
 English
English
 French
French
Pyothorax complicating cervical cellulitis of dental origin: A case report
Pyothorax compliquant une cellulite cervicale d'origine dentaire: À propos d'un cas
Maryem Hindi, Sàad Bounhar, Oussama Fikri, Lamyae Amro
Pneumology Department, Chu Mohammed VI
Labo LRMS, FMPM, UCA, Hospital Arrazi, Marrakech
Corresponding author:
Maryem Hindi. Pneumology Department, Chu Mohammed VI
Labo LRMS, FMPM, UCA, Hospital Arrazi, Marrakech
E-mail: hindi123maryem123@gmail.com
ABSTRACT
The most common type of cellulitis is the cervical-facial cellulitis, which is a serious and potentially life-threatening condition that can affect the face, neck, and the abdomen.
It can be treated with antibiotics and can be prevented from spreading by the proper anatomical continuity between these regions. Cervical and thoracic computed tomography is crucial in the assessment.
A double drainage of the cervical and thoracic regions with an antibiotic therapy directed against the aerobic and anaerobic germs is the standard treatment.
We present a case of 33-year-old smoker who developed pyothorax complicating cervical cellulitis of dental origin.
KEYWORDS: Cellulitis; Cervical-facial cellulitis; Drainage; Pyothorax.
RÉSUMÉ
Le type de cellulite le plus courant est la cellulite cervico-faciale, qui est une maladie grave et potentiellement mortelle qui peut affecter le visage, le cou et l'abdomen.
Elle peut être traitée avec des antibiotiques et sa propagation peut être évitée grâce à une bonne continuité anatomique entre ces régions. La tomodensitométrie cervicale et thoracique est cruciale dans l'évaluation.
Un double drainage des régions cervicale et thoracique avec une antibiothérapie dirigée contre les germes aérobies et anaérobies est le traitement de référence.
Nous présentons le cas d'une fumeuse de 33 ans ayant développé un pyothorax compliquant une cellulite cervicale d'origine dentaire.
MOTS CLÉS: Cellulite; Cellulite cervico-facial; Drainage; Pyothorax.
INTRODUCTION
Empyema thoracic, from the Greek, is defined as ‘‘pus in the chest, [1] is an accumulation of pus in the pleural space that can be confirmed through biochemical and/or microbiological tests. Descending necrotizing mediastinitis (DNM) is an acute and life-threating infection of the neck and mediastinum that originates from an oropharyngeal or cervical infection and spreads into the mediastinal spaces [2]. A mediastinal abscess can quickly spread into the mediastinal connective tissues, causing severe sepsis and an acute critical condition. Emergency surgical intervention, including wide drainage, is necessary to save patients from a critical state.
OBSERVATION
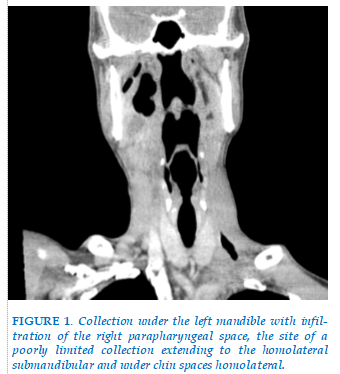
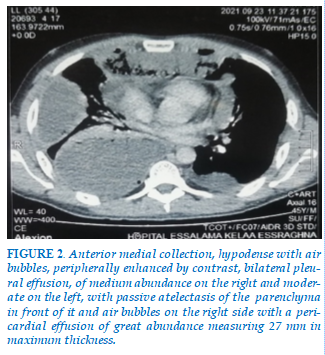
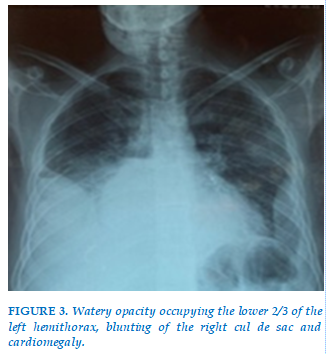
A 33 years old chronic smoker was admitted to the emergency room with septic shock, who was questioned and found to have dental pain and to be taking non-steroidal anti-inflammatory drugs. On physical examination, he was dyspneic, febrile with a trismus, poor oral hygiene, and moderate left submandibular non-fluctuant swelling that was firm, erythematous, and warm to palpation. The initial biological workup showed hyperleukocytosis, high CRP. The CT scan of the cervicothoracic cavity reveals a presence of a hypodense anterior medial collection which leaks, extends with a sub-mandibular collection (Figure 1), bilateral pleural effusion and pericardial effusion (Figure 2), hence the performance of a frontal thoracic radiograph, which showing pleurisy of moderate severity on the right and of low severity on the left (Figure 3).
