 English
English
 French
French
Patient presenting aspergilloma in combination with squamous cell carcinoma of the lung
Patient présentant un aspergillome en combinaison avec un carcinome épidermoïde du poumon
Biborchi, H. Naguyeh, H. Yassine, M. Ijim, O. Fikri, L. Amro
Department of Respiratory Medicine, Arrazi Hospital, Mohammed VI University Hospital Center
LRMS Laboratory, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech, Morocco
Corresponding author:
Houssam Biborchi. Department of Respiratory Medicine, Arrazi Hospital, Mohammed VI University Hospital Center
E-mail: biborchihoussam@gmail.com
ABSTRACT
Endobronchial and intracavitary pulmonary aspergilloma can mimic bronchial neoplasia clinically and radiologically, can remain asymptomatic or present with hemoptysis, which can be life-threatening so a systematic search for an association is imperative. A confirmed association completely changes the prognosis and the therapeutic approach.
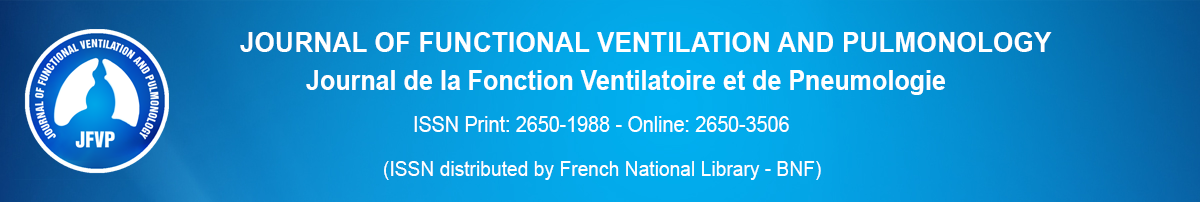
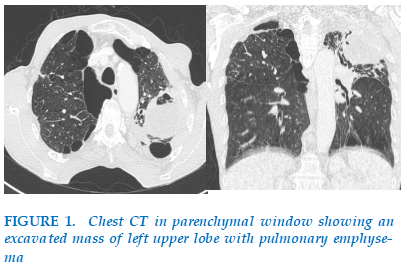
A 62-year-old male patient, former smoker at 40 packs/year and chronic cannabis user, presenting for 6 months with left chest pain of progressive aggravation associated with cervicobrachial neuralgia, The evolution was marked by the appearance of dyspnea on exertion 1 month before his admission associated with a single episode of hemoptysis and weight loss. On physical examination, he appeared with normal findings on chest, cardiovascular, abdominal and neurologic examinations. Chest radiography revealed a mass in the left upper lung zone, CT shows excavated mass in the posterior segment of the left upper lung lobe measuring 10 cm with necrotic lesions.
Aspergilloma can resemble to an endobronchial carcinoma clinically and radiologically. Lung carcinoma may be masked by a covering of fungus and fibrin.
KEYWORDS: Aspergilloma; Endobronchial; Intracavitary; Bronchial neoplasia.
RÉSUMÉ
L'aspergillome endobronchique et intracavitaire peut imiter cliniquement et radiologiquement une néoplasie bronchique, peut rester asymptomatique ou se manifester par une hémoptysie, qui peut mettre la vie en danger, d'où l'importance d'une recherche systématique d'une association. Une association confirmée change complètement le pronostic et l'approche thérapeutique.
Un patient de 62 ans, ancien fumeur à 40 paquets/an et consommateur chronique de cannabis, se présente depuis 6 mois avec une douleur thoracique gauche d’aggravation progressive, associée à une névralgie cervicobrachiale. L’évolution a été marquée par l’apparition d’une dyspnée d’effort un mois avant son admission, associée à un épisode isolé d’hémoptysie et à une perte de poids. À l’examen clinique, les résultats étaient normaux sur les plans thoracique, cardiovasculaire, abdominal et neurologique. La radiographie thoracique a révélé une masse dans la zone pulmonaire supérieure gauche. La tomodensitométrie a montré une masse excavée dans le segment postérieur du lobe supérieur gauche du poumon, mesurant 10 cm, avec des lésions nécrotiques.
L’aspergillome peut ressembler cliniquement et radiologiquement à un carcinome endobronchique. Le carcinome pulmonaire peut être masqué par une couverture de champignons et de fibrine.
MOTS CLÉS: Aspergillome; Endobronchique; Intracavitaire; Néoplasie bronchique.
INTRODUCTION
Aspergillosis is a mycotic disease usually caused by Aspergillus fumigatus, a saprophytic and ubiquitous airborne fungus responsible for human respiratory infections [1]. It rarely affects healthy people with an intact immune response, but those with preexisting structural lung disease, atopy, occupational exposure or impaired immunity are susceptible [2].
In this report, we describe a patient who presented with an aspergilloma arising in a cavitating squamous cell carcinoma of the right lung. The interest of our presentation is to raise the possibility that pulmonary neoplasia may be associated with pulmonary aspergillosis.
