
 English
English
 French
French
An unusual primitive localization of synovialosarcoma: About a case and review of the literature
Une localisation primitive inhabituelle du synovialosarcome: À propos d'un cas et revue de la littérature
Hanane Charaf, Mouna Soualhi, Rachida Zahraoui, Jamal Eddine Bourkadi, Sabrin Darqaoui
Pneumo-Phtisiology Department, Faculty of Medicine and Pharmacy Mohamed V University, Moulay Youssef Hospital, Rabat, Morocco
Anatomopathology Department, Faculty of Medicine and Pharmacy Mohamed V University, Moulay Youssef Hospital, Rabat, Morocco
Corresponding author:
Hanane Charaf Pneumo-Phtisiology Department, Faculty of Medicine and Pharmacy Mohamed V University, Moulay Youssef Hospital, Rabat, Morocco
E-mail: dr.hanane.charaf@gmail.com
ABSTRACT
Introduction. Synovialosarcoma is a rare malignant tumor, accounting for 10% of soft tissue sarcomas. It usually develops in the limbs and its pulmonary localization is exceptional. The diagnosis can only be made after having eliminated an extrapleuropulmonary localization in the past and at the time of diagnosis. The image‑guided tru-cut core biopsy or open lung biopsy and their histopathological examination, supplemented by immunohistochemistry are preferable for the tissue diagnosis of pulmonary synovial sarcoma.
Clinical observation. We report a rare case of primary pulmonary synovial sarcoma in a 58-year-old man, the objective of which is to show diagnostic difficulties.
Conclusion. Trough this case, we present a rare disease that is often difficult to diagnose.
KEYWORDS: Histopathology; immunohistochemistry; lung; primary synovial sarcoma.
RÉSUMÉ
Introduction. Le synovialosarcome est une tumeur maligne rare, représentant 10 % des sarcomes des tissus mous. Il se développe habituellement dans les membres et sa localisation pulmonaire est exceptionnelle. Le diagnostic ne peut être posé qu'après avoir éliminé une localisation extrapleuropulmonaire dans le passé et au moment du diagnostic. La biopsie au trocart guidée par l'image ou la biopsie pulmonaire ouverte et leur examen histopathologique, complété par l'immunohistochimie sont préférables pour le diagnostic tissulaire du sarcome synovial pulmonaire.
Observation clinique. Nous rapportons un cas rare de sarcome synovial pulmonaire primitif chez un homme de 58 ans dont l'objectif est de montrer des difficultés diagnostiques.
Conclusion. A travers ce cas, nous présentons une maladie rare souvent difficile à diagnostiquer.
MOTS CLÉS: Histopathologie ; immunohistochimie; poumon; sarcome synovial primitif.
INTRODUCTION
Synovial sarcoma is a rare soft tissue sarcoma accounting for 8% of all soft tissue tumors in the body. 50-60% of these cancers develop in the limbs [1]. Primary thoracic sarcomas are rare and represent less than 1% of all primary thoracic tumors [2]. Metastatic synovial sarcoma from extremities is the most common in pulmonary parenchyma and pleura. Only 0.5% of all primary pulmonary malignancies are due to pulmonary sarcomas, Primary pulmonary synovial sarcoma is a highly aggressive [3]. It affects the young adipose tissue (15-40 years) with a slight male predominance [4]. Approximately 30 cases of synovialosarcoma of primary pulmonary site are described in the literature. We report a new observation, presenting the particularities of this tumor, which is rarely seen in clinical practice.
CASE PRESENTATION
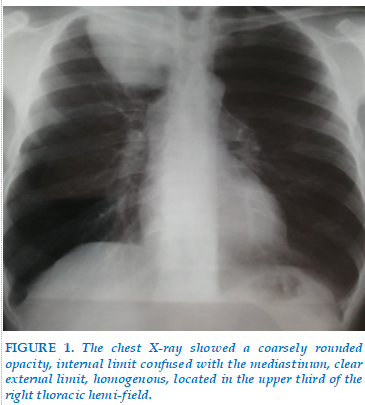
A 58-year-old patient, a chronic 25-package year smoker who quit a month ago, consulted for chest pain and dyspnea associated with a cough producing hemoptoiic sputum in the context of altered general condition. The physical examination was unremarkable. In addition, the notion of tuberculosis contagion was not retained. The chest X-ray showed a coarsely rounded opacity, internal limit confused with the mediastinum, clear external limit, homogenous, located in the upper third of the right thoracic hemi-field (Figure 1).
