
 English
English
 French
French
A successful thrombolysis for ischemic stroke related to HIV and SARS-COV-2 co-infection: A case report
Une thrombolyse réussie pour un accident vasculaire cérébral ischémique lié à la co-infection par le VIH et le SRAS-COV-2: un rapport de cas
Mohamed Amine MNAILI 1,2 Ahmed Bourazza 3
1: Neurology departement, Agadir Military Hospital, Agadir, Morocco
2: University of Hassan II, Casablanca, Morocco
3: Neurology departement, Mohammed V Military Hospital, Rabat, Morocco
Corresponding author:
MNAILI Mohamed Amine. Neurology departement, Agadir Military Hospital, Agadir, Morocco.
E-mail: aminemed08@gmail.com
ABSTRACT
The impact of HIV in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has not been well established. It is uncertain if outcomes are better or worse in these patients compared with COVID-19 patients with diabetes mellitus, hypertension and other chronic diseases.
We present HIV-positive case with COVID-19 pneumonia admitted to the emergency department in the setting of a thrombolysis alert for tetraparesis with dysarthria and left facial paralysis whose explorations revealed a bilateral paramedian pontine ischemic stroke. Patient had favourable outcomes.
KEYWORDS: HIV; SARS-CoV-2 Infection; Ischemic Stroke; Covid-19; case report.
RÉSUMÉ
L’impact de l’infection VIH sur l’infection par du syndrome respiratoire aigu sévère due au le coronavirus 2 (SRAS-CoV-2) n’est bien établi. Il n’est pas certain que les résultats soient meilleurs ou pires chez ces patients par rapport aux patients atteints de COVID-19 souffrant de diabète sucré, d’hypertension et d’autres maladies chroniques.
Nous présentons un cas séropositif avec pneumonie COVID-19 admis aux urgences dans le cadre d’une alerte thrombolyse pour tétraparésie avec dysarthrie et paralysie faciale gauche dont les explorations ont révélé un accident vasculaire cérébral ischémique pontique paramédian bilatéral. Le patient a eu des suites favorables.
MOTS CLÉS: VIH; SARS-CoV-2; Infection; accident vasculaire cérébrale ischémique; Covid-19.
INTRODUCTION
SARS COV 2 viral infection may manifest by respiratory symptoms or other symptoms, such as cardiovascular manifestations. In addition, SARS COV 2 also has neurological invasive capabilities and could spread from the respiratory system to the central nervous system [1,2]. People living with Human Immunodeficiency Virus (PLHIV) are at greater risk of developing prolonged illness due to COVID 19 leading to longer duration of virus shedding owing to their underlying immune defects.
In this article, we will represent a case of a 68 years old patient coinfected with pneumonia resulting from SARS-CoV-2 and the human immunodeficiency virus (HIV), admitted to the emergency department in the setting of a thrombolysis alert for tetraparesis with dysarthria and left facial paralysis whose explorations revealed a bilateral paramedian pontine ischemic stroke.
CASE PRESENTATION
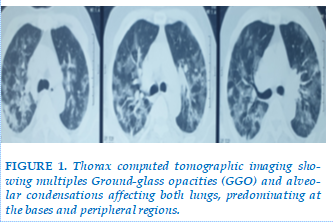
Here we report the case of a 68 years old patient with comorbidities of diabetes and HIV, admitted to the emergency department feeling generally unwell, with 3 days of symptoms including diaphoresis, dizziness, loose stools, and loss of taste sensation. The patient was using tenofovir, lamivudine, and efavirenz. His TCD4 lymphocyte count was measured at 1,163 cells, with a viral load that remained undetectable for a long period of time. On arrival, the patient was hemodynamically instable with a blood pressure of 130/80 mmHg,tachycardic at111 bpm, polypneic with a respiratory rate of 28 breaths/min, and oxygen saturation of 88 % on room air, the temperature was at 38.2 ◦C. Reverse transcription polymerase chain reaction (RT-PCR) showed negative results for SARS-CoV-2 infection, a computed tomography (CT) examination of the chest showed a radiological pattern typically reported following the pulmonary involvement of SARS-CoV-2 (Figure 1).