OBSERVATION
A 62-year-old male patient, former smoker at 40 packs/year and chronic cannabis user, presenting for 6 months with left chest pain of progressive aggravation associated with cervicobrachial neuralgia, The evolution was marked by the appearance of dyspnea on exertion 1 month before his admission associated with a single episode of hemoptysis and weight loss. On physical examination, he appeared with normal findings on chest, cardiovascular, abdominal and neurologic examinations. Chest radiography revealed a mass in the left upper lung zone, CT shows excavated mass in the posterior segment of the left upper lung lobe measuring 10 cm with necrotic lesions.
Flexible bronchoscopy showed a compression of the left main bronchus. Active pulmonary tuberculosis was ruled out after sputum and bronchial aspirations tests for BK came back negative.
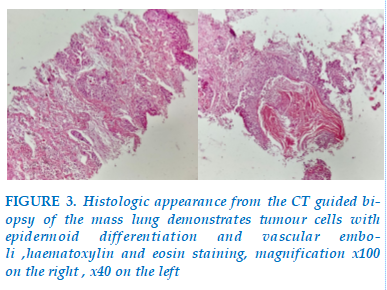
The aspergillus fumigatus serology came back positive and The CT guided biopsy of the mass reveled a squamous cell carcinoma of the lung. FIGURE 3.
DISCUSSION
Aspergillosis, caused predominantly by Aspergillus fumigatus, is the most frequent mould infection of the lungs. The spectrum of the disease is broad and depends on the immune status of the host [3]. Four distinctive patterns of Aspergillus-related lung diseases are recognized, as follows: saprophytic colonization, chronic pulmonary aspergillosis, hypersensitivity-induced aspergillosis, and invasive pulmonary aspergillosis [4].
Chronic pulmonary aspergillosis (CPA) affects individuals who are immunocompetent or mildly immunocompromised and have underlying lung disease, such as chronic obstructive pulmonary disease, sequelae of tuberculosis, nontuberculous mycobacterial infections or lung cancer [3].
The most common form of CPA is Chronic cavitary pulmonary aspergillosis (CCPA) formerly called complex aspergilloma, usually shows multiple cavities in association with pulmonary and systemic symptoms and raised inflammatory markers, over at least 3 months of observation [5]. Untreated, over years, these cavities enlarge and coalesce, developing pericavitary infiltrates or perforating into the pleura, and an aspergilloma may appear or disappear. Its usully localized in the upper lobe of the lung. Thus serological or microbiological evidence implicating Aspergillus is required for diagnosis [6] witch is consistent with our case.
Conditions associated with aspergilloma formation include tuberculosis, sarcoidosis, histoplasmosis, lung abscess, bronchiectasis, bullae, pulmonary infarcts, cystic fibrosis, HIV infection and cavitated squamous cell lung cancer like our case [2]. the most common preexisting condition was tuberculosis. Since then, the prevalence of pulmonary aspergilloma has declined [8]. In one study, the prevalence of Aspergillus growth in patients with bronchogenic carcinoma was reported as being 14.2% [9],4 but only a few cases of combined aspergilloma and lung cancer have been reported in the literature [10].
In this report, the aspergilloma occurred in a healthy man who had no known preexisting risk factors and had an unsuspected cavitary of squamous cell carcinoma, the diagnosis was suspected based on symptoms, radiological features, and the diagnosis was confirmed bay serology and the biopsy .
At present, there is no evidence of the efficacy of antifungal treatment, either systemically or by endobronchial or intracavitary instillation. Treatment abstention remains the rule for endocavitary aspergilloma, particularly in asymptomatic patients. However, surgery is the only curative treatment and is reserved for cases of massive hemoptysis in patients with adequate respiratory function [11]. In cases where aspergillosis is associated with bronchial carcinoma, management is completely different and requires a number of criteria to be taken into consideration, in particular the histological type of tumor, the tumor extension assessment, and the operability (of the tumor and the patient).
We propose that when aspergilloma is found in healthy persons with no risk factors, lung cancer must be ruled out and should be an another indication for surgical treatment of a fungus ball.
CONCLUSION
Aspergilloma can resemble to an endobronchial carcinoma clinically and radiologically. Lung carcinoma may be masked by a covering of fungus and fibrin. A systematic search for a concomitant neoplasia is imperative for any form of pulmonary aspergilloma because of the clinical and radiological similarity between these two diagnoses. Early identification of lung carcinoma is important in terms of management and prognosis.
CONFLICT OF INTEREST
Non.
