 English
English
 French
French
Endoscopic septoplasty and turbinate surgery for obstructive sleep apnea syndrome at 199 Hospital
Septoplastie endoscopique et chirurgie des cornets pour le syndrome d'apnée obstructive du sommeil à l'Hôpital 199
Le Van Diep¹, Nguyen Thi Xuan², Vo Thi Hong Huong2, Tran Huu Khanh Duy², Tran Thi Mong Bo², Sy Duong-Quy3,4, Tran Quang Phap², Quach Huu Trung²
1: Department of Otolaryngology - 199 Hospital. Da Nang city - Vietnam
2: Department of Sleep Medicine - 199 Hospital. Da Nang city - Vietnam
3: Department of Outpatients Consultation - 199 Hospital. Da Nang city - Vietnam
4: Sleep Lab Center - Vietnam Society of Sleep Medicine. Lam Dong Medical College. Dalat - Vietnam
Corresponding author:
Le Van Diep. ENT Department. 199 Hospital. 216 Nguyen Cong Tru, Son Tra District, Da Nang City.
E-mail: bsdiep199@gmail.com
ABSTRACT
Obstructive sleep apnea syndrome (OSAS) is becoming increasingly common, especially due to the rising obesity epidemic, and has significant social, health, and economic impacts. The gold standard for treating moderate to severe OSA is continuous positive airway pressure (CPAP). However, compliance rates with CPAP can be low. Methods to improve patient tolerance to CPAP, along with alternative non-surgical and surgical treatments, are being explored. All patients who fail CPAP therapy should undergo formal upper airway evaluation by an otolaryngologist to identify specific causes and consider targeted surgical therapies. Patient selection is critical to ensuring successful outcomes. A multidisciplinary team is essential for managing these patients.
We present a case of a patient with obstructive sleep apnea syndrome (OSAS) who experienced dramatic clinical improvement after undergoing surgery to correct a deviated nasal septum and turbinate hypertrophy. The subjective improvement was associated with a decrease in the number and duration of obstructive apnea episodes observed during a sleep study. Due to its simplicity and low complication rate, we suggest that septoplasty should be further considered as a treatment option for this condition.
KEYWORDS: Obstructive sleep apnea (OSA); Continuous positive airway pressure (CPAP); Compliance; Failure; Surgery.
RÉSUMÉ
Le syndrome d'apnée obstructive du sommeil (AOS) devient de plus en plus fréquent, notamment en raison de l'épidémie croissante d'obésité, et a des impacts sociaux, sanitaires et économiques significatifs. Le traitement de référence pour l'AOS modérée à sévère est la pression positive continue (PPC). Cependant, les taux d'adhérence au PPC peuvent être faibles. Des méthodes pour améliorer la tolérance des patients au PPC, ainsi que des traitements alternatifs non chirurgicaux et chirurgicaux, sont explorés. Tous les patients qui échouent à la thérapie PPC doivent subir une évaluation formelle des voies aériennes supérieures par un oto-rhino-laryngologiste afin d'identifier des causes spécifiques et de considérer des thérapies chirurgicales ciblées. La sélection des patients est cruciale pour garantir des résultats positifs. Une équipe multidisciplinaire est essentielle pour la prise en charge de ces patients.
Nous présentons le cas d'un patient atteint d’AOS qui a connu une amélioration clinique spectaculaire après avoir subi une intervention chirurgicale pour corriger une déviation de la cloison nasale et une hypertrophie des cornets. L'amélioration subjective était associée à une diminution du nombre et de la durée des épisodes d'apnée obstructive observés lors d'une étude du sommeil. En raison de sa simplicité et de son faible taux de complications, nous suggérons que la septoplastie soit davantage envisagée comme une option thérapeutique pour cette condition
MOTS CLÉS: Apnée obstructive du sommeil (AOS); Pression positive continue des voies respiratoires (PPC); Conformité; Échec; Chirurgie.
