
 English
English
 French
French
CT findings at admission to traditional wards for COVID-19 infection are independently associated with severe outcome
Les résultats de la tomodensitométrie à l'admission dans les services traditionnels pour une infection au COVID-19 sont indépendamment associés à une issue grave
Bilfeld1, M. Lafaurie2, A. Sommet3, J. Monsinjeon1, F. Lafourcade1, F. Lapegue1, H. Chiavassa1, H. Basselerie1, S. Collot4, H. Rousseau4, N. Sans1, GM. Blondel5, G. Moulis2
1: Service d’imagerie, CHU Toulouse-Purpan, place du docteur Baylac, 31059 Toulouse Cedex 9, France
2: Service de Médecine Interne, CHU Toulouse-Purpan, place du docteur Baylac, 31059 Toulouse Cedex 9, France
3: Service de Pharmacologie clinique, Faculté de Médecine, 37 allées Jules Guesde, 31000 Toulouse
4: .Service d’imagerie, CHU Toulouse-Rangueil, 1 Avenue du Professeur Jean Poulhès, 31059 Toulouse Cedex 9, France
5: Service de Maladie Infectieuse et Tropicale, CHU Toulouse-Purpan, place du docteur Baylac, 31059 Toulouse Cedex 9, France
Corresponding author: Marie Faruch Bilfeld. Service de Radiologie. CHU Toulouse-Purpan, Place du Docteur Baylac, 31059 Toulouse Cedex 9, France.
E-mail: faruch.m@chu-toulouse.fr
ABSTRACT
Purpose. To evaluate the association of chest computed tomography (CT) findings at admission to traditional wards for COVID-19 with unfavorable outcome. Material and methods.We selected the patients included in the Covid-Clinic-Toul (the cohort of patients hospitalized for Covid-19 at Toulouse University hospital, south of France) up to April 20, 2020 with a SARS-CoV-2 infection proven by reverse transcriptase polymerase chain reaction, CT performed at admission and hospitalized in traditional wards. The outcome was admission to intensive care unit, need of mechanical ventilation or death occurring at Day14 after admission. We assessed the association of several CT findings with the outcome. Analyses were adjusted for clinical and biological variables that impact COVID-19 severity. Results. Of the 201 included patients, 69 patients (34.3%) met outcome criteria. In the multivariate model, extension of ground-glass opacities ≥50% on CT-scan performed at admission was the radiologic sign the most strongly associated with poor outcome (OR: 3.52; 95% CI: 1.42-8.75). The predominance of intralobular crazy paving (OR: 2.19; 95% CI: 0.91-5.28), vascular thickening (OR: 2.10; 95% CI: 0.84-5.22) and at a lesser extent pleural thickening (OR: 1.51; 95% CI: 0.55-4.13) were also associated with poor outcome. Conclusion. CT-scan helps in identifying COVID-19 patients at risk of poor outcome.
KEYWORDS: COVID-19; CT-scan; Prognosis.
RÉSUMÉ
Introduction. Évaluer l'association des résultats de la tomodensitométrie (TDM) thoracique à l'admission dans les services traditionnels pour COVID-19 avec un résultat défavorable. Matériel et méthodes. Nous avons sélectionné les patients inclus dans la Covid-Clinic-Toul (cohorte de patients hospitalisés pour Covid-19 au CHU de Toulouse) jusqu'au 20 avril 2020 avec une infection avérée au SARS-CoV-2 par amplification en chaîne par polymérase transcriptase inverse, scanner réalisé à l'admission et hospitalisé en service traditionnel. Le résultat était l'admission en unité de soins intensifs, le besoin d'une ventilation mécanique ou le décès survenu au jour 14 après l'admission. Nous avons évalué l'association de plusieurs résultats CT avec le résultat. Les analyses ont été ajustées pour les variables cliniques et biologiques qui ont un impact sur la gravité du COVID-19. Résultats. Sur les 201 patients inclus, 69 patients (34,3 %) répondaient aux critères de résultat. Dans le modèle multivarié, l'extension des opacités en verre dépoli ≥ 50 % au scanner réalisé à l'admission était le signe radiologique le plus fortement associé à un mauvais pronostic (OR : 3,52 ; IC 95 % : 1,42-8,75). La prédominance du pavage fou intralobulaire (OR : 2,19 ; IC 95 % : 0,91-5,28), de l'épaississement vasculaire (OR : 2,10 ; IC 95 % : 0,84-5,22) et dans une moindre mesure de l'épaississement pleural (OR : 1,51 ; IC 95 % : 0,55-4,13) étaient également associés à de mauvais résultats. Conclusion. La tomodensitométrie aide à identifier les patients COVID-19 à risque de mauvais résultats.