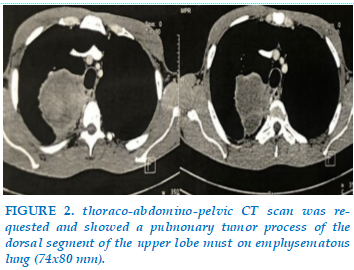
A thoraco-abdomino-pelvic CT scan was requested and showed a pulmonary tumor process of the dorsal segment of the upper lobe must on emphysematous
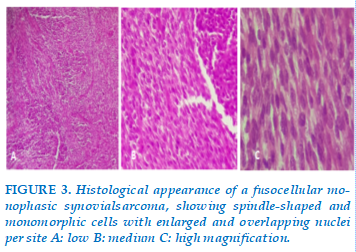
lung (74x80 mm) comes in contact with the ribs and spine backwards and in contact with the trachea and vessels under the clavicle forward without signs of invasion (Figure 2). The abdominal and pelvic stage was not abnormal, which is a priori, a fundamental element of the primitive character of the tumor. Transthoracic biopsy of the pulmonary tumor process was performed (guided by CT). It is concluded from grade I synovial sarcoma of the FNCLCC at the histological study of the fragments. The tumor showed spindle-shaped and monomorphic cells with enlarged and overlapping nuclei per site (Figure 3).
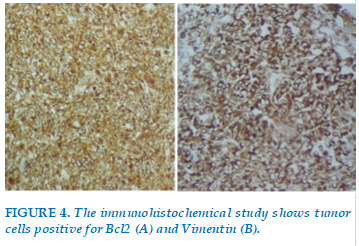
On immunohistochemical study, tumor cells were positive for Bcl2 (Figure 4) and vimentin (Figure 5).
They were negative for EMA. Unfortunately we could not perform chromosomal studies on this patient; we lack the molecular platform in our instruction because we belong to a low-income country. We retained the diagnosis after eliminating the differential diagnosis.
After the confirmation of the diagnosis, the patient was referred to the oncology center for chemotherapy, but he died of a devastating hemoptysis.
DISCUSSION
Synovial sarcoma is a rare soft tissue sarcoma accounting for 8% of all soft tissue tumors in the body. A 50-60% of these cancers develop in the limbs [1]. Primary thoracic sarcomas are rare and represent less than 1% of all primary thoracic tumors [2]. Metastatic synovial sarcoma from extremities is the most common in pulmonary parenchyma and pleura. Only 0.5% of all primary pulmonary malignancies are due to pulmonary sarcomas, Primary pulmonary synovial sarcoma is a highly aggressive [3]. It affects the young adipose tissue (15-40 years) with a slight male predominance [4].
The age of our patient is 58 years, which is much higher than the data in the literature but joins the series of Mastroianni et al. whose average age of patients was between 50 and 60 years [5]. Most sarcomas have not been associated with risk factors, but some genetic and environmental predispositions have been suggested in a minority of patients [6].
The diagnosis of primary pleuropulmonary synovial sarcoma (PPSS) requires a combination of clinical, radiological, pathological, and immunohistochemical investigations to exclude alternative primary tumors and metastatic sarcoma [7].
The origin tissue of synovial sarcomas is not well defined; it appears that they develop from a pluripotent mesenchymal cell with synovial differentiation [8].
The symptomatology as well as the imaging is not characterized by specific sign directing towards a synovial sarcoma. The clinical and radiological data are that of a pulmonary tumor process without histological specificity [9]. Our patient also had a non-specific clinical and paraclinical presentation. The radiologic manifestations of PPSS are no different from bronchogenic carcinoma, metastatic, or other primary lung tumors. However, the young age, absence of mediastinal adenopathy, and bone erosion despite a large size mass favors the diagnosis of a lung tumor other than bronchogenic carcinoma. Because lung is the most common site of metastasis in soft tissue SS and radiological features of primary and metastatic SS are similar, an extrathoracic tumor must be excluded by thorough clinical and radiological evaluation before the diagnosis of PPSS [10, 11].
Histologically, there are four histologic subtypes: biphasic, monophasic (spindle), monophasic epithelial, and poorly differentiated (round cell) tumors. The most commonly observed subtype is monophasic, and the biphasic subtype is easily diagnosed on the basis of the presence of both epithelial and spindle cells. However, the monophasic subtype can be misdiagnosed as other types of sarcoma [12]. Our patient had a monophasic fusiform subtype at the biopsy.