INTRODUCTION
Obstructive sleep apnea (OSA) is a common medical condition affecting at least 4-8% of the adult population and is receiving increasing attention from the public [1]. OSA can occur at any age and is characterized by the collapse of the upper airway at the oropharyngeal region during sleep, leading to ineffective respiratory effort, reduced gas exchange in the blood, and sleep disruption. The signs, symptoms, and consequences of OSA include sleep fragmentation, intermittent hypoxia due to hypopnea or apnea episodes, increased blood CO2 levels, changes in negative chest pressure, and increased sympathetic activity [1].
Obstructive sleep apnea is the leading cause of daytime sleepiness, which increases the risk of motor vehicle accidents, work difficulties, and sexual dysfunction. Relationships with family members may also be negatively affected due to the patient's snoring and restless sleep.Patients with untreated OSA who have normal blood pressure are likely to develop hypertension within the next five years. Nightly hypoxia and sleep disruption are associated with an increased risk of cardiovascular diseases, including heart failure, atrial fibrillation, and other arrhythmias, fatty liver disease, and stroke. The risk of stroke and mortality increases even when other risk factors, such as hypertension and diabetes, are controlled.However, the impact of OSA on these common disorders has not been adequately assessed. Many reports suggest that more than 85% of individuals with symptoms of OSA have never been diagnosed, and the majority of cardiologists in the U.S. are still not fully aware of the cardiovascular consequences of OSA[5][8] [9].Treatment options for OSA in adults include weight loss, positional therapy (side-sleeping), and CPAP for severe cases. Additionally, surgical treatment for nasal or pharyngeal obstruction, such as uvulopalatopharyngoplasty (UPPP) or septoplasty and turbinate surgery, can be considered. 199 Hospital – under the Ministry of Public Security – has recently established a standard sleep study room to diagnose and provide initial treatment for obstructive sleep apnea syndrome and other sleep disorders. In this report, we present a case of surgical septoplasty and turbinate surgery for the treatment of obstructive sleep apnea.
CASE REPORT
A 34-year-old male patient with a history of hypertension for the past five years presented. He frequently experienced nasal congestion, more severe on the left
side, accompanied by headaches, facial pressure, frequent throat clearing, snoring, sleep apnea, poor sleep quality with frequent awakenings (5-6 times per night), dry throat, sore throat upon waking, daytime fatigue, and drowsiness. Clinical examination revealed a retruded chin, neck circumference measurement, Mallampati score of IV, and abdominal circumference. The patient had a deviated nasal septum with a septal spur in contact with the inferior turbinate on the left side; both inferior turbinates were hypertrophied, and there was mucous discharge in the nasal cavity. There were no significant bony changes in the uncinate process or ethmoid bulla. The nasal mucosa was pale, swollen, and irregular. Imaging results: Maxillofacial CT scan showed thickened mucosa in the maxillary and ethmoid sinuses on both sides, along with septal deviation and a spur causing contact with the inferior turbinate and bilateral turbinate hypertrophy.
Nasal Endoscopy: Deviated septal spur with hypertrophy of the inferior turbinate. Sleep Study:
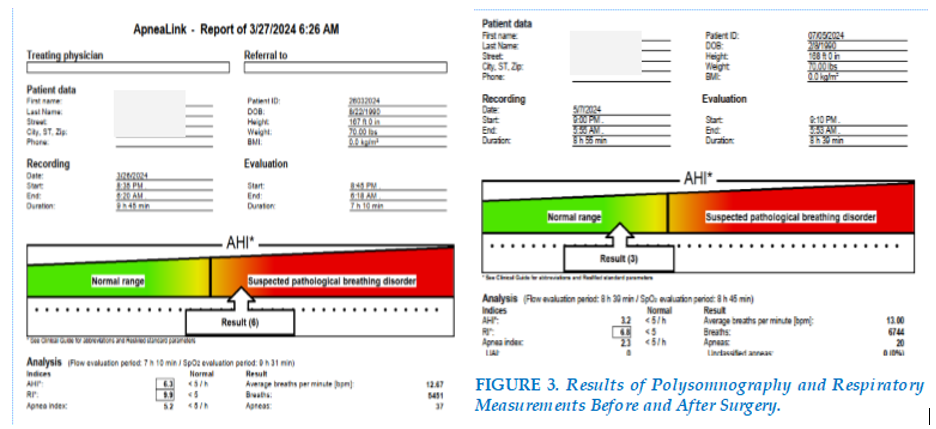
The average apnea-hypopnea index (AHI) was 6.3 episodes per hour; snoring index was 251 episodes per hour; average SpO2 was 96%, with a minimum of 85%. Lateral sleeping position was recommended. FIGURE 2
The patient was diagnosed with obstructive sleep apnea syndrome, deviated nasal septum, and hypertrophy of the inferior turbinate. The chosen treatment method was endoscopic surgery to correct the nasal septum and turbinate hypertrophy.