In addition to resuscitative measures, treatment includes a thoracic drainage thoracic drainage with evacuation of two liters of pus and bacteriological samples, a probabilistic antibiotic therapy based on amoxicillin+clavulanic acid (1 g/8 hours) associated with 5-nitroimidazole (500 mg x 3/d) and gentamicin (160mg/d) readjusted according to the results of the antibiogram.
The patient’s evolution was favorable with improvement in both clinical and radiological symptoms (Figure 4).
DISCUSSION
Cervico-mediastinal cellulitis is a severe infection, sometimes necrotizing, whose diagnosis is difficult at an early stage. This pathology is characterized by the existence of an infectious process that develops at the level of the cellular cervical spaces and extends towards the mediastinum.
The dental or oropharyngeal infection spreads rapidly to the parapharyngeal space which is a real crossroads from which the extension can be extremely rapid: either through the retro visceral space called "danger space" [3]; or through the pre-tracheal space to the anterior mediastinum; or finally through the vascular gutters in about. This propagation is favored by gravity and negative intra thoracic pressure.
Other favorable factors such as diabetes, corticosteroids and immunosuppression have been reported. High risk factors for the development of DNM from deep neck infections include older age (> 65 years), cervical necrotizing fasciitis, involvement of 2 or more cervical spaces, the presence of comorbidities such as chronic renal failure, diabetes mellitus, cardiovascular and pulmonary diseases, C-reactive protein ≥30 mg/dL, and neutrophil to lymphocyte ratio ≥ 13.6-8. The paraclinical exploration is done essentially by the cervico-thoracic scanner. Once the diagnosis has been made and confirmed by CT scan, a probabilistic antibiotic therapy associated with resuscitation measures (vascular filling, correction of visceral failure), must be instituted immediately after bacteriological sampling from the primary infection site [4]. The principle of surgical treatment of MND is the evacuation of all purulent cervical and mediastinal collections, debridement and excision of necrotic tissue, drainage of the various residual cavities and treatment of the primary infection. The duration of antibiotic therapy varies according to the severity of the initial infection and, above all, the patient's progress [5]. The place of hyperbaric oxygen therapy is debated and has not been evaluated in a randomized fashion [4].
CONCLUSION
Descending necrotizing mediastinitis is a serious life-threatening complication that can occur following a common odontogenic infection. Despite advances in antibiotics, diagnostic imaging, and surgical management, the mortality rate remains significant. It is imperative that the practitioner managing patients with odontogenic infections be aware of this potentially fatal complication. The prognosis is essentially related to the terrain; the and the effectiveness of the initial treatment.
CONFLIT D'INTERETS
Aucun.
REFERENCES
FIGURES

REFERENCES
ARTICLE INFO DOI: 10.12699/jfvpulm.15.46.2024.68
Conflict of Interest
Non
Date of manuscript receiving
28/03/2024
Date of publication after correction
26/06/2024
Article citation
Maryem Hindi, Sàad Bounhar, Oussama Fikri, Lamyae Amro. Pyothorax complicating cervical cellulitis of dental origin: A case report. J Func Vent Pulm 2024;46(15):68-70