
 English
English
 French
French
Isolated idiopathic intracranial hypertension as a neurological manifestation of COVID-19: A case report
Hypertension intracrânienne idiopathique isolée presentée comme manifestation neurologique de la COVID-19: Un rapport de cas
Mohamed Amine Mnaili 1,2, Zakaria Toufga 3, Abdennasser El kharras 3, Ahmed Bourazza 4
1: Neurology Departement, Agadir Military Hospital, Agadir, Morocco
2: University of Hassan II, Casablanca, Morocco
3: Radiology Departement, Agadir Military Hospital, Agadir, Morocco
4: Neurology Departement, Rabat Military Hospital, Rabat, Morocco
Corresponding author:
Mnaili Mohamed Amine
Agadir Military Hospital - Morocco
E-mail: Aminemed08@gmail.com
DOI: 10.12699/jfvpulm.15.47.2024.56
ABSTRACT
Headache is a frequent complaint in COVID-19 while intracranial hypertension leading to acute vision loss is unusual. A 23-years-old female presented with persistent headache and vision loss and had been diagnosed with COVID‑19 15 days ago.
Investigations suggested Covid 19 associated intracranial hypertension. She improved with medical management. She had significant recovery in vision during follow up period.
Persistent headache in Covid 19 should have a high index of suspicion for idiopathic intracranial hypertension to avoid irreversible vision loss.
KEYWORDS: Covid 19; Idiopathic intracranial hypertension; Vision loss.
RÉSUMÉ
Les céphalées sont fréquemment rencontrées lors du COVID-19, tandis que l'hypertension intracrânienne est inhabituelle. Une femme de 23 ans ayant reçu un diagnostic de COVID-19 15 jours avant son admission aux urgences pour des céphalées persistantes avec diminution de l'acuité visuelle.
Le diagnostic du’ne hypertension intracrânienne associée au Covid 19 a été retenu . Elle s'est améliorée grâce à une prise en charge médicale. Elle a eu une récupération significative de sa vision au cours de la période de suivi.
Les maux de tête persistants dans le cadre du Covid 19 devraient faire évoquer le diagnostic d’hypertension intracrânienne idiopathique afin d’éviter une perte de vision irréversible
MOTS CLÉS: Covid 19; Hypertension intracrânienne idiopathique; Perte de vision.
INTRODUCTION
Covid −19 is the current health problem all over the world. Commonly, it manifests with respiratory symptoms but neuro-ophthalmic presentations have also been found. Headache is one of the important clinical feature of Covid 19 however; persistent headache is also the main feature of idiopathic intracranial hypertension.
This case was presented to overview idiopathic intracranial hypertension (IIH) as a rare neurological presentation of SARS-CoV2 infection that may be un/misdiagnosed and to increase the suspicion of clinicians for early diagnosis of COVID-19.
CASE PRESENTATION
A 23-year-old man without history of headache and no past medical history was admitted to the emergency room with the symptoms including anorexia, nausea, vomiting, fever, headache and diplopia. Nausea and vomiting started over the past ten days before admission as the initial symptoms. Five days after the presentation of initial symptoms mild diplopia were developed.
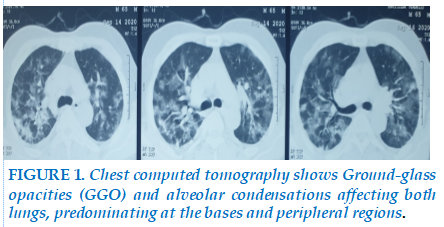
She had been diagnosed with COVID‑19 15 days ago with nasopharyngeal PCR (polymerase chain reaction) positive test result following 3 days of upper respiratory tract infection symptoms and fever up to 38°C. She had used hydroxychloroquine and favipiravir for 5 days and recovered without further complaints. Chest computed tomography showed round ground-glass opacities in both lungs (Figure 1).
Patient had body mass index of 21 with normal physical examination. ENT examination didn’t find any abnormality. Ophthalmic examination found 6/36 visual acuity in both eyes with normal pupillary reactions. Retinoscopy found Frisen grade 4 papilloedema in both optic discs. Neurology examination was also found normal. Cerebrospinal fluid pressure was more than 35cmH2O while biochemical analysis was normal. D-dimers levels were less than 1.0ug/ml FEU while serum ferritin levels were 171.0ng/ml. A possibility of intracranial hypertension was kept and managed accordingly.