Surgical Procedure: Using a 0-degree 3.7mm endoscope, septoplasty and turbinoplasty were performed under general anesthesia with intubation, followed by the placement of Merocel in both nasal cavities for 24 hours.
Postoperative Care: After surgery, the patient received antibiotics, anti-inflammatory drugs, antihistamines, and daily wound care, along with nasal irrigation using a specialized solution. The patient was discharged after 3 days of treatment, with slight nasal congestion remaining.
One-month Follow-up: The patient was in good health, breathing easily through the nose, sleeping well at night, and waking up only 1-2 times per night (compared to 5-6 times before surgery). Morning symptoms such as sore throat, dryness, and fatigue had resolved.
Examination: The nasal passages were clear, the septum was straight, the inferior turbinate had reduced in size, and the nasal mucosa appeared smooth and healthy.
Sleep Study Results: The apnea-hypopnea index (AHI) was 3.2 episodes per hour, average SpO2 was 96%, and the lowest SpO2 was 89%. The snoring index was 270 episodes per hour. The sleep study results were normal. FIGURE 3
DISCUSSION
Obstructive sleep apnea (OSA) is diagnosed according to the 2024 ICSD3 criteria, version 3, as follows:
Having ≥ 5 obstructive respiratory events/hour (measured by sleep time with PSG or recording time with HSAT), where obstructive events are predominant and associated with one or more of the following symptoms or conditions:
Having ≥ 15 obstructive respiratory events/hour, regardless of associated symptoms or comorbid conditions.
Among the available treatment options for OSA, CPAP (Continuous Positive Airway Pressure) remains the first choice for patients with moderate to severe forms of the disease. However, some patients are intolerant to this treatment, citing discomfort with the mask, while others are unwilling to sleep while connected to a mechanical device. In these cases, surgical treatment should be considered, with the goal of eliminating the cause of upper airway obstruction, especially in the pharyngeal area. CPAP was first developed in the 1980s with the basic principle of applying continuous mild air pressure to act as a stent to keep the airway open, thereby addressing collapsed or obstructed anatomical areas.
Many studies demonstrate the benefits of CPAP in improving symptoms and long-term outcomes.
By preventing airway collapse and vibration, CPAP eliminates snoring and enhances the quality of sleep for bed partners, along with improving nighttime symptoms like choking, waking up, and nocturia. Moreover, daytime sleepiness improves both subjectively and objectively, leading to enhanced concentration. CPAP has consistently demonstrated improvement in OSA-specific quality of life studies. From a long-term cardiovascular risk perspective, CPAP has shown positive impacts, such as randomized trials indicating reductions in blood pressure. Interestingly, meta-analyses of these studies suggest that non-compliance, especially when CPAP is used for less than 4 hours per night, may be a confounding factor, underscoring the importance of adherence. Long-term effects on stroke risk, triglyceride levels, and insulin resistance remain unclear.
CPAP continues to be the treatment of choice for moderate to severe OSA, according to NICE guidelines. However, adherence rates can be poor. Additionally, anatomical factors can interfere with CPAP effectiveness, such as nasal septal deviation, nasal valve collapse, enlarged turbinates, and pharyngeal hypertrophy. Beyond structural issues requiring surgery, some of these conditions involve an inflammatory component, such as hypertrophic turbinates, which can be treated medically (e.g., topical nasal steroids, antihistamines, or saline irrigation), potentially improving CPAP compliance with reduced pressure requirements, though rarely resolving OSA entirely.