MOTS CLÉS: COVID-19; CT-scan; Pronostic.
INTRODUCTION
The outbreak of coronavirus disease 2019 (COVID-19) originated in Wuhan, China started in December 2019. The disease quickly rapidly invaded the world affecting millions of people and becoming a global health emergency [1].
With the gradual recognition of COVID-19, professional consensus, guidelines, and criteria were steadily established with the aim of preventing transmission and facilitating diagnosis and treatment. From the recently published literature, CT plays a central role in the diagnosis and management of COVID-19 pneumonia [2]. Currently, for some patients with mild clinical symptoms, CT examination is recommended for the detection of early diagnosis, evaluation of disease severity and of disease progression [3,4]. The predominant CT features of COVID-19 pneumonia are multiple ground-glass opacities (GGO) with or without consolidation and with both lungs, multiple lobes and especially the lower lobe affected [5]. Other CT findings included inter lobularseptal thickening, bronchiectasis, pleural thickening, and subpleural involvement; pleural effusion and lymphadenopathy were less common. The extent of CT abnormalities increases rapidly after the onset of symptoms, and peaks about 6-11 days after [6]. An increase in numbers, extent, and density of GGOs on CT indicate disease progression [7].
Currently, some CT signs are known to be markers of poor prognosis in patients admitted to intensive care units (ICU), but few have explored prognostic factors in patients not admitted to ICU independently of other clinical and biological variables [8–11].
Consequently, we aimed to assess the association of chest computed tomography (CT) findings at admission with unfavorable outcome at Day14 after admission in the setting of patients hospitalized in traditional wards for COVID-19.
METHODS
Study design and participants
We conducted a cohort study within the Covid-clinic-Toul cohort. This cohort records data about all patients hospitalized for SARS-CoV-2 at Toulouse University hospital. Patients transferred from another hospital were excluded. First patients (from March 11 to April 1) were retrospectively included and data from patients hospitalized on April 1 and thereafter were prospectively collected. All patients, or their representatives for those not able to understand the purpose of the study, were informed by a letter given at admission to hospital and/or sent to their place of residency. This cohort has been approved by institutional review board (n°RnIPH 2020-31), in accordance with the French data protection authority (MR004, Commission Nationale de l’Informatique et des Libertés, CNIL).
In the present study, we selected the patients included in the Covid-Clinic-Toul up to April 20, 2020 with a SARS-CoV-2 infection proven by reverse transcriptase polymerase chain reaction (RT-PCR), chest computed tomography (CT) scan performed at admission and hospitalized in traditional wards at day 1 of admission.
CT-scan
CT-scans were performed at admission to hospital (during the first 24 hours). They were retrospectively reviewed by two investigators (MF and JM). Discrepancies were solved by consensus. All CT acquisitions were obtained with the patients in supine position during end-inspiration without contrast medium injection. CT were performed on a 128-slice CT (GE Revolution EVO 64 Slice CT Scanner, GE Medical Systems, Milwaukee, WI, USA). The following technical parameters were used: tube voltage: 120 kV; tube current modulation 100-250 mAs; spiral pitch factor: 0.98; collimation width: 0.625. Reconstructions were made with convolution kernel BONEPLUS at a slice thickness of 1.25 mm.