Laboratory tests showed signs of the inflammatory response, white blood cells counted 14490/μl, C-reactive protein (CRP) at 123 mg/l, lymphopenia at 670/μ ferritin was elevated at 5043.15 μg/, procalcitonin (PCT) at 1.39 ng/ml, interleukin-6(IL-6) at 213 pg/ml, D-Dimer at 2.3, fibrinogen 5.4 g/l, the result of laboratory test for cardiac, renal, liver functions were normal. However, hospitalization was required due to the onset of both dyspnea and asthenia. He was placed on a 100% non-rebreather mask and oxygen saturation improved to 93%. He was commenced on 50 mg hydrocortisone 6-hourly, 60 mg enoxaparin twice daily, 1.2 g amoxicillin-clavulanic acid 8-hourly, 240 mg intravenous gentamicin daily. The patient improved, requiring nasal prongs 2 days later, and a further 3 days later he did not require any supplemental oxygen.
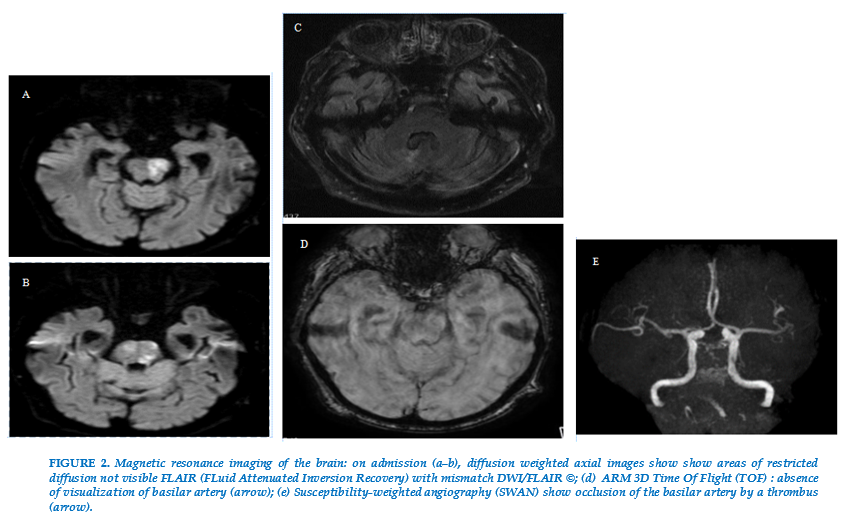
The patient was clinically compensated for respiratory infection, and did not require other therapeutic measures to control the respiratory condition. Four days after hospital discharge, the patient developed sudden onset of tetraparesis, dysarthria, and left facial paralysis and decreased alertness. At that time, the patient scored 18 on the National Institutes of Health Stroke Scale. Brain MRI came back in favor of a with visible thrombus in basilar artery (Figure 2). The decision of thrombolysis was urgently indicated with 90 mg of actilyse for a weight of 96 Kg (9mg loading dose, 81 mg maintenance dose) without any incident, then the patient was transferred to the neurology department.
After six days, there was an improvement in neurological symptoms, the neurological examination revealed (Eye opening:4/4, Motor response:6/6, Verbal respone:5/5) with the improvement of muscle strength at 4/5, also. The patient was very satisfied after the improvement in his clinical condition.