CPAP adherence rates range from 40 - 85% [1]. In the U.S., compliance is arbitrarily defined as use for more than 4 hours per night on more than 70% of nights. This threshold does not correlate with an absolute effectiveness level - put simply, the more CPAP is used, the better the outcomes regarding symptom relief, life signs, and long-term cardiovascular and blood pressure metrics. Therefore, there is significant interest in improving CPAP system tolerability. Commonly cited side effects include dermatitis, rhinitis, epistaxis, nasal discomfort, nasal congestion, mask leaks, aerophagia, barotrauma, and claustrophobia. Thus, there may be specific ENT factors contributing to CPAP failure, particularly involving the nasal and paranasal sinus cavities. Nasal conditions include anatomical, physiological, and pathological factors. Anatomical considerations include nasal septal deviation, external framework deformities, valve collapse, enlarged turbinates, and pharyngeal conditions causing choanal obstruction, which can be corrected surgically. Physiological conditions are common and include allergic or vasomotor rhinitis, which patients need proper education and counseling for, skin allergy testing, advice on allergen avoidance, and treatment with antihistamines and nasal steroids. CPAP rhinitis is caused by inflammatory changes in the nasal mucosa due to prolonged high air pressure - this also requires treatment with saline rinses and nasal steroids. Pathological processes like sinusitis and nasal polyps are often problematic and can be missed during routine respiratory exams, as they are better evaluated with rigid and flexible endoscopy in ENT outpatient settings. These can be effectively treated with medical or surgical interventions, such as endoscopic sinus surgery. Addressing these factors may improve CPAP compliance through reduced pressure requirements, but rarely on their own can they resolve OSA.
Surgical treatment decisions should be based on proper patient selection, with clear preoperative consent and explanation of associated risks. It is important to counsel patients about the aim of the surgery and that CPAP is the gold standard treatment for OSA. The reality that surgery may cure the condition or simply assist in facilitating CPAP use must be clarified. According to Nakata et al., reducing nasal resistance is directly associated with improved quality of life and reduced daytime sleepiness. Notably, nasal surgery reduces resistance and may improve CPAP acceptance but does not significantly improve the AHI [6]. Friedman et al.[4] studied 49 patients with OSA and found that the respiratory disturbance index (RDI) worsened in those with mild OSA who only underwent nasal surgery. This study demonstrated that nasal breathing improved in 49 patients (98%), and snoring was reduced or eliminated in 17 patients (34%), while the remaining 33 patients (66%) did not experience any significant change in their snoring. Daytime energy levels increased in 39 patients (78%) and either did not change or worsened in 11 patients (22%). The CPAP pressure needed to correct OSA decreased after nasal surgery (P < 0.01). However, patients with mild OSA showed a significant worsening of the RDI (P < 0.05), while SpO2 levels improved in the moderate OSA group (P < 0.05). In patients with severe OSA, both the RDI and LSaO2 remained unchanged, but the CPAP pressure required to alleviate obstruction decreased after surgery (P < 0.01). Victores et al. [8] demonstrated that 24 OSA patients who only underwent nasal surgery did not show any significant changes in drug-induced sleep endoscopy findings before and after surgery. Nasal surgery alone did not improve the apnea index, arousal index, or apnea-hypopnea index (AHI) in 22 OSA patients [2]. The primary goal of surgery is to improve the size of the upper airway, thereby reducing obstruction.
Surgical interventions can be considered adjunctive (reducing CPAP pressure requirements and improving compliance) or curative, and can be categorized into minimally invasive versus radical approaches, or single anatomical site versus multilevel approaches.
