-device satisfaction in asthma treatment: Real-world observations of physician-observed compliance and clinical/patient-reported outcomes. Adv Ther, 28(3), 202–212. |
| 9. Mäkelä M.J., Backer V., Hedegaard M., et al. (2013). Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med, 107(10), 1481–1490. |
| 10. Scullion J. (2018). The Nurse Practitioners’ Perspective on Inhaler Education in Asthma and Chronic Obstructive Pulmonary Disease. Can Respir J, 2018. |
| 11. Perpiñá Tordera M., Viejo J.L., Sanchis J., et al. (2008). [Assessment of patient satisfaction and preferences with inhalers in asthma with the FSI-10 Questionnaire]. Arch Bronconeumol, 44(7), 346–352. |
| 12. Plaza V., Fernández-Rodríguez C., Melero C., et al. (2016). Validation of the “Test of the Adherence to Inhalers” (TAI) for Asthma and COPD Patients. J Aerosol Med Pulm Drug Deliv, 29(2), 142–152. |
| 13. Price D., Harrow B., Small M., et al. (2015). Establishing the relationship of inhaler satisfaction, treatment adherence, and patient outcomes: A prospective, real-world, cross-sectional survey of US adult asthma patients and physicians. World Allergy Organ J, 8. |
| 14. Plaza V., Giner J., Curto E., et al. (2020). Determinants and Differences in Satisfaction with the Inhaler Among Patients with Asthma or COPD. J Allergy Clin Immunol Pract, 8(2), 645–653. |
| 15. Dias-Barbosa C., Balp M.-M., Kulich K., et al. (2012). A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence, 6, 39–48. |
| 16. Plaza V., Giner J., Calle M., et al. (2018). Impact of patient satisfaction with his or her inhaler on adherence and asthma control. Allergy Asthma Proc, 39(6), 437–444. |
| 17. Sriram K.B. and Percival M. (2016). Suboptimal inhaler medication adherence and incorrect technique are common among chronic obstructive pulmonary disease patients. Chron Respir Dis, 13(1), 13–22. |
| 18. Ágh T., Inotai A., and Mészáros Á. (2011). Factors associated with medication adherence in patients with chronic obstructive pulmonary disease. Respir Int Rev Thorac Dis, 82(4), 328–334. |
| 19. Montes de Oca M., Menezes A., Wehrmeister F.C., et al. (2017). Adherence to inhaled therapies of COPD patients from seven Latin American countries: The LASSYC study. PloS One, 12(11), e0186777. |
| 20. Nguyen Hoai Thu (2016), Assessment of the adherence treatment and inhaler technique in COPD patients at Bach Mai hospital, Thesis of Master of Science of Pharmacy, Hanoi University of Pharmacy. |
| 21. V P., A L.-V., Lm E., et al. (2016). Differences in Adherence and Non-Adherence Behaviour Patterns to Inhaler Devices Between COPD and Asthma Patients. COPD, 13(5). |
| 22. Ngo C., Phan D., Vu G., et al. (2019). Inhaler Technique and Adherence to Inhaled Medications among Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease in Vietnam. Int J Environ Res Public Health, 16. |
| 23. Ayele A.A. and Tegegn H.G. (2017). Non adherence to inhalational medications and associated factors among patients with asthma in a referral hospital in Ethiopia, using validated tool TAI. Asthma Res Pract, 3, 7. |
ARTICLE INFO DOI: 10.12699/jfvpulm.12.38.2021.1
Conflict of Interest
Non
Date of manuscript receiving
25/02/2021
Date of publication after correction
25/08/2021
Article citation
Duy Thi H , Pham Ngoc H, Vu Van G. The satisfaction and adherence to inhaler devices among patients with chronic obstructive pulmonary disease and asthma at a tertiary hospital in Viet Nam. J Func Vent Pulm 2021;38(12):1-7