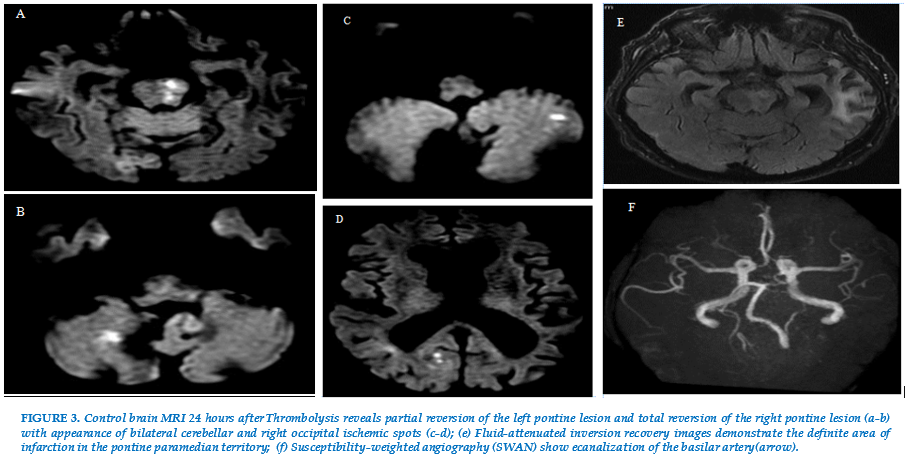
Control brain MRI reveals partial reversion of the left pontine lesion and total reversion of the right pontine lesion with appearance of bilateral cerebellar and right occipital ischemic spots.(Figure 3) a regression of biological markers of inflammation was also noted.
DISCUSSION
Simple symptoms of SARS COV 2 viral infection include fever, cough, and dyspnea; in severe cases, patients develop acute respiratory distress syndrome (ARDS), acute heart problems, and multiple organ dysfunction [3] Additionally, SARS COV 2 can also affect the central nervous system , due to excessive inflammation, hypoxia and a hypercoagulation state [4].
In addition to traditional risk factors, HIV is associated with other factors that increase the risk of stroke, including high viremia, immunosuppression, and use of antiretrovirals such as protease inhibitors, which can lead to dyslipidemia and lipodystrophy. The etiology of stroke in PLHIV is multifactorial, including large artery atherosclerosis, small vessel disease, cardioembolism, central nervous system (CNS) infections, coagulation disorders, and nonatherosclerotic vasculopathy [5].. Several mechanisms have been proposed to explain neurological insult in SARS-CoV-2, including direct injury, hypoxic injury, immunological injury, and neuroinvasion via angiotensin-converting enzyme 2 (ACE2) receptors. This involvement has no direct relationship with the appearance of pulmonary damage or its severity [6]. The pathophysiology of stroke in patients with confirmed SARS CoV-2 is not yet well defined. However, inflammatory activity resulting from infection, with activation of the interleukin
cascade, can lead to coagulation abnormalities, which contribute to the development of thromboembolic events. Under these conditions, it is necessary to identify patients at high potential for thromboembolic events through laboratory monitoring and assays of inflammatory markers (CRP and D-dimer) [7].
Diagnosis is usually based on presenting symptoms, data from clinical examination and brain imaging, other imaging tests (CT, MRI, TTE, Doppler, Angiography), and blood tests are performed to identify the cause of stroke. Treatment may include medications to dissolve clots or make the blood less likely to clot, as well as surgery or angioplasty to open blocked arteries; intravenous thrombolysis is the only approved systemic impact treatment for patients in acute ischemic stroke [8].
CONCLUSION
SARS-CoV-2 co-infection can be a further burden to people living with HIV. Neurological involvement, including ischemic stroke, may be the primary manifestation of COVID-19 infection; clinicians should be aware of that atypical manifestation even in the absence of respiratory tract symptoms.
CONFLICT OF INTEREST
None.
REFERENCES
FIGURES
REFERENCES
ARTICLE INFO DOI: 10.12699/jfvpulm.15.46.2024.59
Conflict of Interest
Non
Date of manuscript receiving
28/03/2024
Date of publication after correction
26/06/2024
Article citation
Mohamed Amine MNAILI Ahmed Bourazza. A successful thrombolysis for ischemic stroke related to HIV and SARS-COV-2 co-infection: A case report. J Func Vent Pulm 2024;46(15):59-63