The following patterns were assessed: extension of GGOs, categorized as mild/moderate (<50% of lung surface) or severe/critical (³50%); presence vs. absence of subpleural curvilinear line, presence vs. absence of nodular parenchyma consolidation, presence vs. absence of intralobular crazy paving pattern, presence vs. absence of pleural thickening, presence vs. absence of vascular thickening, presence of central lesions vs. peripheral lesions only, presence vs. absence of pleural effusion, topography of lesions (anomaly of superior or middle lobes vs. inferior lobes only), presence vs. absence mediastinal lymphadenopathy, and predominant sign among the following: ground-glass opacities, subpleural curvilinear line, nodular parenchyma consolidation, intralobular crazy paving, pleural thickening and vascular thickening.
Outcome
The outcome was composite, including admission to ICU, need of mechanical ventilation and death occurring during the 14 days after admission to hospital.
Covariables
Covariables, measured on the day of admission, were the age (categorized by <65 and ³65 years), sex, body mass index ³25 vs. <25 kg/m², presence vs. absence of comorbidities (among: arterial hypertension, cardiovascular disease, cerebrovascular
disease, diabetes mellitus, cancer, chronic lung disease, chronic kidney disease, chronic liver disease, immunosuppression), oxygen saturation £92% or need of oxygen therapy, respiratory rate >22/minute, protein C-reactive level >5 mg/dL, platelet count < 100 x 109/L and lymphocyte count <0.9 x 109/L.
Statistical analysis
Continuous variables were expressed as mean and standard deviation (SD) or median and interquartile range (IQR) depending on their distribution; categorical variables were presented by numbers and percentages.
We assessed the link between each variable and outcome occurrence by univariate logistic regression models. The variables with a p-value <0.25 were included in a multivariate model.