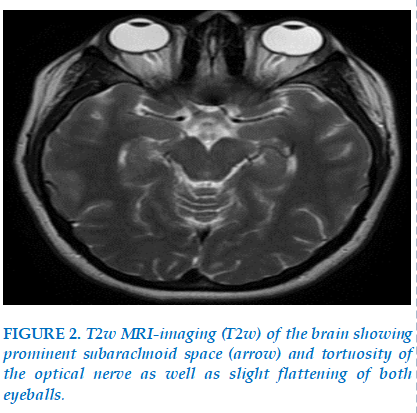
Magnetic resonance imaging of brain (Figue 2) found prominent subarachnoid space and tortuosity of the optical nerve as well as slight flattening of both eyeballs.
Laboratory tests including complete blood picture, liver and kidney function tests, serum electrolytes, thyroid-stimulating hormone (TSH), autoimmune and coagulation profles were also done to rule out secondary causes of intracranial hypertension. All blood tests and CSF analysis results came within normal ranges.
The clinical history and examination, and radiology didn’t find any other cause of intracranial hypertension. Keeping this in view, diagnosis of Covid-19 induced intracranial hypertension was made.
The carbonic anhydrase inhibitor, acetazolamide, was prescribed to the patient at a dose of 250 mg every 6 h and stepped up after one week to 500 mg tid, after which the patient reported total resolution of his symptoms and at 5 weeks of follow-up, the patient’s papilledema grade improved from grade II to grade I.
DISCUSSION
IIH is defined as an increase in intracranial pressure (ICP) without hydrocephalus, any mass lesions to be present, and a normal composition of CSF [1].
The pathogenic mechanism underlying idiopathic intracranial hypertension remains unclear, but the proposed mechanisms include abnormalities in cerebral venous outfow, alterations in absorption or production of CSF, low-grade infammation, and intracranial vascular clotting [2]. It is predominantly found in young, obese, females in child bearing age.
Clinically presentation includes (in order of decreasing incidence) headache that increases on coughing or Valsalva manoeuvre, transient visual disturbances on bending or standing, pulsatile tinnitus, back pain, dizziness, neck pain, visual loss, cognitive disturbances, radicular pain and horizontal diplopia [3]. Fundus examination shows papilledema that warrants neuroimaging (CT/MRI with angiography) to excludes tumour or other causes of increased intracranial pressure. Neuroimaging may show empty sella, flattening of posterior aspect of orbital globe, distension of perioptic subarchnoid space, tortuous optic nerve, attenuation of cerberovenous sinuses and stenosis of transverse sinus. Normal cerebrospinal analysis with pressure more that 25 cm H2O makes the diagnosis of idiopathic intracranial hypertension.
The mechanism of IHT in COVID‑19 can be variable and controversial.
SARS-CoV-2 may access the CNS through different hypothesized mechanisms. The main theory is retrograde axonal transport via sensory nerve endings embedded in the olfactory region. Another possible way is through angiotensin-converting enzyme 2 (ACE2) expressed in vascular endothelial cells, which mediates virus entry across the blood–brain barrier (BBB) [4].
How COVID-19 infection can precipitate isolated intracranial hypertension is a matter of discussion. Silva et al [5] speculated that low-grade inflammation together with the hypercoagulable state attributed to SARS-CoV-2 infection could result in lower CSF absorption. On the other hand, Wostyn et al. [6] reported that SARS-CoV-2 infection might contribute to decreased CSF drainage via the cribriform plate and nasal mucosa as a result of olfactory epithelium destruction and olfactory sensory neurons loss which could also be a credible mechanism of anosmia in infected individuals [7].
The latter view could be a reliable mechanism of intracranial hypertension in our case.
Our patient was in this high‑risk group but had no history of disturbing headache, symptoms, and signs of IHT, and she had no ophthalmic complaints before COVID‑19.
Treatment and prognosis of IHT have not been discussed as a different entity in COVID‑19 patients in the literature. We plannedthe treatment asdescribedforidiopathic IHTcases [8].
CONCLUSION
COVID‑19 could be a causative or precipitating factor forI HT, especially in high‑risk groups, even in the late phases of the disease. This case scenario implies that SARS-CoV-2 infection could be a precipitating factor for isolated intracranial hypertension. Severe headache in subjects who have recovered from SARS-CoV-2 infection prompts investigational work-up for intracranial hypertension.