REFERENCE
| 1. Goracci A, Chabi ML, Roche N, Paugam A, Mansuet Lupo A, Revel MP. L’aspergillose pulmonaire, ce que le radiologue doit savoir. Accessed on 17 May 2017. |
| 2. Bardana EJ. Pulmonary aspergillosis. In: Al-Doory Y, Wagner GE, editors. Aspergillosis. Springfield (IL): Charles C Thomas; 1985. p. 43-78. |
| 3. Lamoth F, Calandra T. Pulmonary aspergillosis: diagnosis and treatment. Eur Respir Rev 2022; 31: 220114 |
| 4. Al-Alawi A, Rayan CF, Flint JD, et al. Aspergillus-related lung disease. Can Respir J 2005;12:377-87. |
| 5. Denning DW, Riniotis K, Dobrashian R, et al. Chronic cavitary and fibrosing pulmonary and pleural aspergillosis: case series, proposed nomenclature change, and review. Clin Infect Dis 2003; 37: Suppl. 3, S265–S280 |
| 6. Chronic pulmonary aspergillosis: rationale and clinical guidelines for diagnosis and management David W. Denning, Jacques Cadranel, Catherine Beigelman-Aubry, Florence Ader, Arunaloke Chakrabarti, Stijn Blot, Andrew J. Ullmann, George Dimopoulos, Christoph Lange European Respiratory Journal 2016 47: 45-68 |
| 7. Mahboub F, Jabri H, Elkhattabi W, Mobachir H, Afif H. Serologie aspergillaire et diagnostic des aspergillomes pulmonaires. Revue des Maladies Respiratoires. 2016 Jan;33(Suppl):A231–A232 |
| 8. Babatasi G, Massetti M, Chapelier A, et al. Surgical treatment of pulmonary aspergilloma: current outcome. J Thorac Cardiovasc Surg 2000;119:906-12 |
| 9. Malik A, Shahid M, Bhagava R. Prevalence of aspergillosis in bronchogenic carcinoma. Indian J Pathol Microbiol 2003;46:507-10 |
| 10. Tomioka H, Iwasaki H, Okumura N, et al. Undiagnosed lung cancer complicated by intracavitary aspergillosis [abstract]. Nihon Kokyuki Gakkai Zasshi 1999;37:78-82. |
| 11. David G, Blandin S. L’aspergillose en pratique pour le pneumologue. Revue de la pneumologie Clinique. 2008 Aug;64(4):202–10. Epub 2008 Sep 19 |
TABLE - FIGURES
REFERENCE
| 1. Goracci A, Chabi ML, Roche N, Paugam A, Mansuet Lupo A, Revel MP. L’aspergillose pulmonaire, ce que le radiologue doit savoir. Accessed on 17 May 2017. |
| 2. Bardana EJ. Pulmonary aspergillosis. In: Al-Doory Y, Wagner GE, editors. Aspergillosis. Springfield (IL): Charles C Thomas; 1985. p. 43-78. |
| 3. Lamoth F, Calandra T. Pulmonary aspergillosis: diagnosis and treatment. Eur Respir Rev 2022; 31: 220114 |
| 4. Al-Alawi A, Rayan CF, Flint JD, et al. Aspergillus-related lung disease. Can Respir J 2005;12:377-87. |
| 5. Denning DW, Riniotis K, Dobrashian R, et al. Chronic cavitary and fibrosing pulmonary and pleural aspergillosis: case series, proposed nomenclature change, and review. Clin Infect Dis 2003; 37: Suppl. 3, S265–S280 |
| 6. Chronic pulmonary aspergillosis: rationale and clinical guidelines for diagnosis and management David W. Denning, Jacques Cadranel, Catherine Beigelman-Aubry, Florence Ader, Arunaloke Chakrabarti, Stijn Blot, Andrew J. Ullmann, George Dimopoulos, Christoph Lange European Respiratory Journal 2016 47: 45-68 |
| 7. Mahboub F, Jabri H, Elkhattabi W, Mobachir H, Afif H. Serologie aspergillaire et diagnostic des aspergillomes pulmonaires. Revue des Maladies Respiratoires. 2016 Jan;33(Suppl):A231–A232 |
| 8. Babatasi G, Massetti M, Chapelier A, et al. Surgical treatment of pulmonary aspergilloma: current outcome. J Thorac Cardiovasc Surg 2000;119:906-12 |
| 9. Malik A, Shahid M, Bhagava R. Prevalence of aspergillosis in bronchogenic carcinoma. Indian J Pathol Microbiol 2003;46:507-10 |
| 10. Tomioka H, Iwasaki H, Okumura N, et al. Undiagnosed lung cancer complicated by intracavitary aspergillosis [abstract]. Nihon Kokyuki Gakkai Zasshi 1999;37:78-82. |
| 11. David G, Blandin S. L’aspergillose en pratique pour le pneumologue. Revue de la pneumologie Clinique. 2008 Aug;64(4):202–10. Epub 2008 Sep 19 |
ARTICLE INFO DOI: 10.12699/jfvpulm.15.47.2024.59
Conflict of Interest
Non
Date of manuscript receiving
20/06/2024
Date of publication after correction
28/11/2024
Article citation
Biborchi, H. Naguyeh, H. Yassine, M. Ijim, O. Fikri, L. Amro. Patient presenting aspergilloma in combination with squamous cell carcinoma of the lung. J Func Vent Pulm 2024;47(15):59-61