Missing values of the selected variables were handled by multiple imputation (n=5 imputations by missing value). Results are expressed using odds ratios (ORs) and their 95% confidence intervals (CIs). All statistical analyses were carried out using SAS V9.4TM software (SAS institute, Cary, NC, USA).
RESULTS
Patients’ characteristics (whole population)
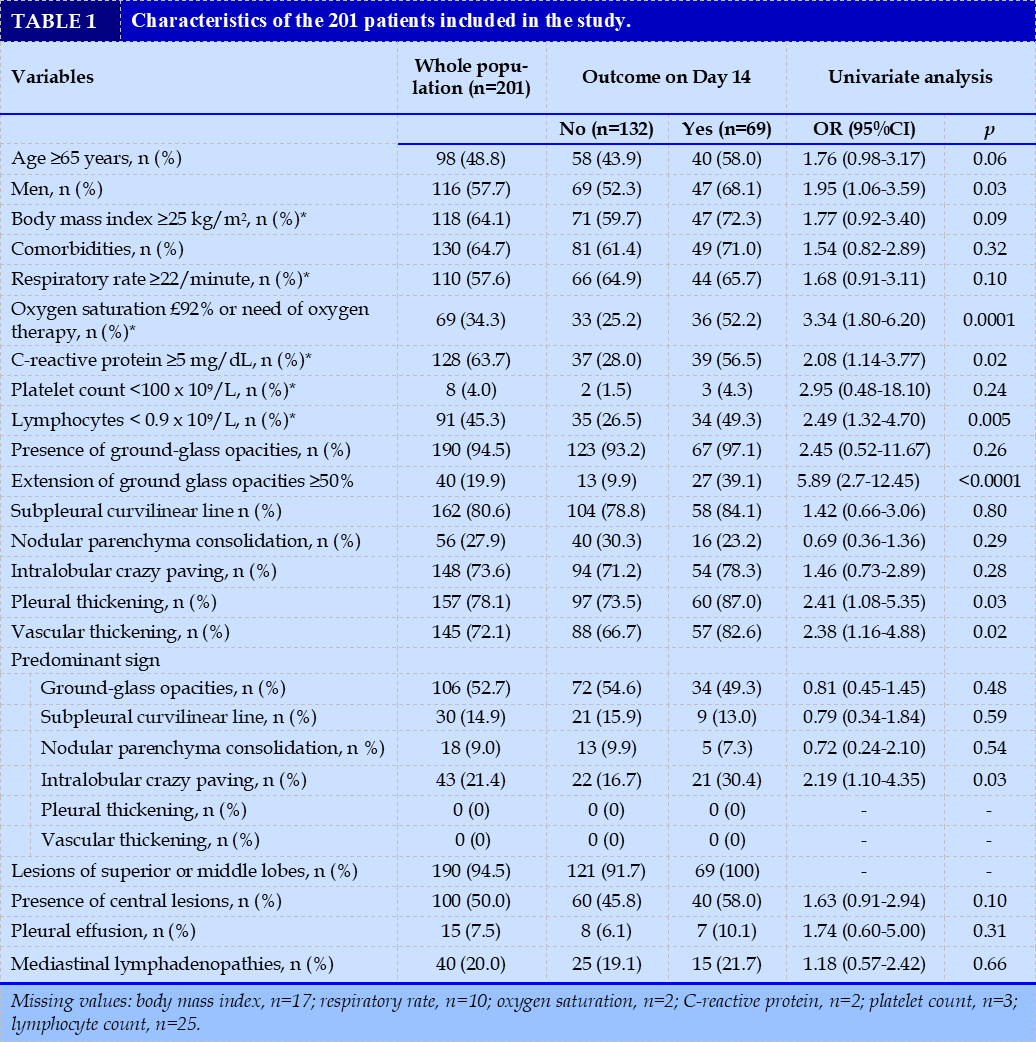
Among 263 patients included in the Covid-clinic-Toul cohort, 201 were not hospitalized in ICU on the first day of admission to hospital and were included in the present study. Patients’ characteristics are presented in Table 1. The median age was 64 years (IQR: 53-76), and 116 patients (57.7%) were men. The median duration of symptoms at admission was 7 days (IQR: 4-10).
Outcome
Of the 201 patients, 69 patients (34.3%) met outcome criteria at Day 14 after admission to hospital. Thirty-two needed mechanical ventilation and 14 died.
Comparison of patients who met outcome criteria and other patients
The results of univariate comparisons are indicated in Table 1. Patients who achieved the composite outcome at Day 14 were older (58.0% ≥65 years vs. 43.9%), more frequently men (68.1% vs. 52.3%), had more frequently an oxygen saturation £92% or a need of oxygen therapy at admission (52.2% vs. 25.2%), C-reactive level >5 mg/dL (56.5% vs. 28.0%), and lymphopenia (49.3% vs. 26.5%). In univariate analyses, an extension of GGOs ≥50% on CT-scan performed at admission was highly associated with a worse prognosis (OR: 5.89; 95% CI: 2.78-12.45). The other CT-scan signs associated with outcome occurrence were: pleural thickening (OR: 2.41; 95% CI: 1.08-5.35), vascular thickening (OR: 2.38; 95% CI: 1.16-4.88) and the predominance of intralobular consolidation/crazy paving (OR: 2.19; 95% CI: 1.10-4.35).