Surgical options include septoplasty, nasal valve surgery, functional endoscopic sinus surgery, and turbinate reduction. All aim to address sources of anatomical obstruction. It is worth remembering that nasal surgery rarely eliminates the need for CPAP but can facilitate its use and thus improve compliance. A meta-analysis confirmed this finding, showing that nasal surgery can reduce CPAP pressure requirements and improve comfort [9]. Although nasal surgery for addressing nasal obstruction significantly improves quality of life, this improvement does not strongly correlate with noticeable improvements in polysomnography data [9]. It is also important to note that more than 50% of CPAP users report nasal symptoms, including nasal congestion, rhinorrhea, and dryness [10]. In our patient, endoscopic septoplasty and turbinate reduction have proven to be effective in treating obstructive sleep apnea syndrome (OSAS). Clinically, the patient has shown significant improvement, with resolution of nasal congestion, improved sleep, reduced nighttime awakenings, and snoring, and importantly, no morning symptoms. This is supported by respiratory polysomnography, with an AHI of 3.2. This method addresses anatomical obstacles causing sleep apnea, thereby improving airway patency and enhancing both sleep quality and the patient's overall quality of life. The endoscopic method allows for precise and less invasive manipulation compared to traditional open surgery. This leads to less tissue damage, reduced postoperative pain, and faster recovery. Conservative treatments such as lifestyle changes, positional therapy, and CPAP are often prioritized due to their non-invasive nature and lower costs. However, these methods may not be sufficiently effective for patients with significant anatomical obstacles. CPAP, while effective, can cause discomfort and inconvenience, leading to poor compliance. Laser and radiofrequency technologies offer an intermediate, less invasive approach compared to surgery but may not yield long-lasting results. A comprehensive care model involving sleep specialists, ENT specialists, and respiratory specialists can provide a holistic approach to managing OSAS [11,12]. This includes clinical evaluation, ENT and respiratory examination, polysomnography, individualized treatment planning, and follow-up for treatment adherence.
CONCLUSION
Obstructive Sleep Apnea (OSA) has become the most prevalent and significant sleep disorder, closely associated with several systemic changes, primarily cardiovascular complications. CPAP remains the treatment of choice for moderate to severe OSA, as recommended by NICE guidelines. However, the most definitive and effective method for treating moderate to severe OSA is surgical correction. Specifically, septoplasty and turbinate surgery have shown good results in treating nasal-related obstructive sleep apnea. We believe it is necessary to continue this research with a larger number of patients and longer follow-up periods. We recommend that all patients who fail CPAP treatment be referred to an ENT specialist for evaluation.
CONFLICT OF INTEREST: Non.
REFERENCE
| 1. Duong-Quy, S., Nguyen-Huu, H., Hoang-Chau-Bao, D et al.Personalized medicine and obstructive sleep apnea. Journal of Personalized Medicine 2022, 12(12), 2034. |
| 2. Choi JH, Kim EJ, Kim YS, et al. Effectiveness of nasal surgery alone on sleep quality, architecture, position, and sleep-disordered breathing in obstructive sleep apnea syndrome with nasal obstruction. Am J Rhinol Allergy. 2011;25(5):338–41. Nasal surgery does improve sleep architecture and sleep quality, but falls short in improving apnea indices. |
| 3. Feitoza CC, da-Silva MC, Nascimento YL, Leite ES, Pereira CV, Patrocínio LG. Surgical treatment of a Pattern I Obstructive Sleep Apnea Syndrome individual - clinical case report. Sleep Sci. 2017 Oct-Dec;10(4):168-173. doi: 10.5935/1984-0063.20170029. PMID: 29410749; PMCID: PMC5760051. |
| 4. Friedman M, Tanyeri H, Lim JW, et al. Effect of improved nasal breathing on obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000;122(1):71–4. |