ACKNOWLEDGMENTS
Our warmest thanks to the patient for allowing us to report this case
FINANCIAL DISCLOSURE
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST
The authors report no conflict of interest.
INFORMED CONSENT
Informed consent to write and publish the case was obtained from the patients.
REFERENCE
| 1. Sylaja PN, Ahsan Moosa NV, Radhakrishnan K, Sankara Sarma P, Pradeep Kumar S. Differential diagnosis of patients with intracranial sinus venous thrombosis related isolated intracranial hypertension from those with idiopathic intracranial hypertension. J Neurol Sci 2003;215:9—12. |
| 2. Mollan SP, Ali F, Hassan-Smith G, Botfeld H, Friedman DI, Sinclair AJ (2016) Evolving evidence in adult idiopathic intracranial hypertension: pathophysiology and management. J Neurol Neurosurg Psyc 87:982 |
| 3. Wakerley BR, Mollan SP, Sinclair AJ (2020) Idiopathic intracranial hypertension: update on diagnosis and management. Clin Med (Lond) 20:384–388 |
| 4. Generoso JS, Barichello de Quevedo JL, Cattani M, Lodetti BF, Sousa L, Collodel A (2021) Neurobiology of COVID-19: how can the virus afect the brain? |
| 5. Silva MTT, Lima MA, Torezani G, Soares CN, Dantas C, Brandão CO et al (2020) Isolated intracranial hypertension associated with COVID-19. Cephalalgia Internat J Headache 40:1452–1458 |
| 6. Wostyn P (2021) COVID-19 and chronic fatigue syndrome: is the worst yet to come? Med Hypotheses 146:110469 |
| 7. Butowt R, von Bartheld CS (2020) Anosmia in COVID-19: Underlying mechanisms and assessment of an olfactory route to brain infection. Neuroscientist. 1073858420956905 |
| 8. Markey KA, Mollan SP, Jensen RH, Sinclair AJ. Understanding idiopathic intracranial hypertension: Mechanisms, management, and future directions. Lancet Neurol 2016;15:78‑91. |
TABLE - FIGURES
REFERENCE
| 1. Sylaja PN, Ahsan Moosa NV, Radhakrishnan K, Sankara Sarma P, Pradeep Kumar S. Differential diagnosis of patients with intracranial sinus venous thrombosis related isolated intracranial hypertension from those with idiopathic intracranial hypertension. J Neurol Sci 2003;215:9—12. |
| 2. Mollan SP, Ali F, Hassan-Smith G, Botfeld H, Friedman DI, Sinclair AJ (2016) Evolving evidence in adult idiopathic intracranial hypertension: pathophysiology and management. J Neurol Neurosurg Psyc 87:982 |
| 3. Wakerley BR, Mollan SP, Sinclair AJ (2020) Idiopathic intracranial hypertension: update on diagnosis and management. Clin Med (Lond) 20:384–388 |
| 4. Generoso JS, Barichello de Quevedo JL, Cattani M, Lodetti BF, Sousa L, Collodel A (2021) Neurobiology of COVID-19: how can the virus afect the brain? |
| 5. Silva MTT, Lima MA, Torezani G, Soares CN, Dantas C, Brandão CO et al (2020) Isolated intracranial hypertension associated with COVID-19. Cephalalgia Internat J Headache 40:1452–1458 |
| 6. Wostyn P (2021) COVID-19 and chronic fatigue syndrome: is the worst yet to come? Med Hypotheses 146:110469 |
| 7. Butowt R, von Bartheld CS (2020) Anosmia in COVID-19: Underlying mechanisms and assessment of an olfactory route to brain infection. Neuroscientist. 1073858420956905 |
| 8. Markey KA, Mollan SP, Jensen RH, Sinclair AJ. Understanding idiopathic intracranial hypertension: Mechanisms, management, and future directions. Lancet Neurol 2016;15:78‑91. |
ARTICLE INFO DOI: 10.12699/jfvpulm.15.47.2024.56
Conflict of Interest
Non
Date of manuscript receiving
20/06/2024
Date of publication after correction
28/11/2024
Article citation
Mohamed Amine Mnaili , Zakaria Toufga , Abdennasser El kharras , Ahmed Bourazza. Isolated idiopathic intracranial hypertension as a neurological manifestation of COVID-19: A case report. J Func Vent Pulm 2024;47(15):56-58