In the presence of malignant tumor proliferation of spindle-cell sarcomatous aspects, a carcinomatous component should always be sought to eliminate the diagnosis of sarcomatoid carcinoma. Once the pure character of sarcomatous proliferation is established, the possibility of a sarcomatoid carcinoma, which, unlike synovial sarcoma, is always rich in cytonuclear atypia, must be rejected at first sight. In addition, proliferating cells are intensely and diffusely positive to epithelial markers. After discarding these 2 more frequent events the diagnosis of sarcoma can be retained [13].
The next question is whether the pleuropulmonary tumor is primitive or secondary. The second eventuality is by far the most frequent. The mother tumor usually sits in the soft tissues. Only the absence of extrapleuropulmonary tumor localization in the past and at the time of diagnosis will attest to the primitive nature of the tumor. In our case, a thoraco-abdomino-pelvic CT scan had eliminated an extrathoracic localization of the tumor, so we had retained the diagnosis of primary pulmonary synovial sarcoma.
In immunohistochemistry, synovialosarcomas express in 90% of cases the Epithelial Membrane Antigen (EMA), and Bcl2 in 90% of cases, CD99 in 60% of cases and S100 in 30% of cases [14].
In most cases, there is a characteristic t translocation (X; 18) involving the SSX1 or SSX2 genes of the X chromosome (Xp11). Transcripts of the SYST-SSX fusion gene can be detected in pathological samples with a sensitivity of 96% and a specificity of 100% [15]. In the framework of our observation, immunohistochemistry revealed positivity to bcl2 and vimentin.
Despite its high sensitivity, molecular testing is not required if the diagnosis of synovial sarcoma is certain or probable on the basis of clinical, histological, and immunohistochemical evaluations [16].
There are no standard recommendations for the management of SS. Wherever feasible, wide surgical resection with tumor‑free margins remains the preferred modality of treatment followed by chemotherapy and/or radiotherapy [17].
Surgery is not recommended for tumors that are locally invasive or have metastatic disease. Neoadjuvant and adjuvant chemotherapy may be required in some cases along with surgery. SS is generally considered as relatively chemosensitive tumor, and treatment with adriamycin alone or in combination with ifosfamide remains the standard chemotherapy in metastatic disease [18‑24].
Undoubtedly, there is a serious need for an ideal therapeutic agent in SS that is more effective and less toxic. Several novel potential therapeutic targets under research are SS18‑SSX fusion oncogene, epidermal growth factor receptor, and vascular endothelial growth factor receptor [25, 26].
The prognosis for patients with PPSS is poor, with an overall 5-year survival rate of 50 percent.
Factors predicting a worse prognosis for patients with synovial sarcomas include tumor size (>5 cm), male gender, older age (>20 years), extensive tumor necrosis, high grade, large number of mitotic figures (>10 per 10 hpf), neurovascular invasion, and, recently, the SYT-SSX1 variant [12]. In our observation, approximately two months between the appearance of the first clinical signs and the confirmation of the diagnosis, the patient died after the first chemotherapy treatment with a devastating hemoptysis.
CONCLUSION
Primary pulmonary sarcomas are rare. They first discuss a tumor with double carcinomatous and sarcomatous contingent whose first component is discrete or was not interested in sampling. Once the diagnosis of sarcoma is established, a secondary pulmonary site should be removed, which is more likely. It is therefore only after a diagnostic procedure of exclusion that the primary pulmonary seat of a sarcoma will be retained. Our observation is in line with what has been reported in the literature.
CONFLICT OF INTEREST
Non.