| 5. Heimer D, Scharf SM, Lieberman A, Lavie P. Sleep apnea syndrome treated by repair of deviated nasal septum. Chest. 1983 Aug;84(2):184-5. |
| 6. Nakata S, Noda A, Yagi H, et al. Nasal resistance for determinate factor of nasal surgery in CPAP failure patients with obstructive sleep apnea syndrome. Rhinology. 2005;43:296–9. |
| 7. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2024;146(5):1387-94. |
| 8. Victores AJ, Takashima M. Effects of nasal surgery on the upper airway: a drug-induced sleep endoscopy study. Laryngoscope. 2012;122(11):2606–10. |
| 9. Pang, K.P. The Role of Nasal Surgery in the Treatment of OSA. Curr Otorhinolaryngol Rep 1, 20–24 (2013). |
| 10. Dinh-Thi-Dieu, H., Vo-Thi-Kim, A., Tran-Van, H.,et al. Efficacy and adherence of auto-CPAP therapy in patients with OSA:a prospective study. Multidisciplinary respiratory medicine 2020, 15(1). |
| 11. Tran-Minh, D., Phi-Thi-Quynh, A., Nguyen-Dinh, et al. Efficacy of OSA treatment by antileukotriene receptor and surgery therapy in children with adenotonsillar hypertrophy. Frontiers in Neurology 2022, 13, 1008310. |
| 12. Duong-Quy, S., Nguyen-Ngoc-Quynh, L., et al.. ‘Personalized medicine’: phenotyping pediatric obstructive sleep apnea. Current Opinion in Pulmonary Medicine, 10-1097. |
TABLE - FIGURES

REFERENCE
| 1. Duong-Quy, S., Nguyen-Huu, H., Hoang-Chau-Bao, D et al.Personalized medicine and obstructive sleep apnea. Journal of Personalized Medicine 2022, 12(12), 2034. |
| 2. Choi JH, Kim EJ, Kim YS, et al. Effectiveness of nasal surgery alone on sleep quality, architecture, position, and sleep-disordered breathing in obstructive sleep apnea syndrome with nasal obstruction. Am J Rhinol Allergy. 2011;25(5):338–41. Nasal surgery does improve sleep architecture and sleep quality, but falls short in improving apnea indices. |
| 3. Feitoza CC, da-Silva MC, Nascimento YL, Leite ES, Pereira CV, Patrocínio LG. Surgical treatment of a Pattern I Obstructive Sleep Apnea Syndrome individual - clinical case report. Sleep Sci. 2017 Oct-Dec;10(4):168-173. doi: 10.5935/1984-0063.20170029. PMID: 29410749; PMCID: PMC5760051. |
| 4. Friedman M, Tanyeri H, Lim JW, et al. Effect of improved nasal breathing on obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000;122(1):71–4. |
| 5. Heimer D, Scharf SM, Lieberman A, Lavie P. Sleep apnea syndrome treated by repair of deviated nasal septum. Chest. 1983 Aug;84(2):184-5. |
| 6. Nakata S, Noda A, Yagi H, et al. Nasal resistance for determinate factor of nasal surgery in CPAP failure patients with obstructive sleep apnea syndrome. Rhinology. 2005;43:296–9. |
| 7. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2024;146(5):1387-94. |
| 8. Victores AJ, Takashima M. Effects of nasal surgery on the upper airway: a drug-induced sleep endoscopy study. Laryngoscope. 2012;122(11):2606–10. |
| 9. Pang, K.P. The Role of Nasal Surgery in the Treatment of OSA. Curr Otorhinolaryngol Rep 1, 20–24 (2013). |
| 10. Dinh-Thi-Dieu, H., Vo-Thi-Kim, A., Tran-Van, H.,et al. Efficacy and adherence of auto-CPAP therapy in patients with OSA:a prospective study. Multidisciplinary respiratory medicine 2020, 15(1). |
| 11. Tran-Minh, D., Phi-Thi-Quynh, A., Nguyen-Dinh, et al. Efficacy of OSA treatment by antileukotriene receptor and surgery therapy in children with adenotonsillar hypertrophy. Frontiers in Neurology 2022, 13, 1008310. |
| 12. Duong-Quy, S., Nguyen-Ngoc-Quynh, L., et al.. ‘Personalized medicine’: phenotyping pediatric obstructive sleep apnea. Current Opinion in Pulmonary Medicine, 10-1097. |
ARTICLE INFO DOI: 10.12699/jfvpulm.15.47.2024.38
Conflict of Interest
Non
Date of manuscript receiving
20/06/2024
Date of publication after correction
25/11/2024
Article citation
Le Van Diep, Nguyen Thi Xuan, Vo Thi Hong Huong, Tran Huu Khanh Duy, Tran Thi Mong Bo, Sy Duong-Quy, Tran Quang Phap, Quach Huu Trung. Endoscopic septoplasty and turbinate surgery for obstructive sleep apnea syndrome at 199 Hospital. J Func Vent Pulm 2024;47(15):38-42