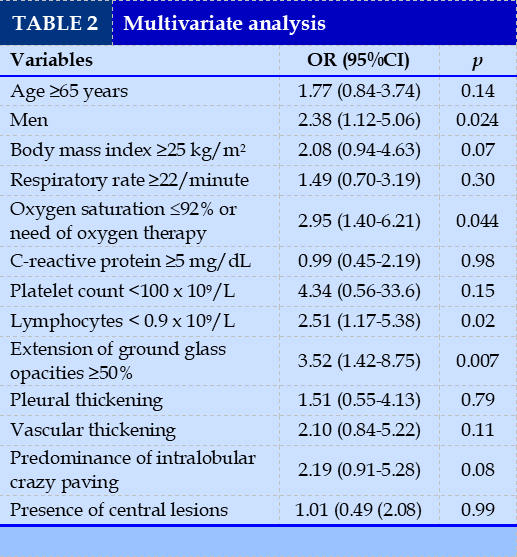
Multivariate model
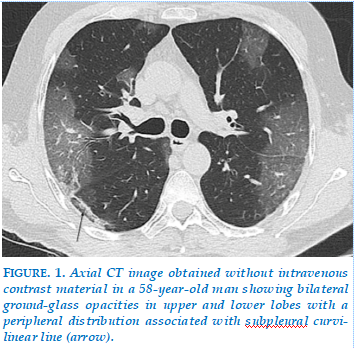
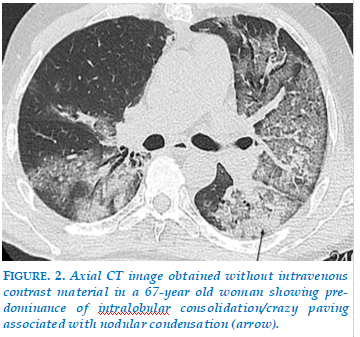
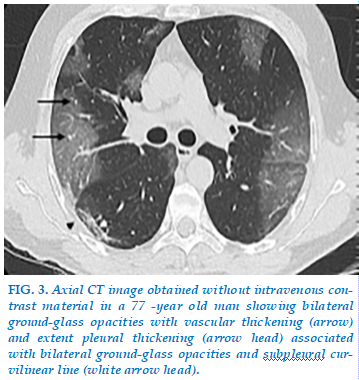
Results of the multivariate model are indicated in Table 2. The extension of GGOs ≥50% on CT-scan performed at admission (Fig. 1) was the radiologic sign the most strongly associated with poor outcome (OR: 3.52; 95% CI: 1.42-8.75). The predominance of intralobular consolidation/crazy paving (OR: 2.19; 95% CI: 0.91-5.28) (Fig. 2), vascular thickening (OR: 2.10; 95% CI: 0.84-5.22) and at a lesser extent pleural thickening (OR: 1.51; 95% CI: 0.55-4.13) (Fig. 3) were also associated with poor outcome (OR>1.50), albeit not reaching clinical significance.
DISCUSSION
In this study, we reported chest CT findings in patients at admission at hospital in traditional wards for COVID-19. We found that clinical characteristics at admission associated with poor outcome were age over 65 years (58.0% ≥65 years vs. 43.9%), male sex (68.1% vs. 52.3%), oxygen saturation < 92% or a need of oxygen therapy at admission (52.2% vs. 25.2%). All these clinical characteristic are in accordance with previous reports [12,13]. Biological characteristics at admission associated with worse prognostic were C-reactive level >5 mg/dL (56.5% vs. 28.0%), and lymphopenia (49.3% vs. 26.5%), also in accordance with results from previous cohorts [14–16].
The prevalences of CT signs we observed were comparable to findings of studies conducted in other countries [7,17–19]. Our results are in accordance with the systematic review performed by Salehi et al. [18] of 919 patients, despite some interesting differences: we found a higher prevalence of GGOs (94,5% vs 88%) and a lower prevalence pulmonary consolidations (18% vs 31%). This discrepancy has also been observed in other studies: In the series by Zhu et al. (32 patients), GGOs were found in only 47% of patients [Chung et al. reported >50% of 21 patients with GGOs without consolidative opacities, 29% with GGOs in addition to consolidative opacities at presentation and crazy paving pattern in 19%, while we found a prevalence of 27,9% for nodular parenchyma consolidation, 73,6% for intralobular crazy paving [20]. There are two hypothesis to explain these discrepancies: CT may be performed later in Chung and al study or clinical status may be worse in present study.
After adjustment for these clinical and biological variables, we found that 4 CT signs at admission associated with a poor outcome: extension of GGOs ≥50% (OR: 3.52; 95% CI: 1.42-8.75), predominance of intralobular consolidation/crazy paving (OR: 2.19; 95% CI: 0.91-5.28), vascular thickening (OR: 2.10; 95% CI: 0.84-5.22) and at a lesser extent pleural thickening (OR: 1.51; 95% CI: 0.55-4.13). This is concordant with results of Shayganfar and al. study [11]. Colombi and al use software for quantitative analysis in the development of prognostic criteria; this analysis requires the use of software external to the examination reading system and therefore seems incompatible with sustained clinical activity [9].