REFERENCES
| 1. Penel N, Nisse C, Feddal S, Lartigau E. Epidemiology of soft tissue sarcomas in adults. Press Med 2001 Oct; 6; 30(28): 1405-13. PubMed| Google Scholar. |
| 2. Eilber FR, Eckardt J. Surgical management of soft tissue sarcoma. Semin Oncol 1997 Oct; 24(5): 526-33. PubMed| Google Scholar |
| 3. Shah UB, Joshi S, Ghorpade SV, Gaikwad SN, Sundrani RM. Primary pleuro‑pulmonary synovial sarcoma. Indian J Chest Dis Allied Sci 2010; 52:169‑72. |
| 4. Zeren H, Moran CA, Suster S, Fishback NF, Koss MN. Primary pulmonary sarcomas with features of monophasic synovialsarcoma: a clinicopathological, immunohistochemical and ultrastructural study of 25 cases. Hum Pathol 1995 May; 26(5): 474-80. PubMed| Google |
| 5. Etienne-Mastroianni B, Falchero L, Chalabreysse L, Loire R, Ranchere D, Souquet PJ et al. Primary sarcoma of the lung: a clinicopathologic study of 12 cases. Lung Cancer 2002 Dec; 38(3): 283-9. PubMed|Google Scholar |
| 6. Zahm SH, Fraumeni JF. The epidemiology of soft tissue sarcoma. Semin Oncol 1997; 25(5): 504-14. PubMed| Google Scholar |
| 7. Arun RD, “A rare primary synovial sarcoma of lung – case report with literature review,” Nursing & Health Sciences 2017; vol. 3: no. 1. |
| 8. Qassimi L, El Khattabi W, Lyousfi H, Aichane A, Afif H, “Une tumeur rare de la paroi thoracique : le synovialosarcome,” Revue de Pneumologie Clinique 2015 ; vol. 71, no. 4, pp. 251-252. |
| 9. Panigrahi MK, Pradhan G, Sahoo N, Mishra P, Patra S, Mohapatra PR, “Primary pulmonary synovial sarcoma: A reappraisal,” Journal of Cancer Research and Therapeutics 2017. |
| 10. Frazier AA, Franks TJ, Pugatch RD, Galvin JR. From the archives of the AFIP: Pleuropulmonary synovial sarcoma. Radiographics 2006; 26:923‑40. |
| 11. Kim GH, Kim MY, Koo HJ, Song JS, Choi CM. Primary pulmonary synovial sarcoma in a tertiary referral center: Clinical characteristics, CT, and 18F‑FDG PET findings, with pathologic correlations. Medicine (Baltimore) 2015; 94: e1392. |
| 12. Chang C-C, Chang P-Y. Primary pulmonary synovial sarcoma. Journal of Cancer Research and Practice 2018; 5 (1):24–26. doi: 10.1016 j.jcrpr.2017.09.002 .https://doi.org/10.1016/j.jcrpr.2017.09.002 . [CrossRef ] [Google Scholar] |
| 13. Thakur C, Li WR, Gupta S, “Primary pulmonary synovial sarcoma: one case report,” Journal of Lung Cancer Diagnosis & Treatment 2017; vol. 2: p.114. |
| 14. Lino-Silva LS, Flores-Gutiérrez JP, Vilches-Cisneros N, Domínguez-Malagón HR. TLE1 est exprimé dans la majorité des sarcomes synoviaux pleuropulmonaires primaires. Virchows Arch 2011; 459 (6): 615-21 |
| 15. Ngahane BH. Evaluation of factors prognosis of thoracic synovialosarcomas. Rev Mal Respiir 2010; 27(1): 93-7. PubMed| Google Scholar |
| 16. Rajeev LK, Patidar R, Babu G, Suresh Babu MC, Lokesh KN, Patil Okaly GV, “A rare case of primary synovial sarcoma of lung,” Lung India 2017 vol. 34, no. 6:545–547. |
| 17. Jain A, Sajeevan KV, Babu KG, Lakshmaiah KC. Chemotherapy in adult soft tissue sarcoma. Indian J Cancer 2009; 46:274‑87 |
| 18. Essary LR, Vargas SO, Fletcher CD. Primary pleuropulmonary synovial sarcoma: Reappraisal of a recently described anatomic subset Cancer 2002; 94:459‑69. |
| 19. Okamoto S, Hisaoka M, Daa T, Hatakeyama K, Iwamasa T, Hashimoto H. P rimar y pulmonar y synovial sarcoma: A clinicopathologic, immunohistochemical, and molecular study of 11 cases. Hum Pathol 2004; 35:850‑6. |