In line with other studies, the predominant patterns of abnormalities on CT for our patients were GGOs (52,7%) with a peripheral distribution and bilateral, multifocal lower lung involvement [2,3,16,18,21]. In our study, extension of GGOs ≥50% was strongly associated with poor outcome (OR: 3.52; 95% CI: 1.42-8.75).
The extent of the lesions has already been correlated with the severity of the infection in previous reports [22]. Liu and al. showed that an increased in the number of involved lobes from the baseline are associated with poor prognosis [21]. Crazy paving pattern corresponds to thickened inter lobular septa and intralobular lines with superimposition on a GGO background, resembling irregular paving stones. Based on previous pathological knowledge of severe acute respiratory syndrome (SARS) and Middle East Respiratory Syndrome (MERS), this sign may result from alveolar edema and interstitial inflammation of acute lung injury [5,23]. This may explain the association of crazy paving as predominant sign with poor outcome in our cohort. An interesting CT finding was the presence of enlarged subsegmental pulmonary vessels in 72,1% of study participants, that was associated with poor outcome. Vascular thickening is often described as the dilatation of pulmonary vessels around and within the lesions on CT images. This finding has been described by Zhao et al. in 71,3% of COVID-19 pneumonia cases [12]. Bai et al. described subsegmental vascular enlargement in 59% of the patients with COVID-19 pneumonia as compared with 22% of patients with non-viral pneumonia [20]. Ye et al. suggested that vascular enlargement may be attributed to the damage and swelling of the capillary wall caused by proinflammatory factors [24].
According to Shi and al., in a study of 81 patients, 32% of them had pleural thickening while 5% showed pleural effusion [25]. The impact of this sign as a prognosis sign is debated: we found no association with poor outcome, in contrast with other cohorts [12,13].
Pan and al. showed that CT findings change with the disease course with preponderance of GGOs in early disease, followed by the development of crazy paving and, finally, consolidation later in the disease course. Crazy-paving pattern would be a manifestation as the disease course after GGO and before condensation [6]. Bernheim et al. showed also that lung involvement gradually increased to consolidation up to 2 weeks after disease onset [7] This may explain why the prevalence of condensation was low (27,9%) in our study. In our study, CT-scan were not repeated and disease course was variable at admission. However the aim of our study was to identify Ct patterns associated with poor outcome at admission, whatever the duration of symptoms. In general, the patients in our study were somewhat older (48,8% >65 years) with more men (57,7%) described in prior reports. Our study had several limitations. RT-PCR-based tests were used to confirm the infection status, which may minimize the misclassification error. Very few missing data were observed, and were handled by multiple imputation.
The findings of the statistical tests should be interpreted with caution even though our cohort is relatively large.
The size of ORs allow the conclusion of clinical significance for the association of predominance of intralobular crazy paving, vascular thickening and pleural thickening with poor outcome, albeit statistical significance was not reached.
CONCLUSION
Extension of GGOs ≥50%, predominance of intralobular consolidation/crazy paving, vascular thickening and at a lesser extent pleural thickening are independent markers of poor outcome in the setting of patients admitted to traditional wards for COVID-19 pneumonia.
CONFLICT OF INTERESTS
The authors declare no conflict of interests.