| 20. Bégueret H, Galateau‑Salle F, Guillou L, Chetaille B, Brambilla E, Vignaud JM, et al. Primary intrathoracic synovial sarcoma: A clinicopathologic study of 40 t(X;18) positive cases from the French Sarcoma Group and the Mesopath Group. Am J Surg Pathol 2005; 29:339‑46. |
| 21. Suster S, Moran CA. Primary synovial sarcomas of the mediastinum: A clinicopathologic, immunohistochemical, and ultrastructural study of 15 cases. Am J Surg Pathol 2005; 29:569‑78. |
| 22. Hartel PH, Fanburg‑Smith JC, Frazier AA, Galvin JR, Lichy JH, Shilo K, et al. Primary pulmonary and mediastinal synovial sarcoma: A clinicopathologic study of 60 cases and comparison with five prior series. Mod Pathol 2007; 20:760‑9. |
| 23. Lino‑Silva LS, Flores‑Gutiérrez JP, Vilches‑ Cisneros N, Domínguez‑Malagón HR. TLE1 is expressed in the majority of primary pleuropulmonary synovial sarcomas. Virchows Arch 2011; 459:615‑21. |
| 24. Lan T, Chen H, Xiong B, Zhou T, Peng R, Chen M, et al. Primary pleuropulmonary and mediastinal synovial sarcoma: A clinicopathologic and molecular study of 26 genetically confirmed cases in the largest institution of Southwest China. Diagn Pathol 2016; 11:62. |
| 25. Casali PG. Histology‑and non‑histology‑driven therapy for treatment of soft tissue sarcomas. Ann Oncol 2012; 23 Suppl 10:x167‑9. |
| 26. Wakamatsu T, Naka N, Sasagawa S, Tanaka T, Takenaka S, Araki N, et al. Deflection of vascular endothelial growth factor action by SS18‑SSX and composite vascular endothelial growth factor‑ and chemokine (C‑X‑C motif) receptor 4‑targeted therapy in synovial sarcoma. Cancer Sci 2014; 105:1124‑34. |
FIGURE
REFERENCES
| 1. Penel N, Nisse C, Feddal S, Lartigau E. Epidemiology of soft tissue sarcomas in adults. Press Med 2001 Oct; 6; 30(28): 1405-13. PubMed| Google Scholar. |
| 2. Eilber FR, Eckardt J. Surgical management of soft tissue sarcoma. Semin Oncol 1997 Oct; 24(5): 526-33. PubMed| Google Scholar |
| 3. Shah UB, Joshi S, Ghorpade SV, Gaikwad SN, Sundrani RM. Primary pleuro‑pulmonary synovial sarcoma. Indian J Chest Dis Allied Sci 2010; 52:169‑72. |
| 4. Zeren H, Moran CA, Suster S, Fishback NF, Koss MN. Primary pulmonary sarcomas with features of monophasic synovialsarcoma: a clinicopathological, immunohistochemical and ultrastructural study of 25 cases. Hum Pathol 1995 May; 26(5): 474-80. PubMed| Google |
| 5. Etienne-Mastroianni B, Falchero L, Chalabreysse L, Loire R, Ranchere D, Souquet PJ et al. Primary sarcoma of the lung: a clinicopathologic study of 12 cases. Lung Cancer 2002 Dec; 38(3): 283-9. PubMed|Google Scholar |
| 6. Zahm SH, Fraumeni JF. The epidemiology of soft tissue sarcoma. Semin Oncol 1997; 25(5): 504-14. PubMed| Google Scholar |
| 7. Arun RD, “A rare primary synovial sarcoma of lung – case report with literature review,” Nursing & Health Sciences 2017; vol. 3: no. 1. |
| 8. Qassimi L, El Khattabi W, Lyousfi H, Aichane A, Afif H, “Une tumeur rare de la paroi thoracique : le synovialosarcome,” Revue de Pneumologie Clinique 2015 ; vol. 71, no. 4, pp. 251-252. |
| 9. Panigrahi MK, Pradhan G, Sahoo N, Mishra P, Patra S, Mohapatra PR, “Primary pulmonary synovial sarcoma: A reappraisal,” Journal of Cancer Research and Therapeutics 2017. |
| 10. Frazier AA, Franks TJ, Pugatch RD, Galvin JR. From the archives of the AFIP: Pleuropulmonary synovial sarcoma. Radiographics 2006; 26:923‑40. |
| 11. Kim GH, Kim MY, Koo HJ, Song JS, Choi CM. Primary pulmonary synovial sarcoma in a tertiary referral center: Clinical characteristics, CT, and 18F‑FDG PET findings, with pathologic correlations. Medicine (Baltimore) 2015; 94: e1392. |