REFERENCES
| 1. Johns Hopkins Coronavirus resource center-https://coronavirus.jhu.edu/map.html n.d. |
| 2. Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, et al. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology 2020:200490. |
| 3. Fu F, Lou J, Xi D, Bai Y, Ma G, Zhao B, et al. Chest computed tomography findings of coronavirus disease 2019 (COVID-19) pneumonia. Eur Radiol 2020;30(10):5489-5498. |
| 4. Ding X, Xu J, Zhou J, Long Q. Chest CT findings of COVID-19 pneumonia by duration of symptoms. European Journal of Radiology 2020;127:109009. |
| 5. Gao F, Li M, Ge X, Zheng X, Ren Q, Chen Y, et al. Multi-detector spiral CT study of the relationships between pulmonary ground-glass nodules and blood vessels. Eur Radiol 2013;23:3271–7. |
| 6. Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol 2020 ;30(6):3306-3309. |
| 7. Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology 2020;295:200463. |
| 8. Chest CT-derived pulmonary artery enlargement at the admission predicts overall survival in COVID-19 patients: insight from 1461 consecutive patients in Italy - Eur Radiol 2020 Dec 23;1-11. |
| 9. Colombi D, Villani GD, Maffi G, Risoli C, Bodini FC, Petrini M, et al. Qualitative and quantitative chest CT parameters as predictors of specific mortality in COVID-19 patients. Emerg Radiol 2020;27:701–10. |
| 10. Colombi D, Bodini FC, Petrini M, Maffi G, Morelli N, Milanese G, et al. Well-aerated Lung on Admitting Chest CT to Predict Adverse Outcome in COVID-19 Pneumonia. Radiology 2020:201433. |
| 11. Shayganfar A, Sami R, Sadeghi S, Dehghan M, Khademi N, Rikhtegaran R, et al. Risk factors associated with intensive care unit (ICU) admission and in-hospital death among adults hospitalized with COVID-19: a two-center retrospective observational study in tertiary care hospitals. Emerg Radiol 2021 Feb 3;1-7. |
| 12. Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation Between Chest CT Findings and Clinical Conditions of Coronavirus Disease (COVID-19) Pneumonia: A Multicenter Study. AJR Am J Roentgenol 2020;214:1072–7. |
| 13. Wu J, Pan J, Teng D, Xu X, Feng J, Chen Y-C. Interpretation of CT signs of 2019 novel coronavirus (COVID-19)pneumonia.European Radiology2020;30(10):5455-62. |
| 14. Tan L, Wang Q, Zhang D, Ding J, Huang Q, Tang Y-Q, et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther 2020;5:33. |
| 15. Li Q, Ding X, Xia G, Chen H-G, Chen F, Geng Z, et al. Eosinopenia and elevated C-reactive protein facilitate triage of COVID-19 patients in fever clinic: a retrospective case-control study. EClinicalMedicine 2020:100375. |
| 16. Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology 2020;295:210–7. |
| 17. Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology 2020;295:715–21. |
| 18. Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol 2020:1–7. |
| 19. Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, et al. Chest CT Features of COVID-19 in Rome, Italy. Radiology 2020:201237. |
| 20. Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology 2020;295:202–7. |
| 21. Liu J, Chen T, Yang H, Cai Y, Yu Q, Chen J, et al. Clinical and radiological changes of hospitalised patients with COVID-19 pneumonia from disease onset to acute exacerbation: a multicentre paired cohort study. Eur Radiol. 2020;30(10):5702-5708. |
| 22. Liang T, Liu Z, Wu CC, Jin C, Zhao H, Wang Y, et al. Evolution of CT findings in patients with mild COVID-19 pneumonia. Eur Radiol. 2020 Sep;30(9):4865-4873. |
| 23. Wong KT, Antonio GE, Hui DSC, Lee N, Yuen EHY, Wu A, et al. Thin-section CT of severe acute respiratory syndrome: evaluation of 73 patients exposed to or with the disease. Radiology 2003;228:395–400. |
| 24. Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020 Aug;30(8):4381-4389. |
| 25. Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020;20:425–34. |
FIGURE - TABLES
REFERENCES
| 1. Johns Hopkins Coronavirus resource center-https://coronavirus.jhu.edu/map.html n.d. |
| 2. Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, et al. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology 2020:200490. |