| 12. Chang C-C, Chang P-Y. Primary pulmonary synovial sarcoma. Journal of Cancer Research and Practice 2018; 5 (1):24–26. doi: 10.1016 j.jcrpr.2017.09.002 .https://doi.org/10.1016/j.jcrpr.2017.09.002 . [CrossRef ] [Google Scholar] |
| 13. Thakur C, Li WR, Gupta S, “Primary pulmonary synovial sarcoma: one case report,” Journal of Lung Cancer Diagnosis & Treatment 2017; vol. 2: p.114. |
| 14. Lino-Silva LS, Flores-Gutiérrez JP, Vilches-Cisneros N, Domínguez-Malagón HR. TLE1 est exprimé dans la majorité des sarcomes synoviaux pleuropulmonaires primaires. Virchows Arch 2011; 459 (6): 615-21 |
| 15. Ngahane BH. Evaluation of factors prognosis of thoracic synovialosarcomas. Rev Mal Respiir 2010; 27(1): 93-7. PubMed| Google Scholar |
| 16. Rajeev LK, Patidar R, Babu G, Suresh Babu MC, Lokesh KN, Patil Okaly GV, “A rare case of primary synovial sarcoma of lung,” Lung India 2017 vol. 34, no. 6:545–547. |
| 17. Jain A, Sajeevan KV, Babu KG, Lakshmaiah KC. Chemotherapy in adult soft tissue sarcoma. Indian J Cancer 2009; 46:274‑87 |
| 18. Essary LR, Vargas SO, Fletcher CD. Primary pleuropulmonary synovial sarcoma: Reappraisal of a recently described anatomic subset Cancer 2002; 94:459‑69. |
| 19. Okamoto S, Hisaoka M, Daa T, Hatakeyama K, Iwamasa T, Hashimoto H. P rimar y pulmonar y synovial sarcoma: A clinicopathologic, immunohistochemical, and molecular study of 11 cases. Hum Pathol 2004; 35:850‑6. |
| 20. Bégueret H, Galateau‑Salle F, Guillou L, Chetaille B, Brambilla E, Vignaud JM, et al. Primary intrathoracic synovial sarcoma: A clinicopathologic study of 40 t(X;18) positive cases from the French Sarcoma Group and the Mesopath Group. Am J Surg Pathol 2005; 29:339‑46. |
| 21. Suster S, Moran CA. Primary synovial sarcomas of the mediastinum: A clinicopathologic, immunohistochemical, and ultrastructural study of 15 cases. Am J Surg Pathol 2005; 29:569‑78. |
| 22. Hartel PH, Fanburg‑Smith JC, Frazier AA, Galvin JR, Lichy JH, Shilo K, et al. Primary pulmonary and mediastinal synovial sarcoma: A clinicopathologic study of 60 cases and comparison with five prior series. Mod Pathol 2007; 20:760‑9. |
| 23. Lino‑Silva LS, Flores‑Gutiérrez JP, Vilches‑ Cisneros N, Domínguez‑Malagón HR. TLE1 is expressed in the majority of primary pleuropulmonary synovial sarcomas. Virchows Arch 2011; 459:615‑21. |
| 24. Lan T, Chen H, Xiong B, Zhou T, Peng R, Chen M, et al. Primary pleuropulmonary and mediastinal synovial sarcoma: A clinicopathologic and molecular study of 26 genetically confirmed cases in the largest institution of Southwest China. Diagn Pathol 2016; 11:62. |
| 25. Casali PG. Histology‑and non‑histology‑driven therapy for treatment of soft tissue sarcomas. Ann Oncol 2012; 23 Suppl 10:x167‑9. |
| 26. Wakamatsu T, Naka N, Sasagawa S, Tanaka T, Takenaka S, Araki N, et al. Deflection of vascular endothelial growth factor action by SS18‑SSX and composite vascular endothelial growth factor‑ and chemokine (C‑X‑C motif) receptor 4‑targeted therapy in synovial sarcoma. Cancer Sci 2014; 105:1124‑34. |
ARTICLE INFO DOI: 10.12699/jfvpulm.12.38.2021.61
Conflict of Interest
Non
Date of manuscript receiving
25/02/2021
Date of publication after correction
25/08/2021
Article citation
Hanane Charaf, Mouna Soualhi, Rachida Zahraoui, Jamal Eddine Bourkadi, Sabrin Darqaoui. An unusual primitive localization of synovialosarcoma: About a case and review of the literature. J Func Vent Pulm 2021;38(12):61-65