| 3. Fu F, Lou J, Xi D, Bai Y, Ma G, Zhao B, et al. Chest computed tomography findings of coronavirus disease 2019 (COVID-19) pneumonia. Eur Radiol 2020;30(10):5489-5498. |
| 4. Ding X, Xu J, Zhou J, Long Q. Chest CT findings of COVID-19 pneumonia by duration of symptoms. European Journal of Radiology 2020;127:109009. |
| 5. Gao F, Li M, Ge X, Zheng X, Ren Q, Chen Y, et al. Multi-detector spiral CT study of the relationships between pulmonary ground-glass nodules and blood vessels. Eur Radiol 2013;23:3271–7. |
| 6. Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol 2020 ;30(6):3306-3309. |
| 7. Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology 2020;295:200463. |
| 8. Chest CT-derived pulmonary artery enlargement at the admission predicts overall survival in COVID-19 patients: insight from 1461 consecutive patients in Italy - Eur Radiol 2020 Dec 23;1-11. |
| 9. Colombi D, Villani GD, Maffi G, Risoli C, Bodini FC, Petrini M, et al. Qualitative and quantitative chest CT parameters as predictors of specific mortality in COVID-19 patients. Emerg Radiol 2020;27:701–10. |
| 10. Colombi D, Bodini FC, Petrini M, Maffi G, Morelli N, Milanese G, et al. Well-aerated Lung on Admitting Chest CT to Predict Adverse Outcome in COVID-19 Pneumonia. Radiology 2020:201433. |
| 11. Shayganfar A, Sami R, Sadeghi S, Dehghan M, Khademi N, Rikhtegaran R, et al. Risk factors associated with intensive care unit (ICU) admission and in-hospital death among adults hospitalized with COVID-19: a two-center retrospective observational study in tertiary care hospitals. Emerg Radiol 2021 Feb 3;1-7. |
| 12. Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation Between Chest CT Findings and Clinical Conditions of Coronavirus Disease (COVID-19) Pneumonia: A Multicenter Study. AJR Am J Roentgenol 2020;214:1072–7. |
| 13. Wu J, Pan J, Teng D, Xu X, Feng J, Chen Y-C. Interpretation of CT signs of 2019 novel coronavirus (COVID-19)pneumonia.European Radiology2020;30(10):5455-62. |
| 14. Tan L, Wang Q, Zhang D, Ding J, Huang Q, Tang Y-Q, et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther 2020;5:33. |
| 15. Li Q, Ding X, Xia G, Chen H-G, Chen F, Geng Z, et al. Eosinopenia and elevated C-reactive protein facilitate triage of COVID-19 patients in fever clinic: a retrospective case-control study. EClinicalMedicine 2020:100375. |
| 16. Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology 2020;295:210–7. |
| 17. Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology 2020;295:715–21. |
| 18. Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol 2020:1–7. |
| 19. Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, et al. Chest CT Features of COVID-19 in Rome, Italy. Radiology 2020:201237. |
| 20. Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology 2020;295:202–7. |
| 21. Liu J, Chen T, Yang H, Cai Y, Yu Q, Chen J, et al. Clinical and radiological changes of hospitalised patients with COVID-19 pneumonia from disease onset to acute exacerbation: a multicentre paired cohort study. Eur Radiol. 2020;30(10):5702-5708. |
| 22. Liang T, Liu Z, Wu CC, Jin C, Zhao H, Wang Y, et al. Evolution of CT findings in patients with mild COVID-19 pneumonia. Eur Radiol. 2020 Sep;30(9):4865-4873. |
| 23. Wong KT, Antonio GE, Hui DSC, Lee N, Yuen EHY, Wu A, et al. Thin-section CT of severe acute respiratory syndrome: evaluation of 73 patients exposed to or with the disease. Radiology 2003;228:395–400. |
| 24. Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020 Aug;30(8):4381-4389. |
| 25. Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020;20:425–34. |
ARTICLE INFO DOI: 10.12699/jfvpulm.12.38.2021.44
Conflict of Interest
Non
Date of manuscript receiving
25/02/2021
Date of publication after correction
25/08/2021
Article citation
Bilfeld, M. Lafaurie, A. Sommet, J. Monsinjeon, F. Lafourcade, F. Lapegue, H. Chiavassa, H. Basselerie, S. Collot, H. Rousseau, N. Sans, GM. Blondel, G. Moulis. CT findings at admission to traditional wards for COVID-19 infection are independently associated with severe outcome. J Func Vent Pulm 2021;38(12):44-49